This document discusses the history and development of the Ilizarov fixator for limb lengthening. Some key points:
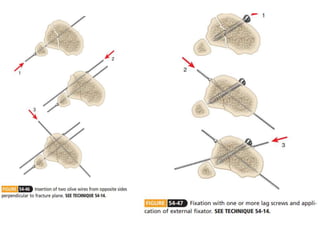
- Previous methods from the 1940s-1960s by Anderson and Wagner were crude, requiring multiple invasive surgeries and resulting in many complications.
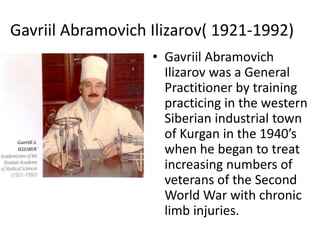
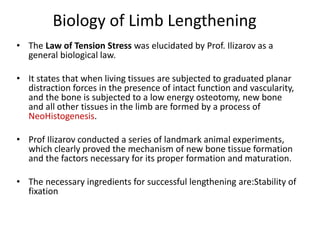
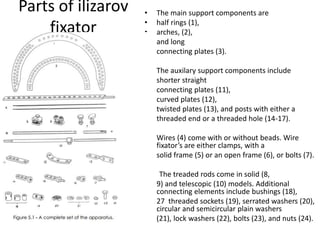
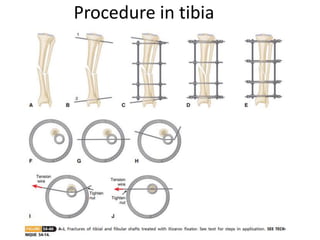
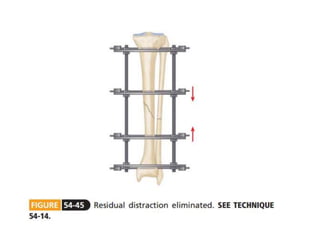
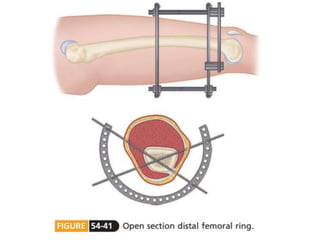
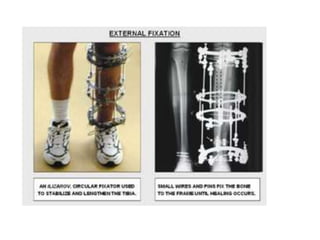
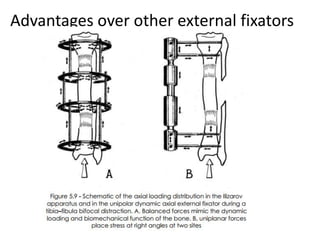
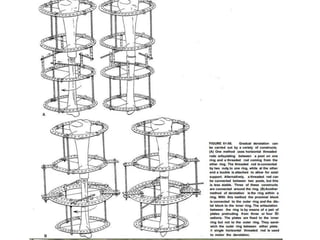
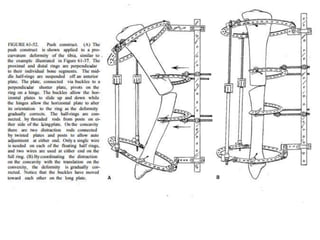
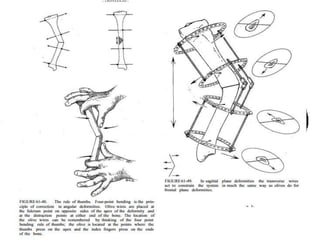
- Soviet physician Gavriil Ilizarov in the 1940s-50s pioneered a circular external fixator made of thin wires that could gradually and safely lengthen limbs using the body's natural bone regeneration, establishing the biological principles still used today.
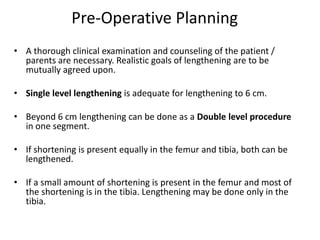
- His method reduced complications and made limb lengthening a reliable procedure to treat many causes of limb length discrepancies and shortening.