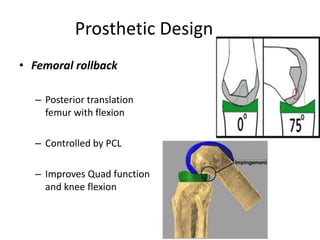
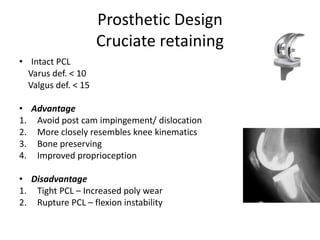
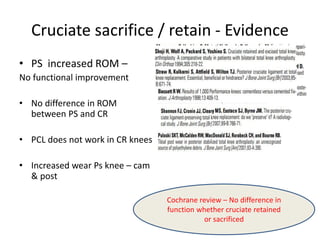
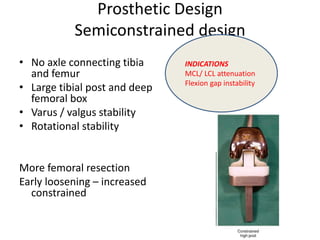
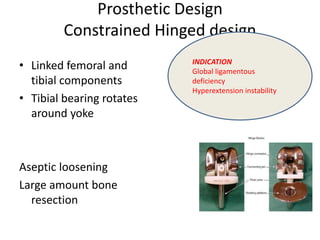
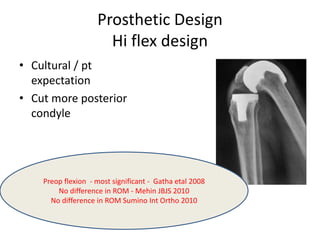
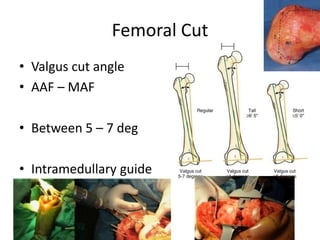
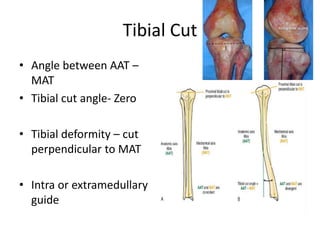
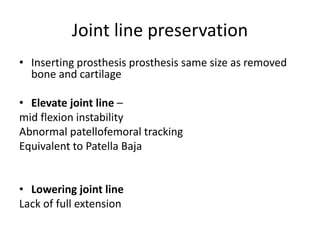
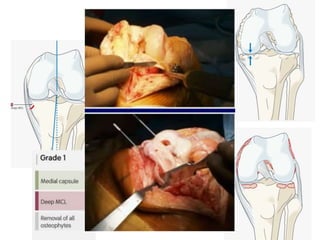
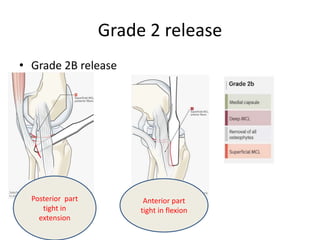
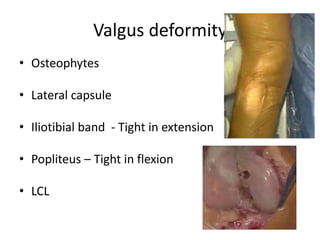
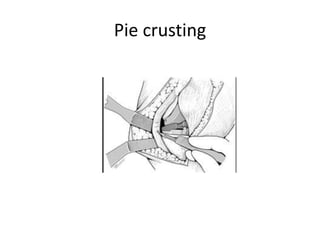
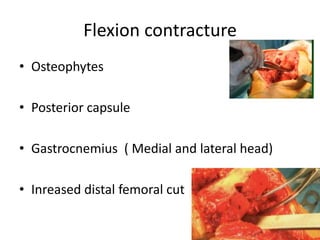
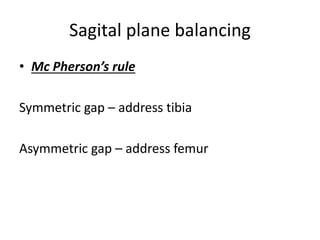
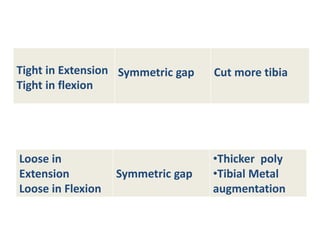
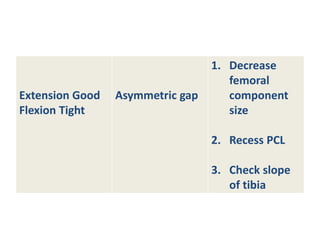
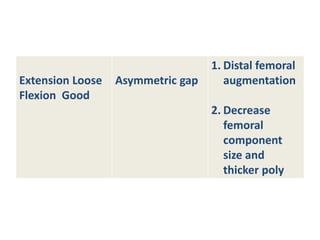
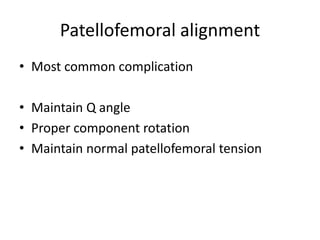
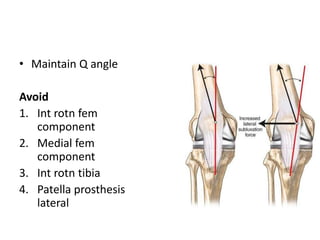
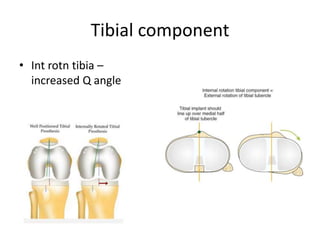
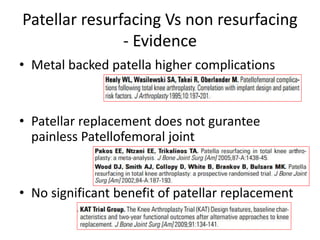
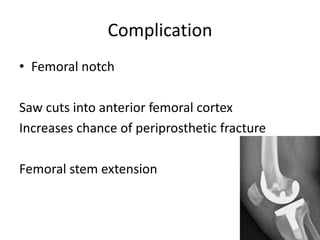
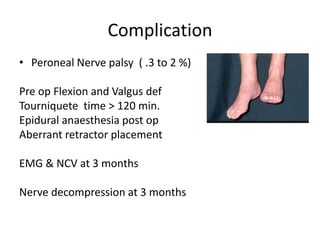
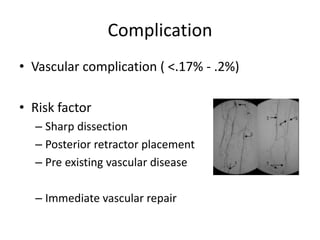
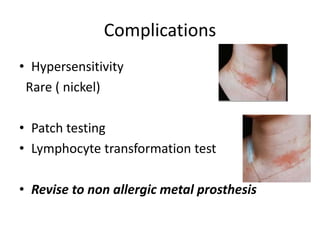
Primary Total Knee Arthroplasty has evolved since the 19th century with various prosthetic designs introduced over time. Prosthetic design considerations include femoral rollback, modularity, constraint, and whether to retain or sacrifice the cruciate ligaments. Radiographs are important for preoperative planning to assess alignment and bone defects. Surgical goals include restoring mechanical alignment, joint line, balanced soft tissues, and normal patellofemoral tracking. Key steps include femoral and tibial cuts, balancing the knee in flexion and extension, and addressing any flexion contractures or deformities. Complications can include nerve palsies, vascular issues, stiffness, infections, and loosening. With careful patient selection, planning and technique, total knee