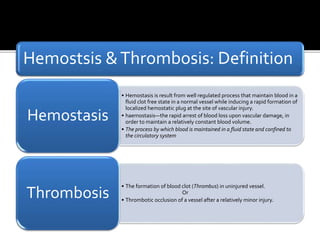
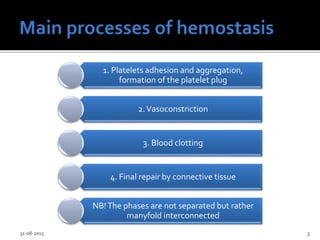
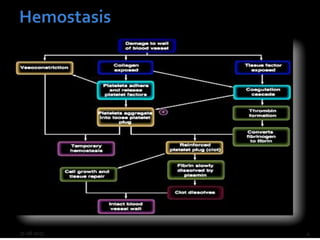
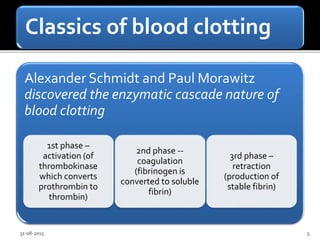
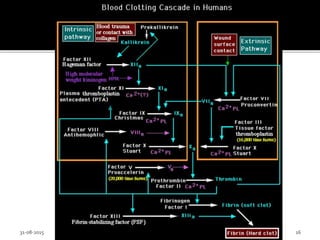
Hemostasis is the process by which blood is maintained in a fluid state within blood vessels and a clot is formed at the site of injury to stop bleeding. It involves platelet adhesion and aggregation to form a platelet plug, vasoconstriction, and the blood clotting cascade. Thrombosis is the formation of a blood clot within an uninjured blood vessel. The endothelium regulates hemostasis by producing anticoagulant and profibrinolytic factors but can also express procoagulant factors like tissue factor under certain conditions. A balance of pro- and anti-coagulant factors is needed to maintain normal hemostasis.