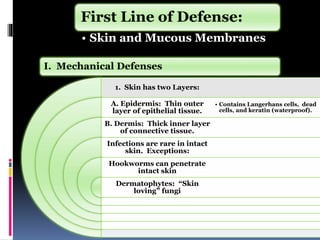
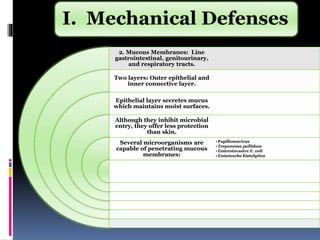
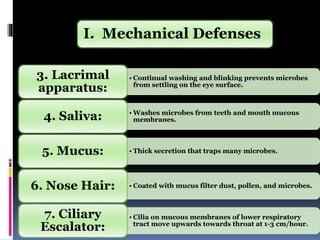
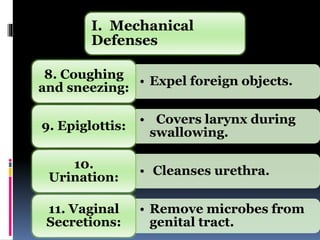
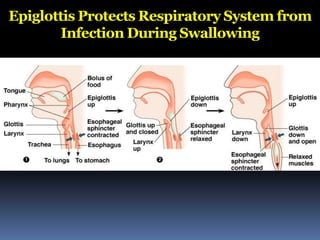
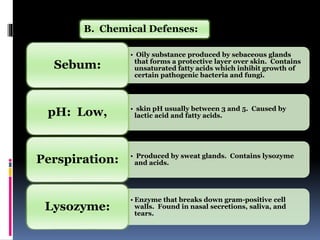
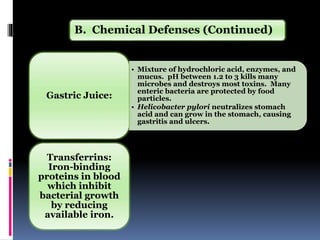
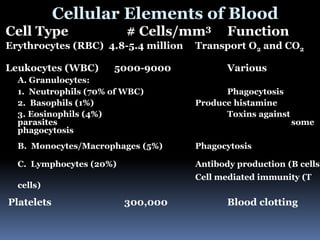
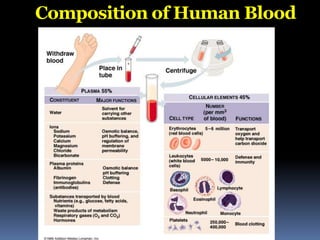
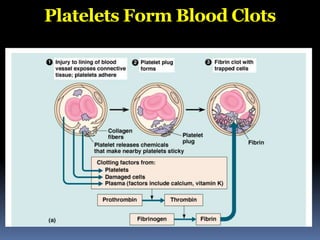
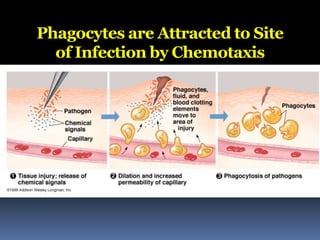
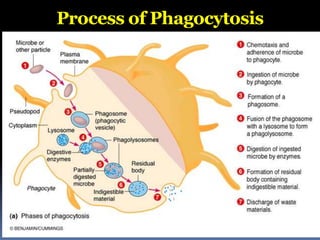
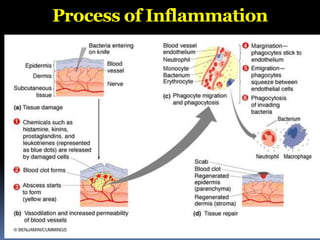
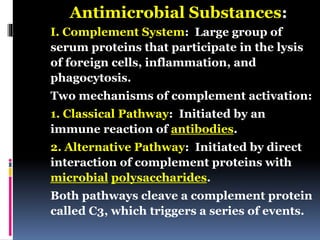
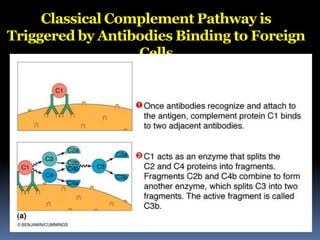
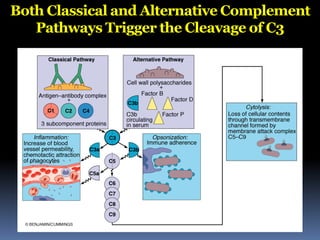
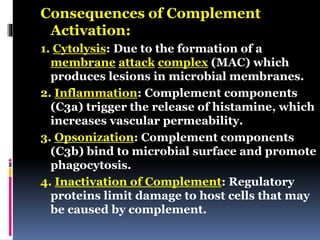
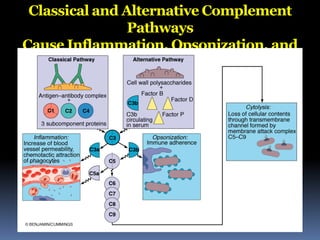
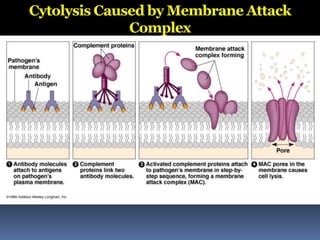
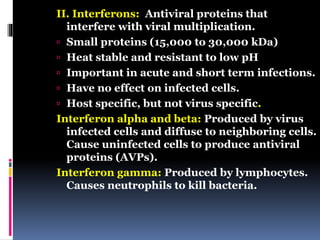
The document discusses the immune system's responses, categorizing them into nonspecific and specific defenses against pathogens. Nonspecific defenses include physical barriers like skin and mucous membranes, as well as inflammatory responses, while specific defenses involve targeted actions by antibodies and lymphocytes. It also details the mechanisms of phagocytosis, inflammation, and humoral responses through various immune components.