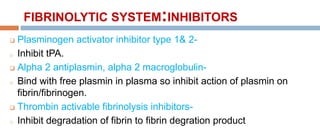
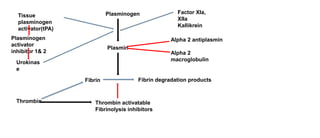
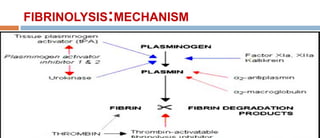
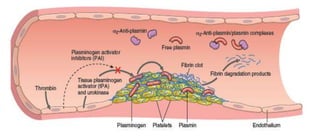
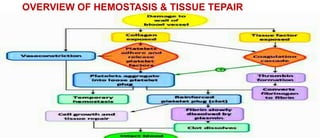
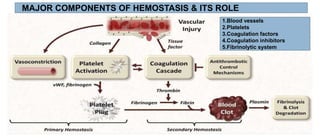
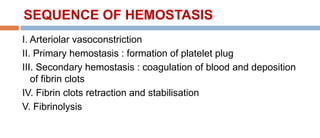
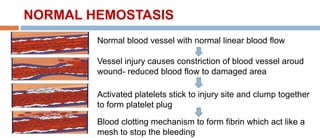
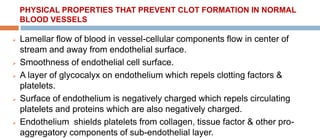
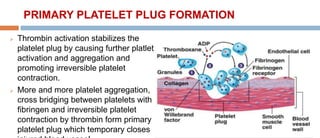
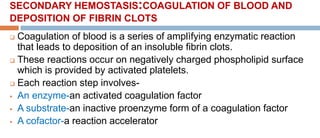
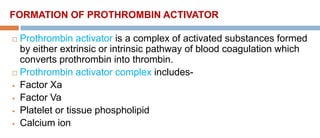
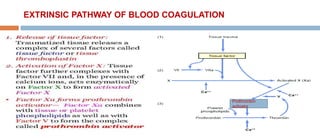
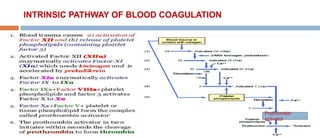
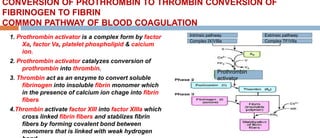
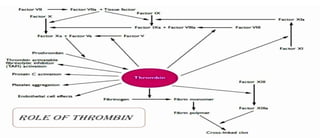
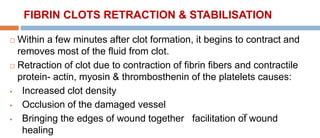
The document discusses normal hemostasis, a physiological process that prevents blood loss while maintaining blood fluidity through a cascade involving blood vessels, platelets, coagulation factors, and inhibitors. It details the sequence of hemostatic events, including vasoconstriction, platelet plug formation, and blood coagulation, highlighting the roles of various components in preventing excessive bleeding and facilitating tissue repair. Additionally, it introduces the fibrinolytic system responsible for the dissolution of blood clots and the mechanisms that regulate these processes.
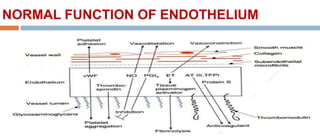
![SUBSTANCES RELEASED FROM OR FOUND ON THE SURFACE OF
ENDOTHELIAL CELLS PREVENT CLOT FORMATION IN NORMAL
BLOOD VESSEL
Prostaglandin I2[PGI2]- produced from endothelium-prevents platelets
aggregation and its activation.
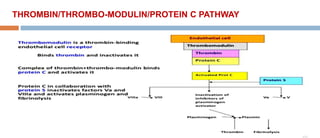
Thrombomodulin- expressed on surface of endothelial cells-binds with
thrombin & modulates function of thrombin- activates Protein C –causes
inactivation of coagulation factor F Va & F VIIIa.
Heparan sulfate- on surface of endothelium-binds & activates Antithrombin
III- inhibits thrombin & coagulation factor IXa, Xa, XIa & XIIa.](https://image.slidesharecdn.com/normalhemostasis-3-230314071434-6bea4f8c/85/NORMAL-HEMOSTASIS-9-320.jpg)
![ Tissue plasminogen activator[tPA]- released from endothelium-
activates plasminogen to plasmin which breaks down abnormaly
formed fibrin into fibrin degradation product.
Prostacyclin & Nitric oxide-inhibits platelet adhesion &
aggregation, promotes vasodilation.
ATPase & ADPase-ATP & ADP produced by platelets are
inactivated.
Tissue factor pathway inhibitors[TFPI]-binds and inhibits TF-F
VIIa complex](https://image.slidesharecdn.com/normalhemostasis-3-230314071434-6bea4f8c/85/NORMAL-HEMOSTASIS-10-320.jpg)

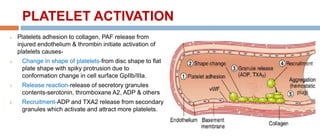

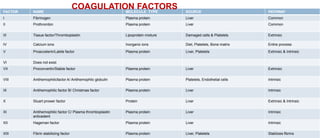
![COAGULATION FACTORS
Normally coagulation factors are circulating in the blood in an inactive
form.
All coagulation factors are protein except tissue factor[thromboplastin] &
calcium.
Most of coagulation factors are synthesised by liver except tissue factor
and calcium.
Tissue factor synthesised by various tissues and calcium from bones
and diet.
F V & F XIII synthesised by platelets in addition to liver.](https://image.slidesharecdn.com/normalhemostasis-3-230314071434-6bea4f8c/85/NORMAL-HEMOSTASIS-30-320.jpg)
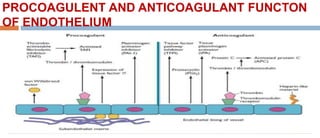
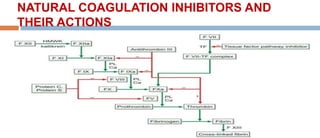
![COAGULATION INHIBITORS
Tissue factor pathway inhibitor[TFPI]-
o Release from endothelium of blood vessel.
o Inhibit TF-F VIIa complex- inhibit coagulation.
Antithrombin III[AT III]-
o Synthesises in liver.
o Inhibit Thrombin[F IIa], Factor IXa, Xa, Xia, XIIa.
Protein C & S-
o Protein C is activated by thrombin in presence of thrombomodulin on surface of
endothelium causes proteolysis of F Va, F VIIIa.
o Protein S act as a cofactor & inhance activity of protein C.](https://image.slidesharecdn.com/normalhemostasis-3-230314071434-6bea4f8c/85/NORMAL-HEMOSTASIS-51-320.jpg)

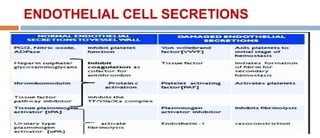
![FIBRINOLYTIC SYSTEM:ACTIVATOR
Tissue plasminogen activator[tPA]-
Secreted by endothelial cells.
Activates Plasminogen to Plasmin.
Urokinase-
Produced by kidney.
Activates plasminogen to plasmin.
Plasmin-
Degraded fibrinogen/fibrin into fibrinogen/fibrin degration
product[FDPs].](https://image.slidesharecdn.com/normalhemostasis-3-230314071434-6bea4f8c/85/NORMAL-HEMOSTASIS-56-320.jpg)