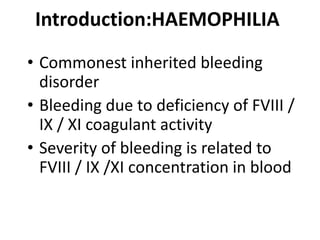
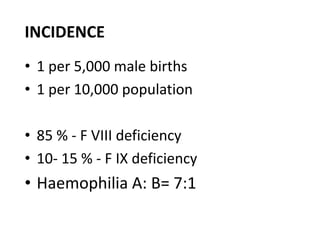
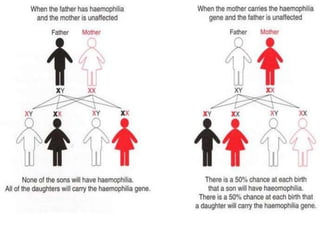
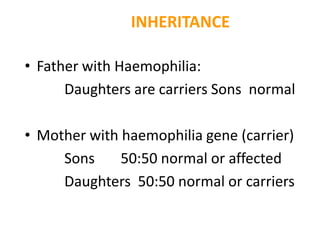
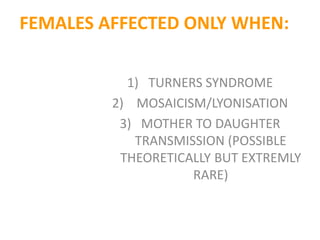
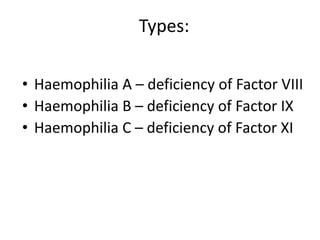
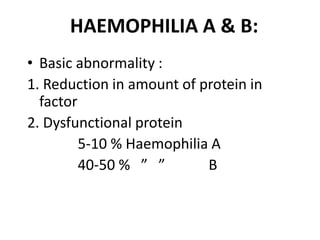
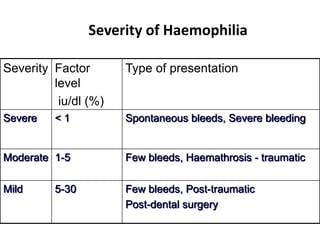
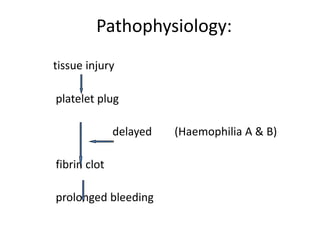
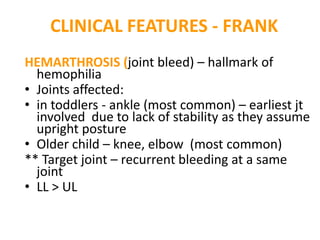
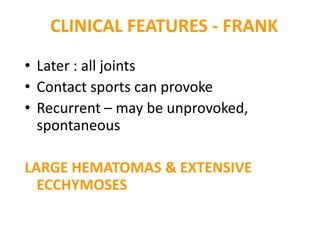
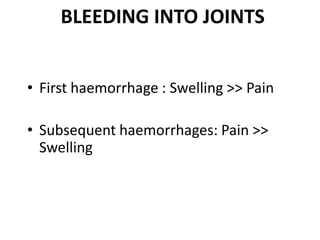
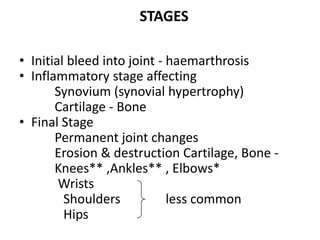
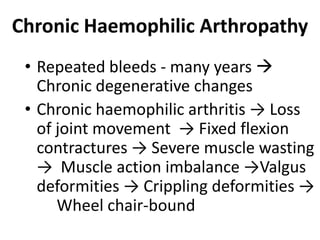
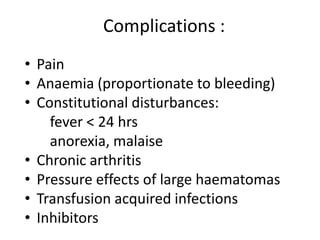
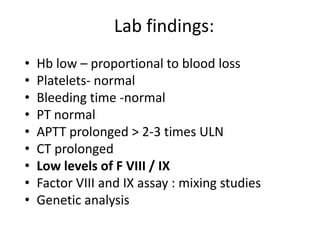
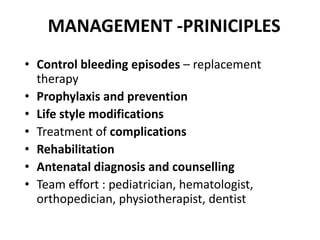
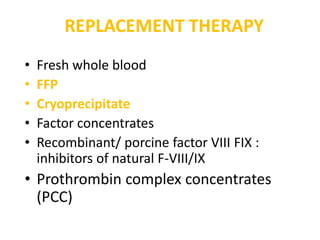
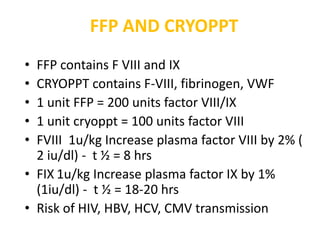
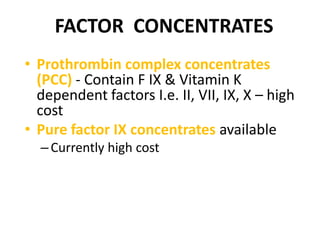
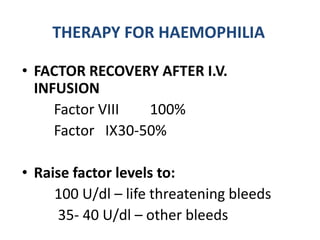
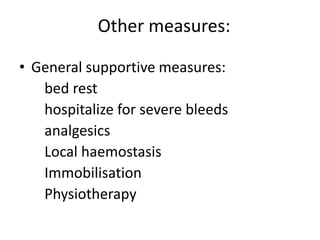
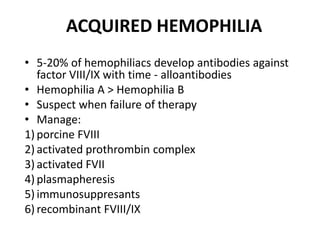
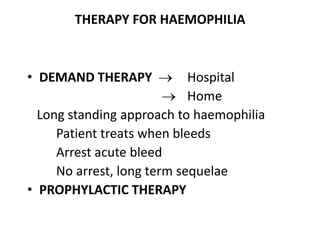
Hemophilia is a genetic bleeding disorder caused by deficiencies in clotting factors VIII or IX. It is inherited in an X-linked recessive pattern and primarily affects males. Symptoms range from easy bruising to spontaneous internal bleeding that can be life-threatening. Treatment involves replacement of the missing clotting factor through infusions to prevent or treat bleeding episodes. Repeated bleeding can lead to chronic joint damage over time without proper management.
![Hemophilia
Dr. Kalpana Malla
MD Pediatrics
Manipal Teaching Hospital
Download more documents and slide shows on The Medical Post [ www.themedicalpost.net ]](https://image.slidesharecdn.com/hematology-hemophilia-120108093052-phpapp02/75/Hemophilia-1-2048.jpg)
![Thank you
Download more documents and slide shows on The
Medical Post [ www.themedicalpost.net ]](https://image.slidesharecdn.com/hematology-hemophilia-120108093052-phpapp02/85/Hemophilia-59-320.jpg)