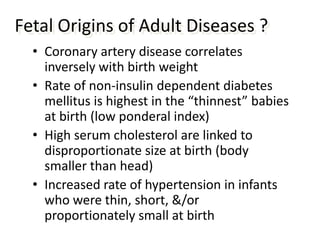
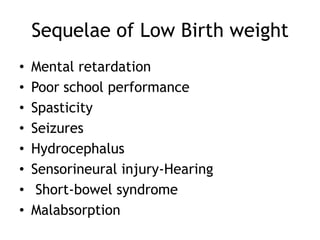
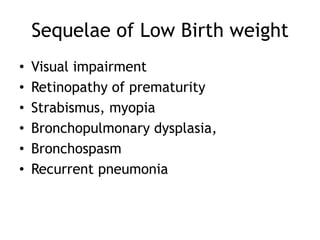
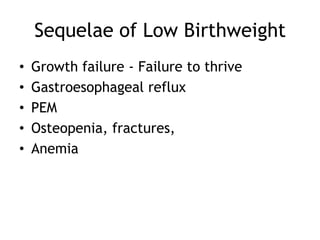
This document discusses prematurity, intrauterine growth restriction (IUGR), and their associated risks and management. It covers:
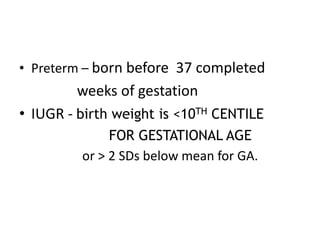
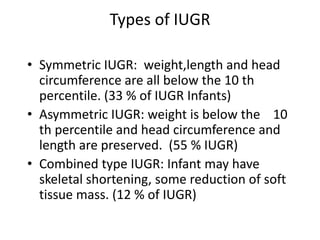
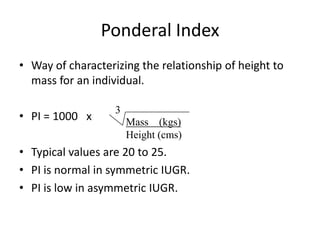
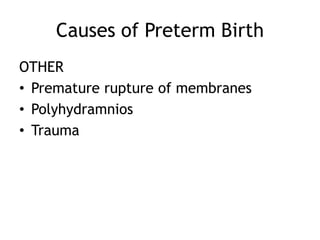
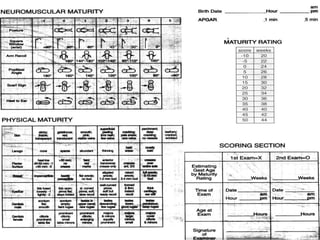
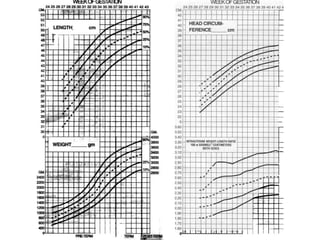
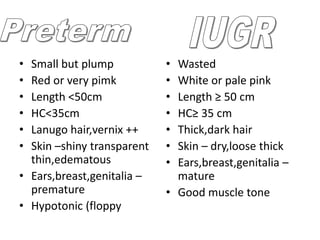
- Definitions and types of prematurity and IUGR
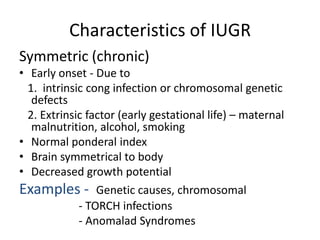
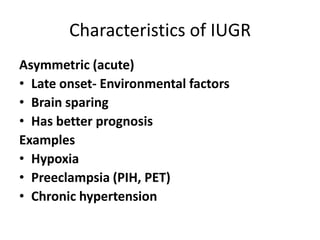
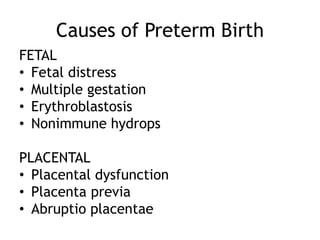
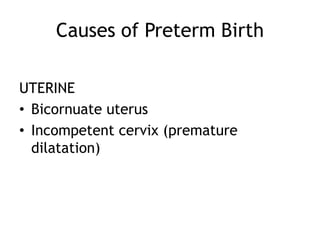
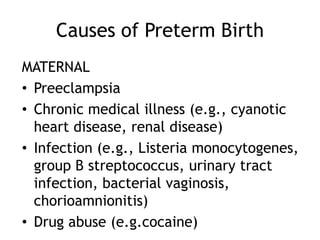
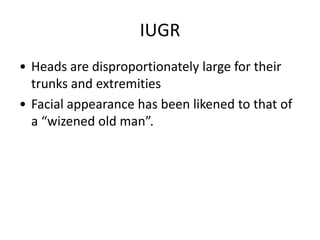
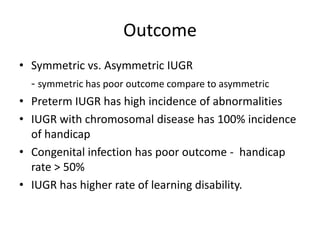
- Characteristics and causes of symmetric vs asymmetric IUGR
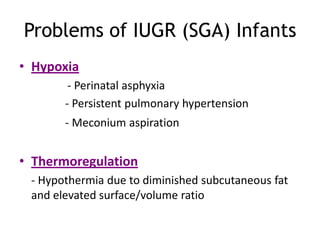
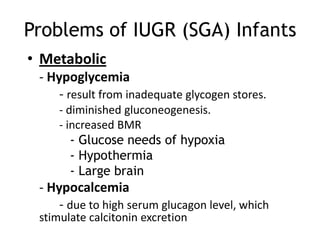
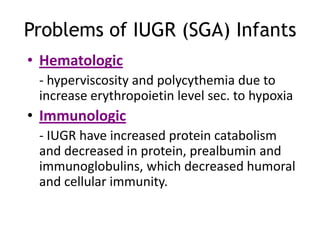
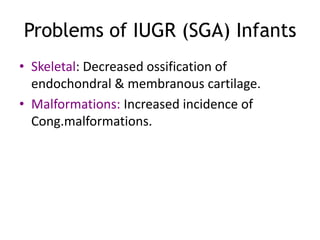
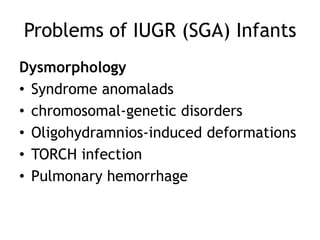
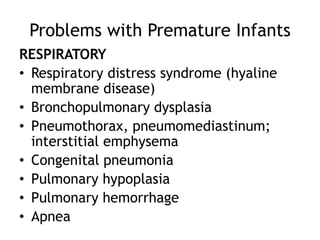
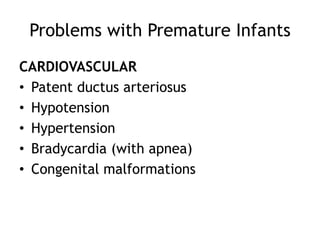
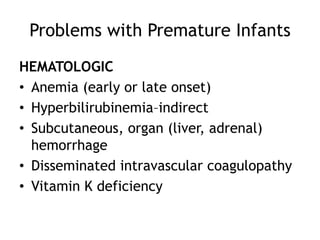
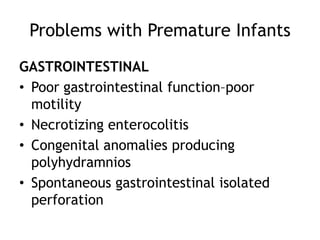
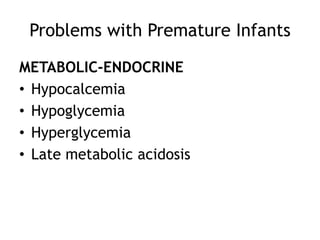
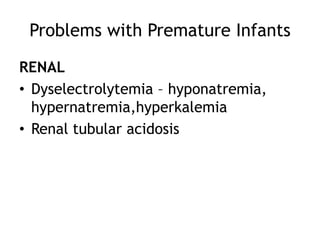
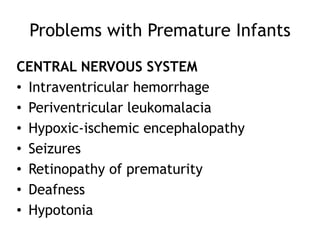
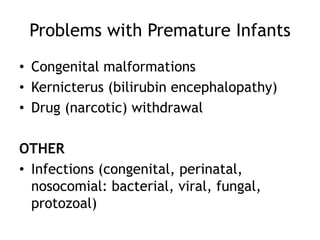
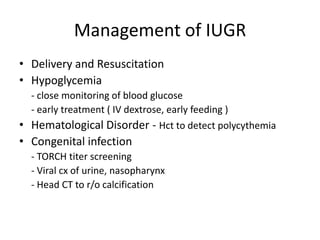
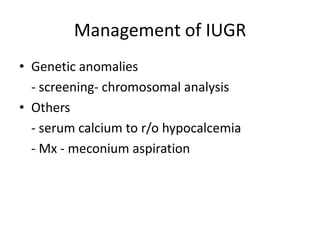
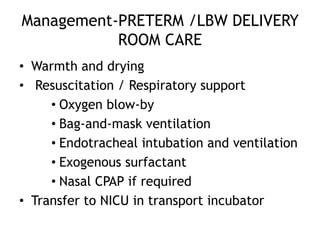
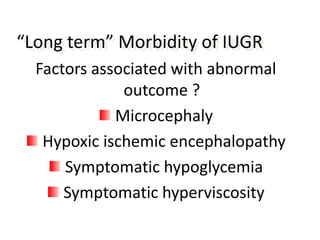
- Problems that can occur in IUGR and premature infants like respiratory distress, hypoglycemia, and intraventricular hemorrhage
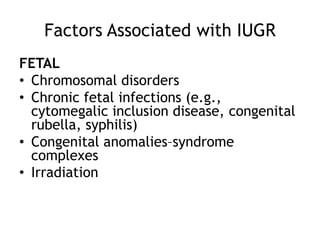
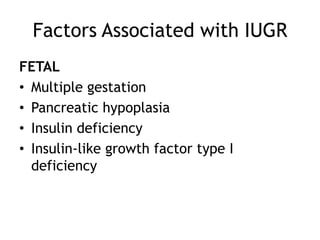
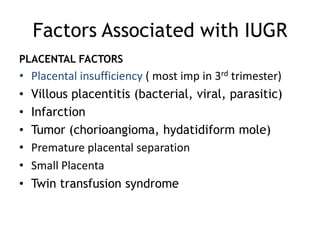
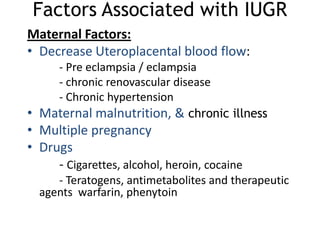
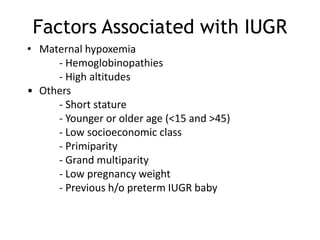
- Factors associated with IUGR including placental and maternal factors
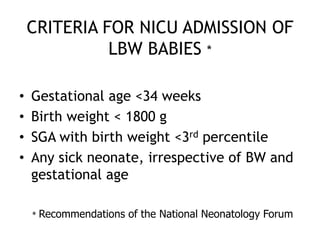
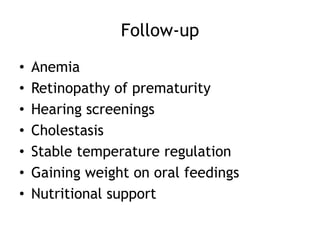
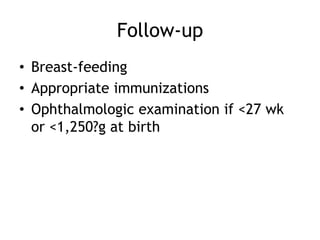
- Guidelines for admission to the neonatal intensive care unit (NICU)
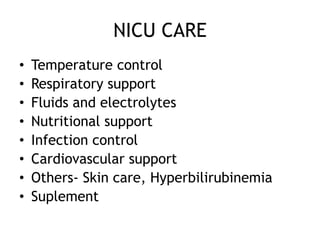
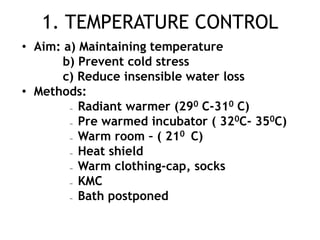
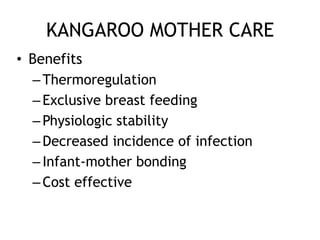
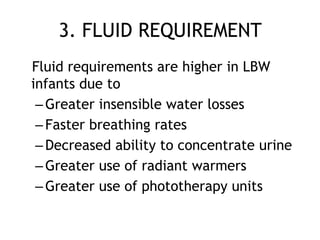
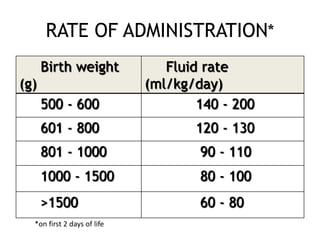
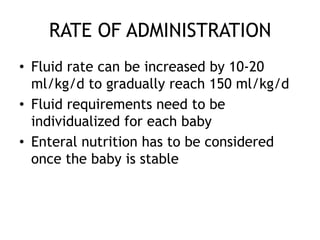
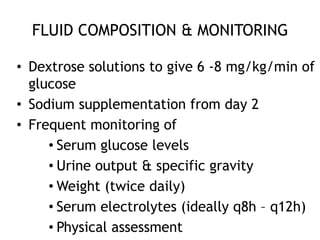
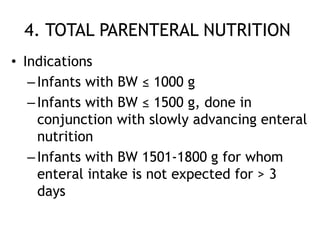
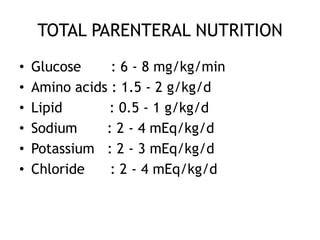
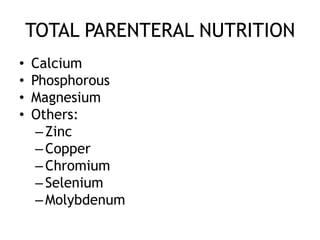
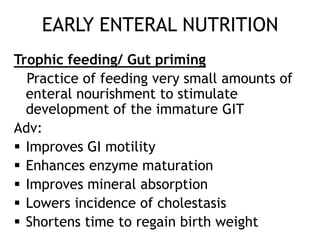
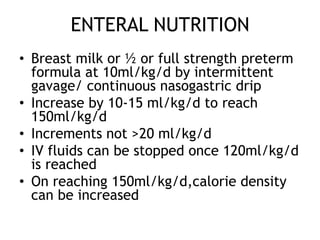
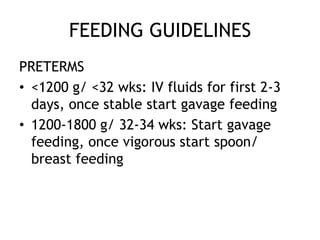
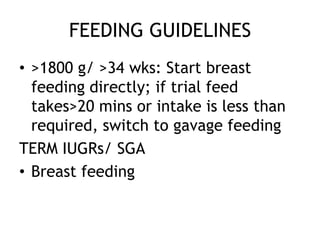
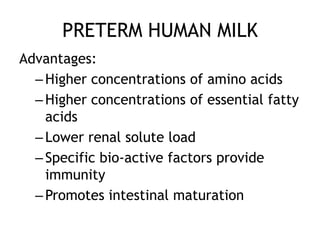
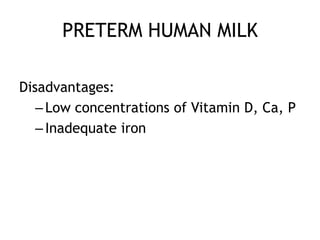
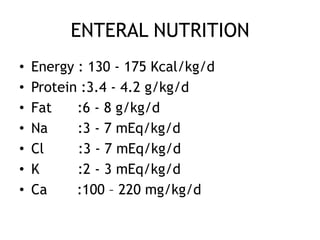
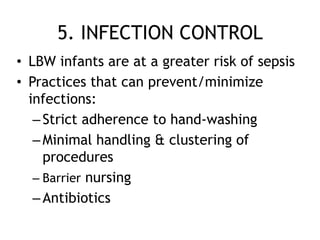
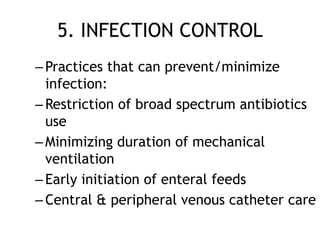
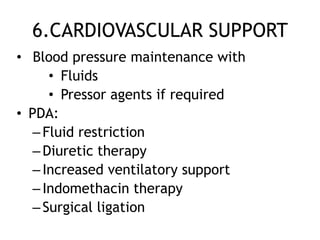
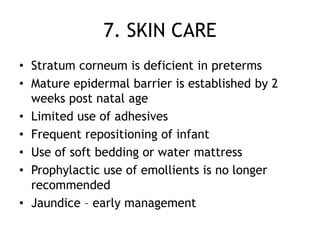
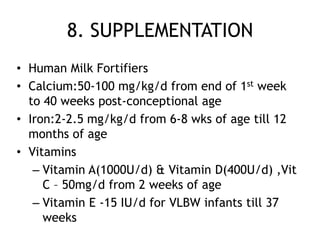
- Important aspects of care in the NICU like temperature control, respiratory support, fluid management, and infection control
![Prematurity and IUGR
Dr. Kalpana Malla
MD Pediatrics
Manipal Teaching Hospital
Download more documents and slide shows on The Medical Post [ www.themedicalpost.net ]](https://image.slidesharecdn.com/newborn-prematurityandiugr-120107084441-phpapp01/75/Prematurity-and-IUGR-1-2048.jpg)

![Thank you
Download more documents and slide shows on The
Medical Post [ www.themedicalpost.net ]](https://image.slidesharecdn.com/newborn-prematurityandiugr-120107084441-phpapp01/85/Prematurity-and-IUGR-69-320.jpg)