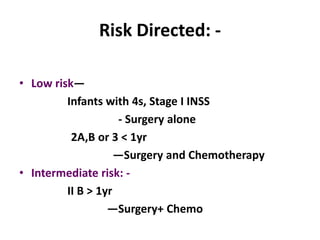
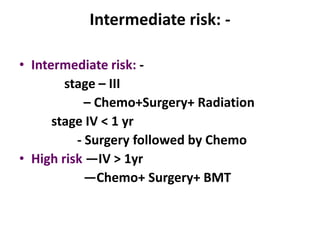
This document discusses neuroblastoma and nephroblastoma. [1] Neuroblastoma is the most common extracranial tumor in children and accounts for 8% of childhood cancers. It commonly presents before age 5 and can secrete catecholamines. [2] Nephroblastoma, also known as Wilm's tumor, is the most common renal tumor in children. It typically presents before age 3 as an abdominal mass. Staging and treatment involve surgery with or without chemotherapy and radiation depending on risk factors. Both tumors can metastasize but have better prognosis when caught early.
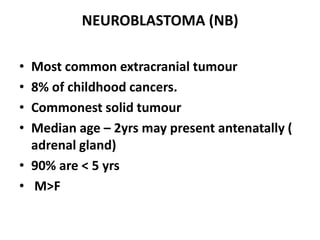
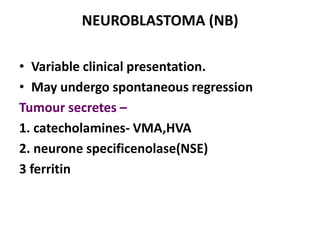
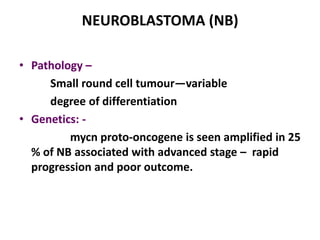
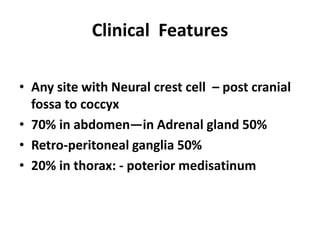
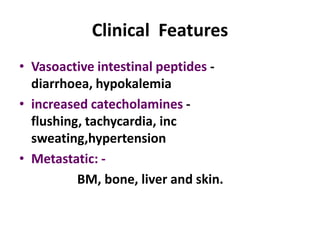
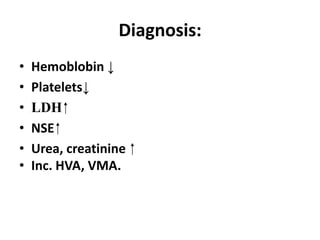
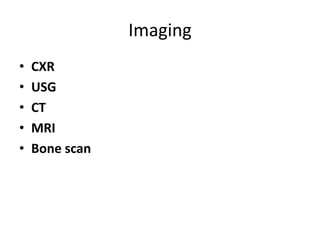
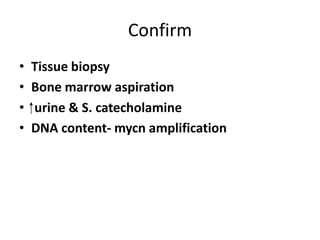
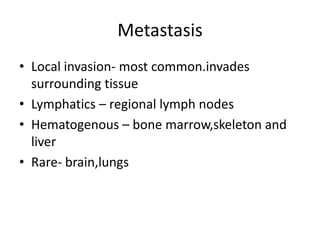
![Neuroblastoma and
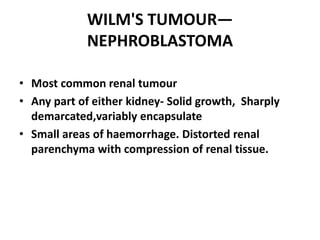
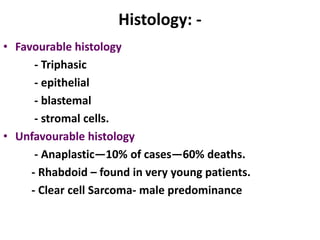
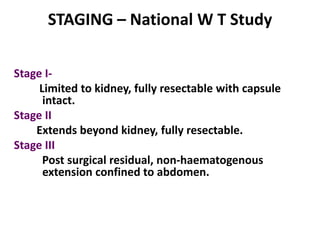
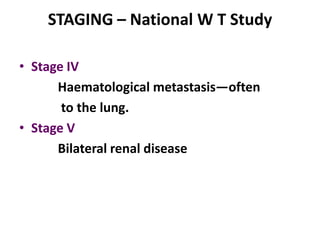
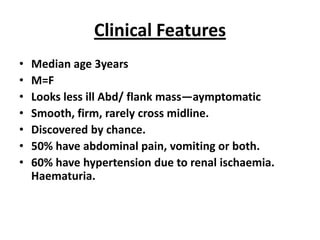
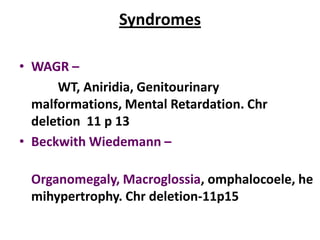
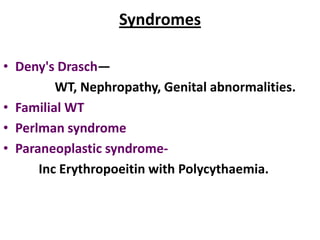
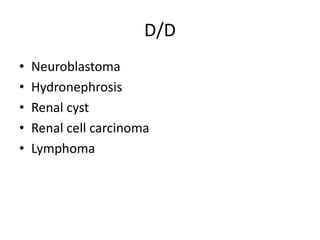
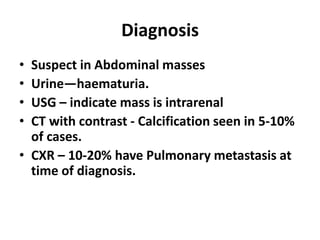
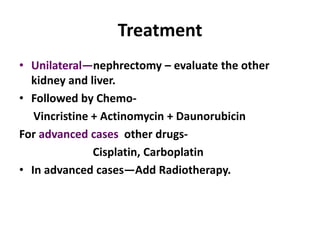
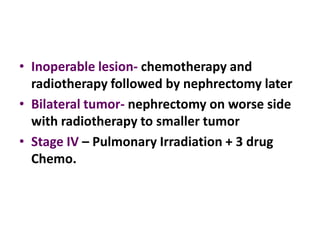
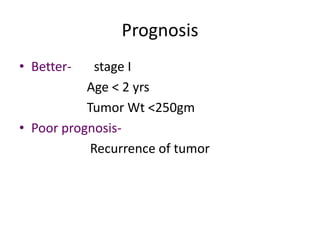
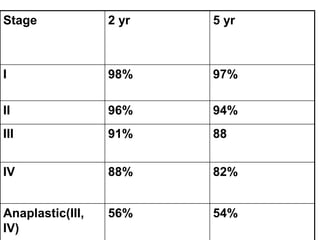
Nephroblastoma
Dr. Kalpana Malla
MD Pediatrics
Manipal Teaching Hospital
Download more documents and slide shows on The Medical Post [ www.themedicalpost.net ]](https://image.slidesharecdn.com/newborn-neuroandnephroblastoma-120107084301-phpapp02/75/Neuroblastoma-and-Nephroblastoma-1-2048.jpg)

![Thank you
Download more documents and slide shows on The
Medical Post [ www.themedicalpost.net ]](https://image.slidesharecdn.com/newborn-neuroandnephroblastoma-120107084301-phpapp02/85/Neuroblastoma-and-Nephroblastoma-35-320.jpg)