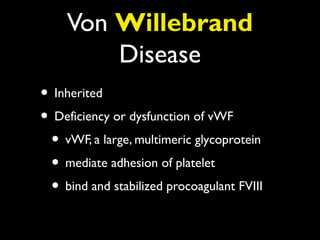
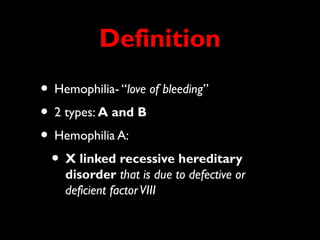
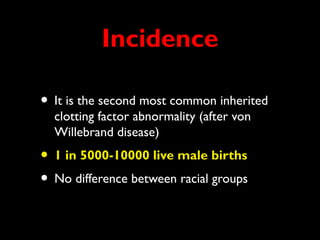
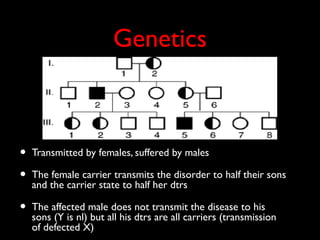
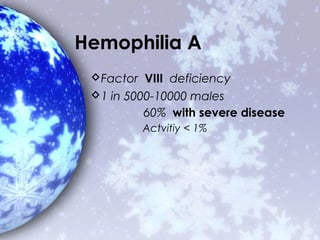
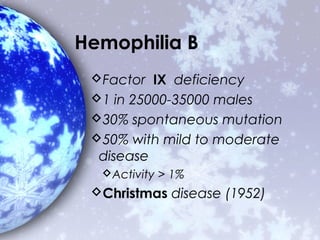
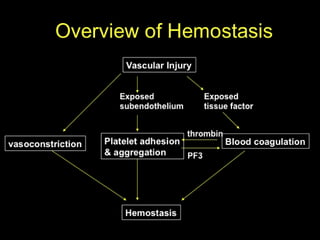
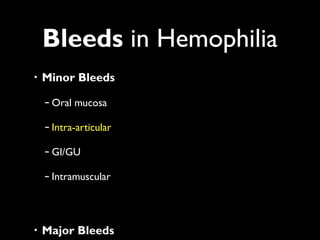
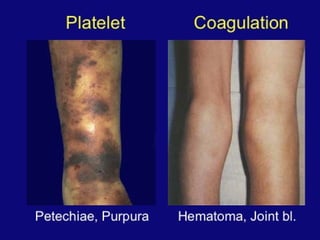
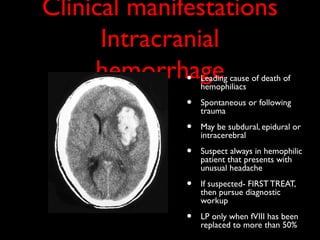
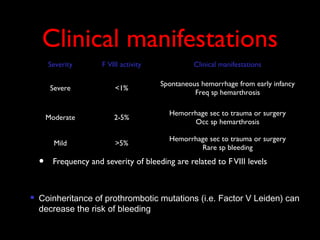
Hemophilia A and B are X-linked bleeding disorders caused by deficiencies of coagulation factors VIII and IX respectively. Hemophilia A is more common, affecting about 1 in 5,000-10,000 live male births. The disorders are inherited but only affect males, with female carriers able to pass the gene to their sons or daughters. Common clinical manifestations include hemarthrosis, hematomas, and intracranial bleeding. Treatment involves replacement of the missing coagulation factor, initially through plasma-derived or recombinant products, with the goal of preventing bleeds or treating acute bleeds.


![Treatment: The Old Days
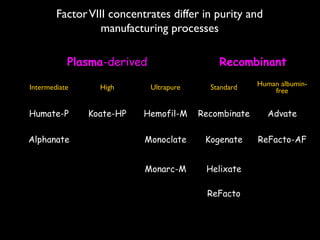
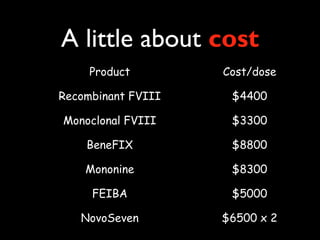
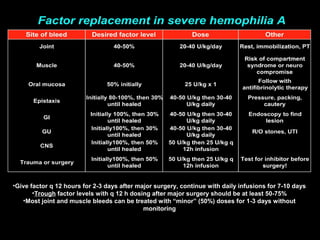
Factor replacement
Units = (wt[kg]) x (50mL plasma/kg) x (1 U factor/mL plasma) x
(desired factor level – native factor level)
FFP: 10-20 mL/kg BB will increase factor level 20-30%
Number of unit : desire dose (mL)/200 mL/unit
Plasma concentrates
Thousands of donors
Hepatitis B, C
HIV (60-70%)](https://image.slidesharecdn.com/hemophilia-130127161535-phpapp01/85/Hemophilia-32-320.jpg)