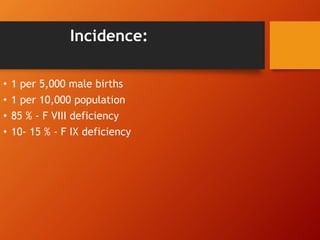
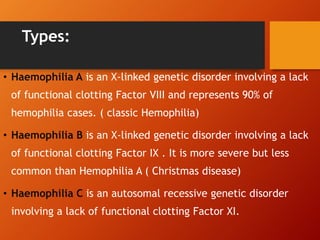
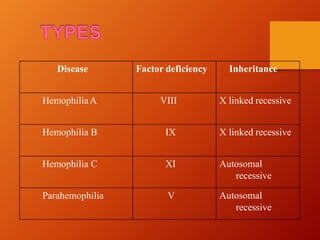
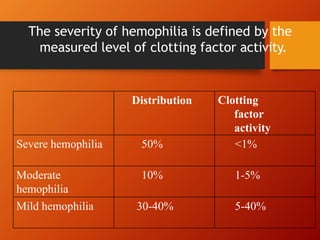
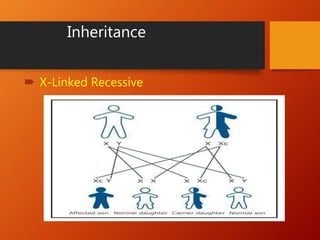
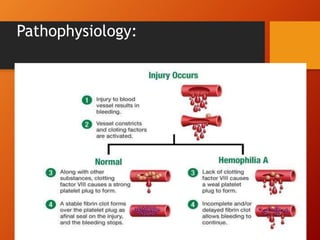
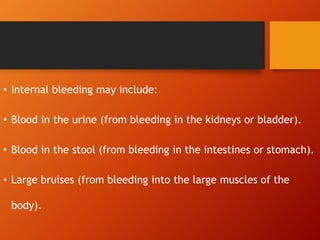
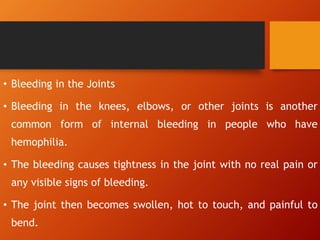
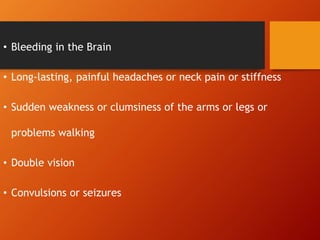
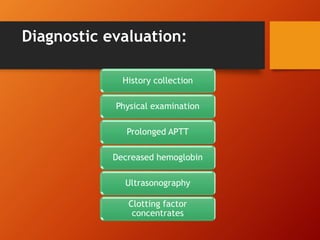
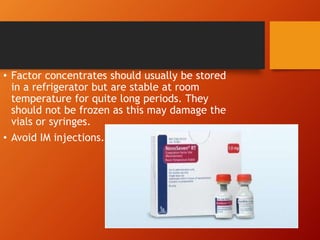
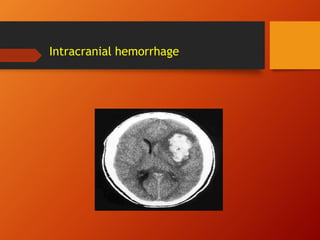
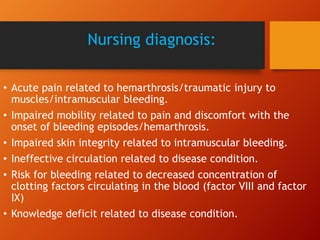
Hemophilia is a genetic bleeding disorder caused by deficiencies in clotting factors VIII or IX. The main symptoms are prolonged bleeding after injury or surgery and bleeding into joints or muscles. There are three main types - A, B, and C - defined by which clotting factor is deficient. Treatment involves replacing the missing clotting factor through infusions of plasma-derived or recombinant factor concentrates. Management also focuses on preventing bleeding episodes and complications through measures like RICE, immobilization, exercise, and infection control.