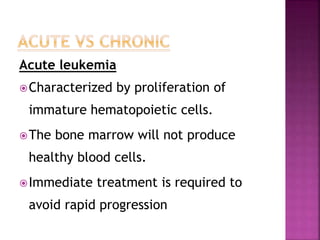
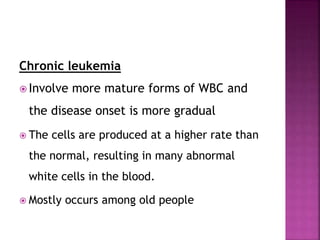
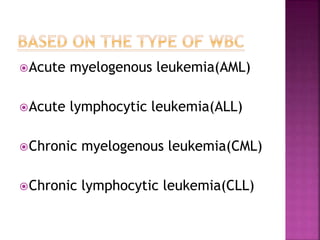
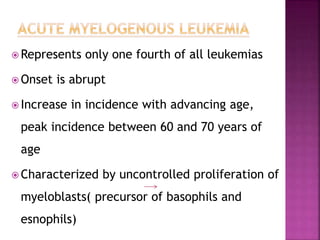
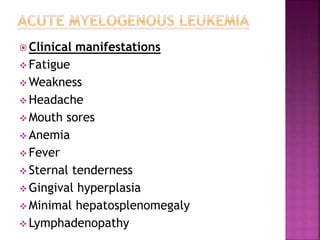
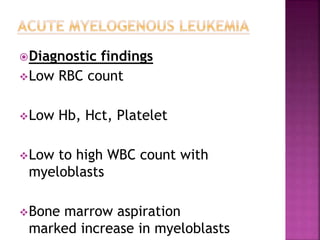
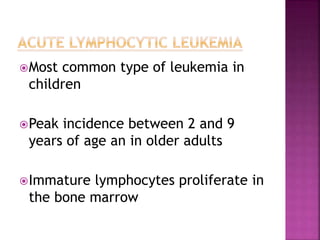
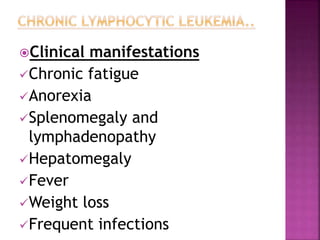
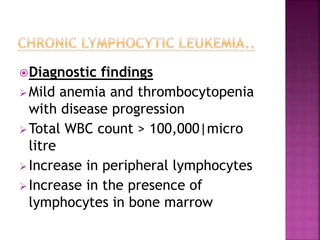
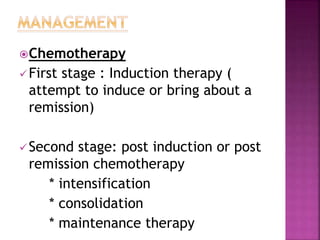
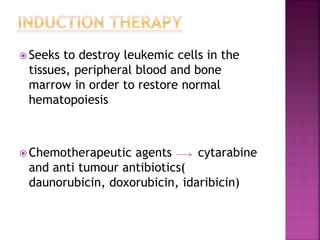
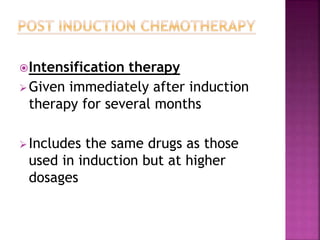
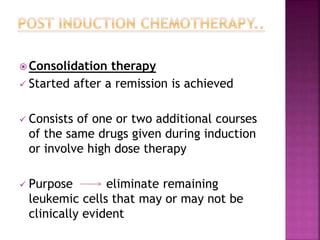
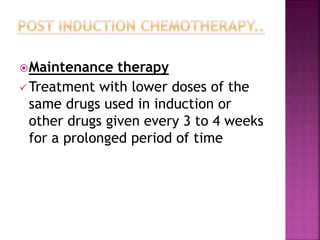
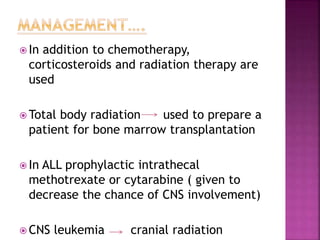
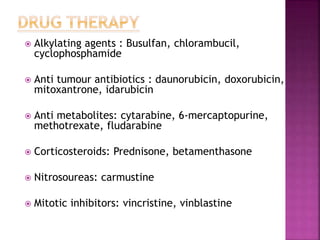
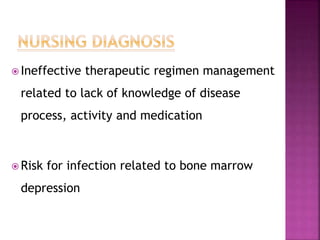
Leukemia is a cancer of the blood and bone marrow that results in abnormal blood cell production and accumulation. The main types are acute myeloid leukemia, acute lymphoblastic leukemia, chronic myeloid leukemia, and chronic lymphocytic leukemia. Risk factors include genetic predispositions, environmental exposures, and prior chemotherapy or radiation therapy. Treatment involves chemotherapy, corticosteroids, radiation therapy, stem cell transplantation, targeted therapy, or biological therapy to destroy leukemia cells and restore normal blood cell production. Nursing care focuses on managing side effects, preventing infections, providing education and support, and monitoring the patient's condition and response to treatment.