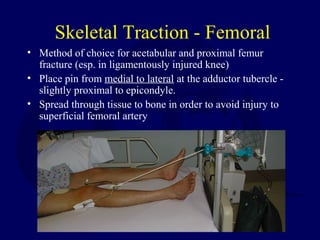
This document discusses principles and techniques for closed reduction, traction, and casting of fractures. It describes how adequate analgesia, axial traction, and restoration of length, rotation and angulation are critical for successful closed reduction. Common techniques like Bier blocks, hematoma blocks, splinting and casting are outlined. Complications of immobilization like pressure sores, joint stiffness and thromboembolism are also reviewed. The use of skin traction, skeletal traction using pins, and halo fixation are described.