This document discusses the surgical management and approaches for spinal tuberculosis. Key points include:
- Surgical management includes debridement of diseased vertebrae, drainage of abscesses, arthrodesis for instability, and decompression for neurological complications.
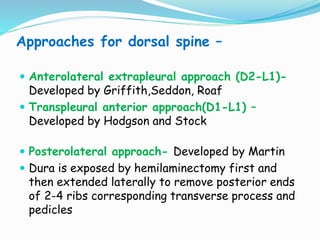
- Common surgical approaches discussed for different spinal regions include anterior, posterior, anterolateral, costotransversectomy, and laminectomy.
- Indications for surgery include neurological deficits not improving with conservative treatment, mechanical instability, and prevention of severe kyphosis.