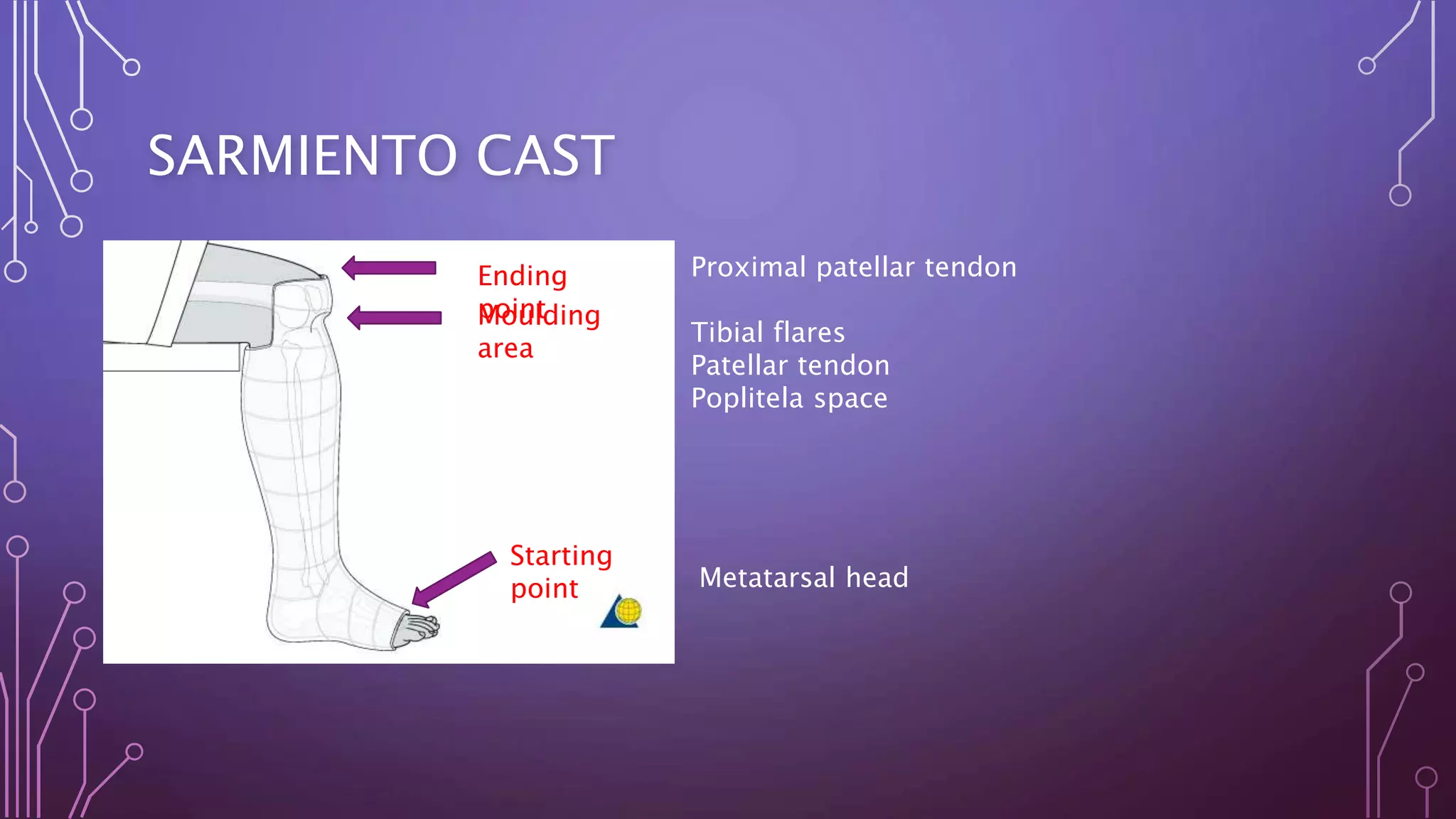
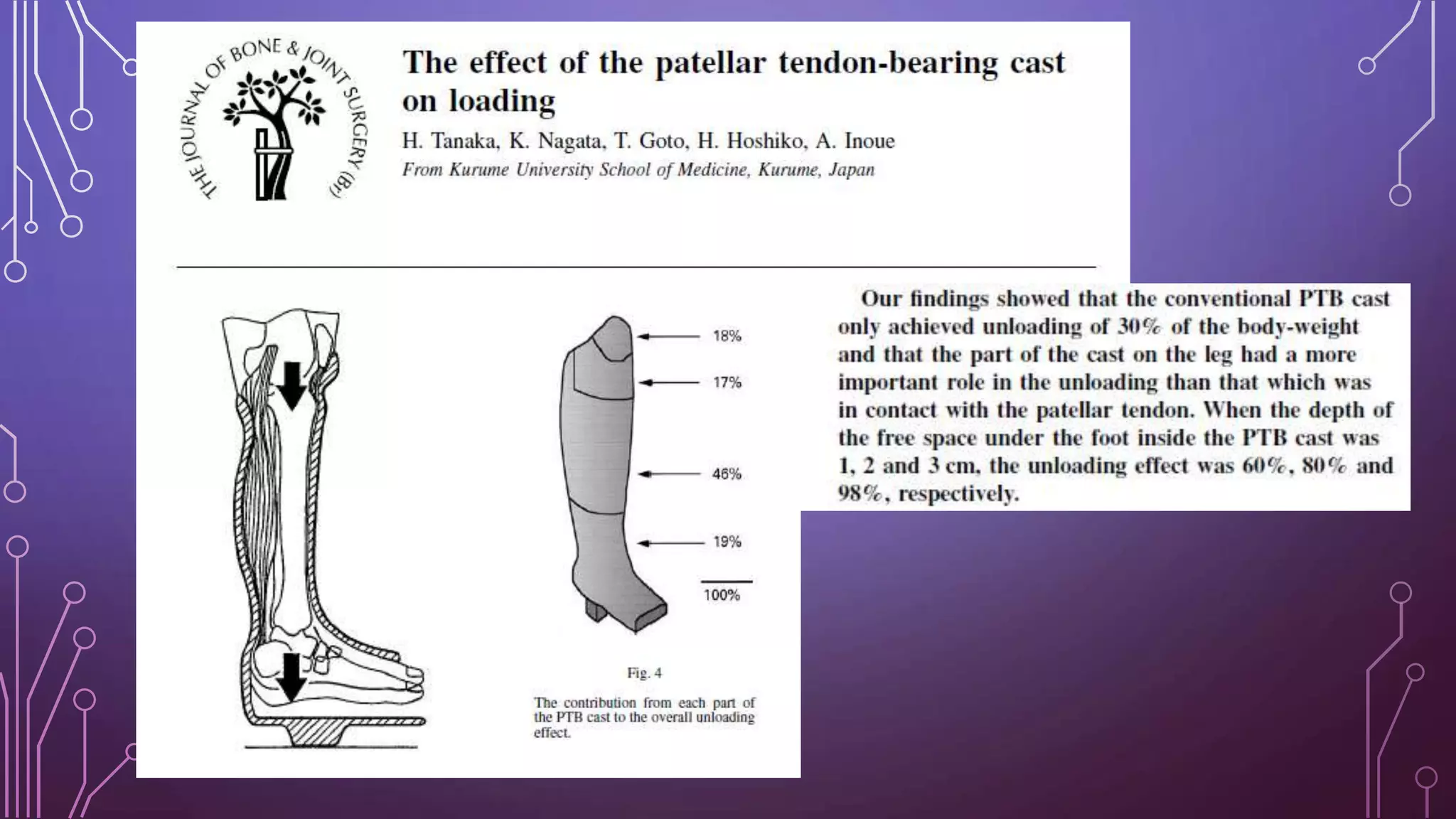
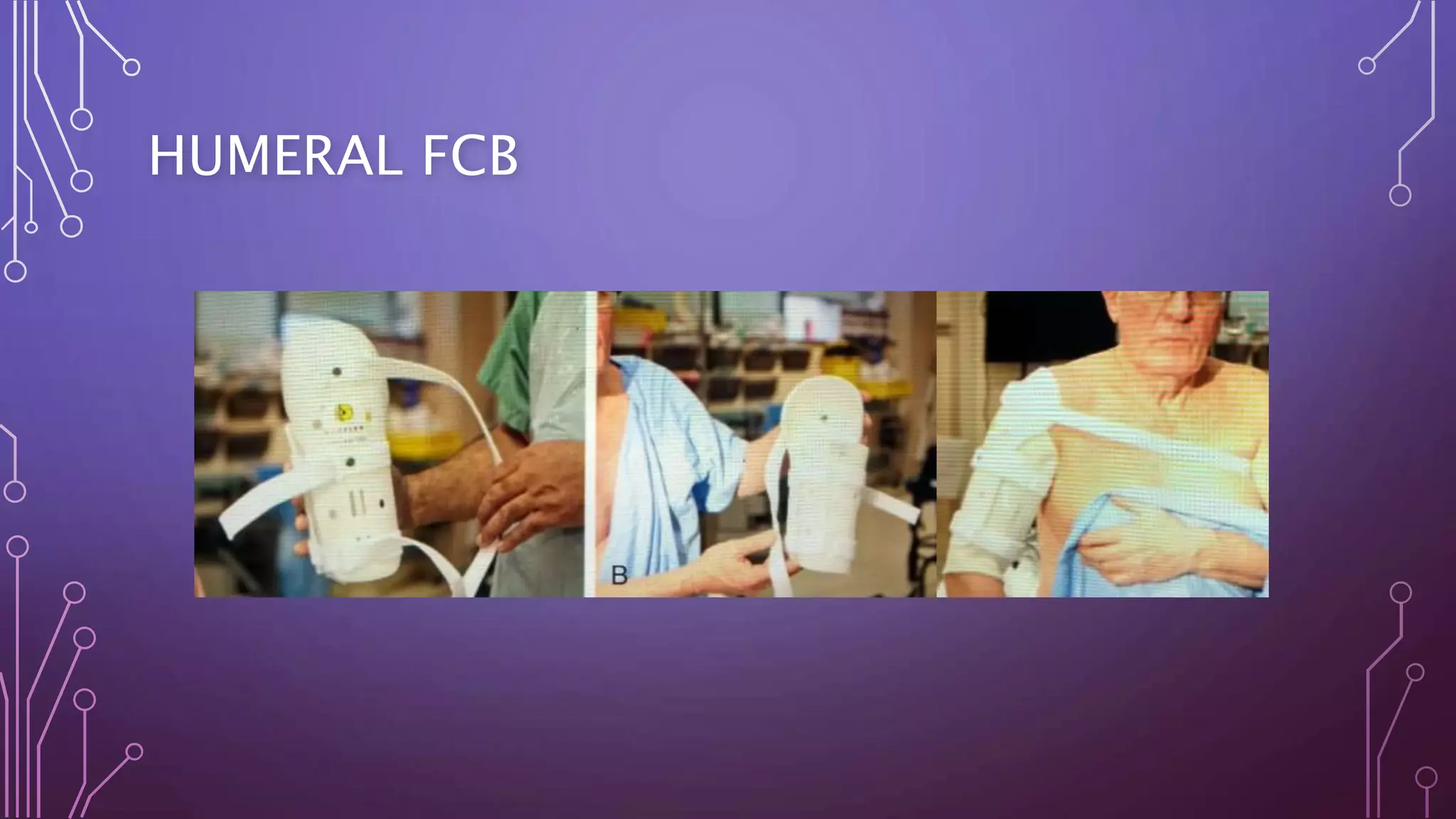
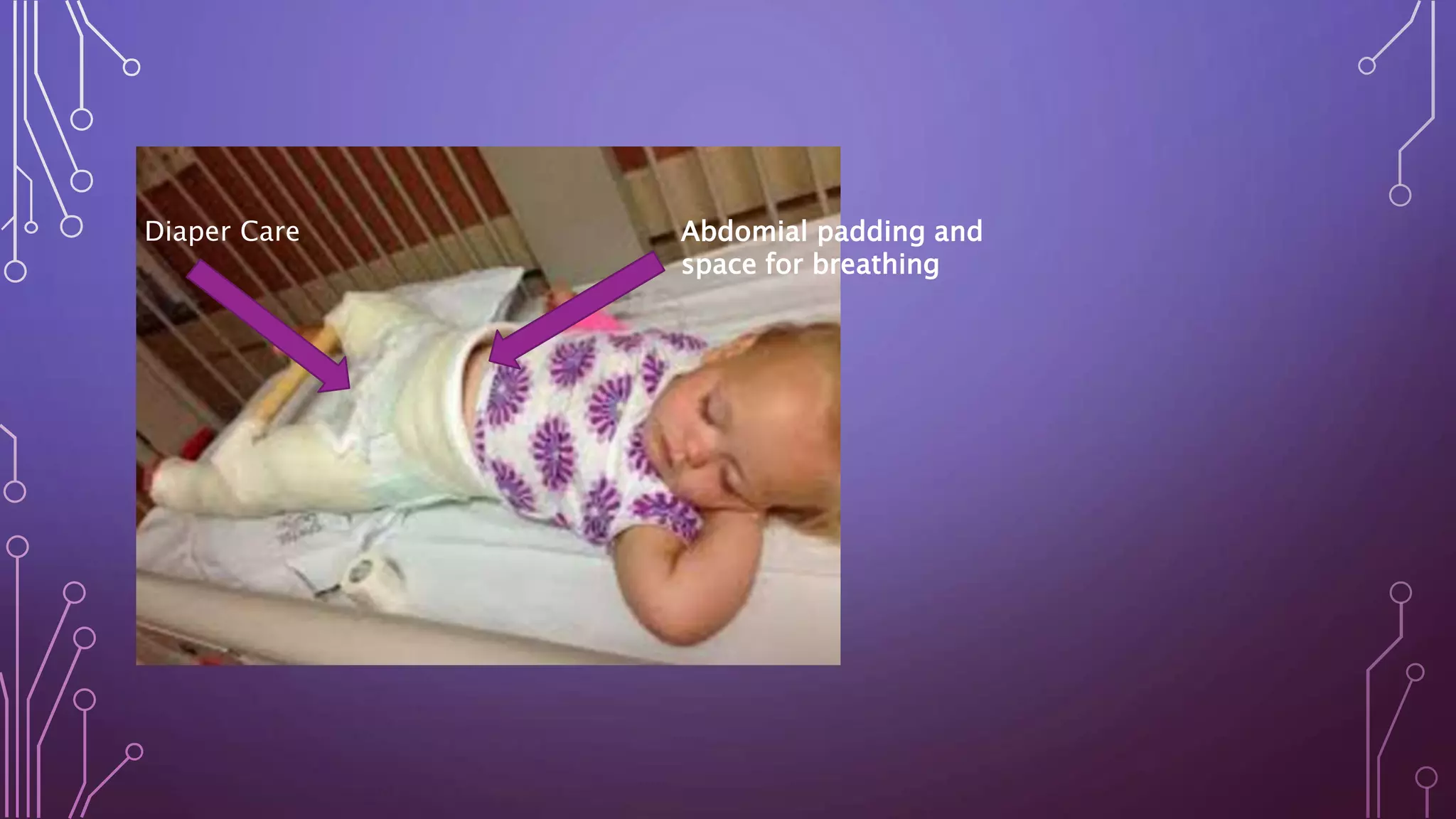
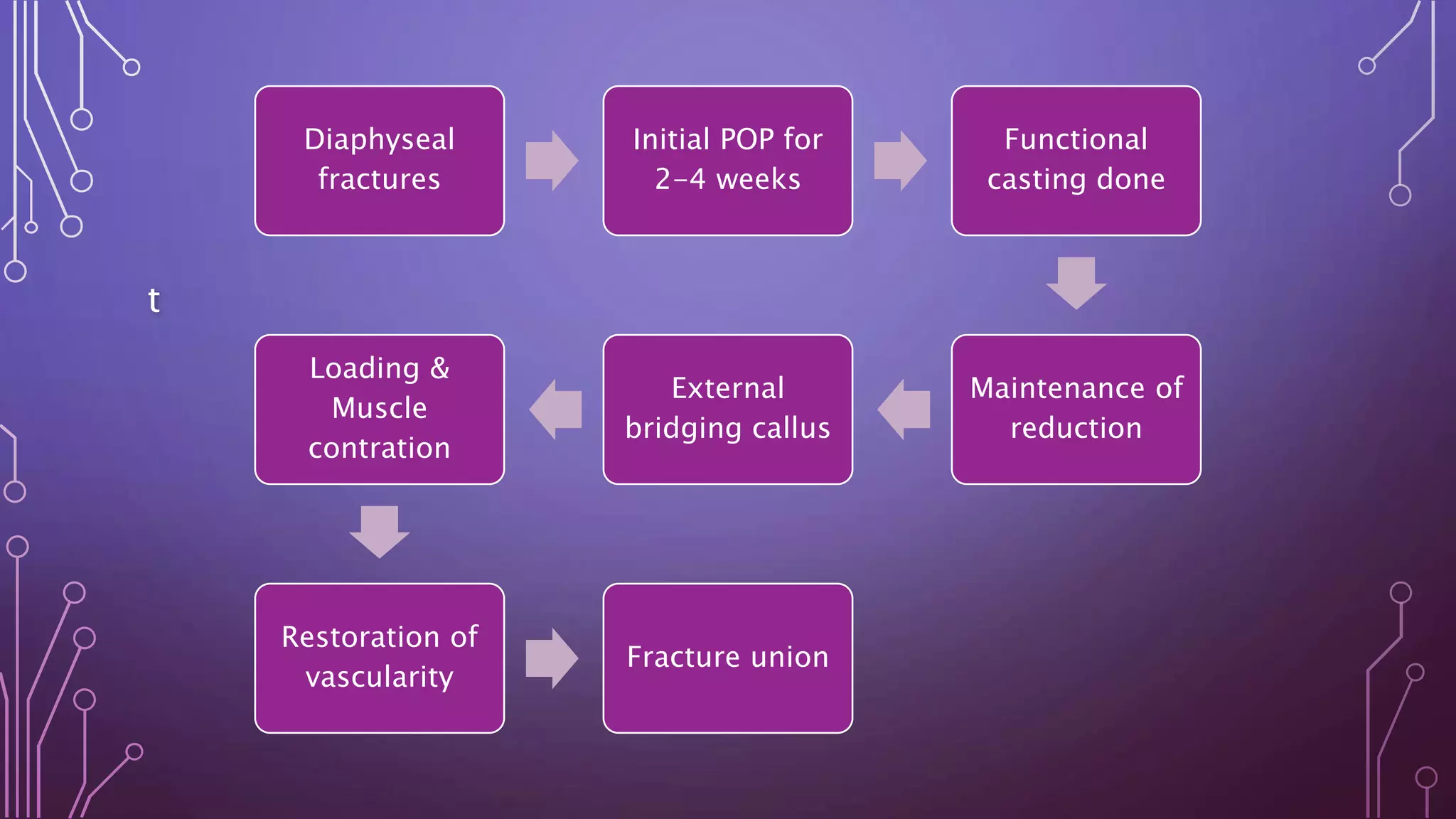
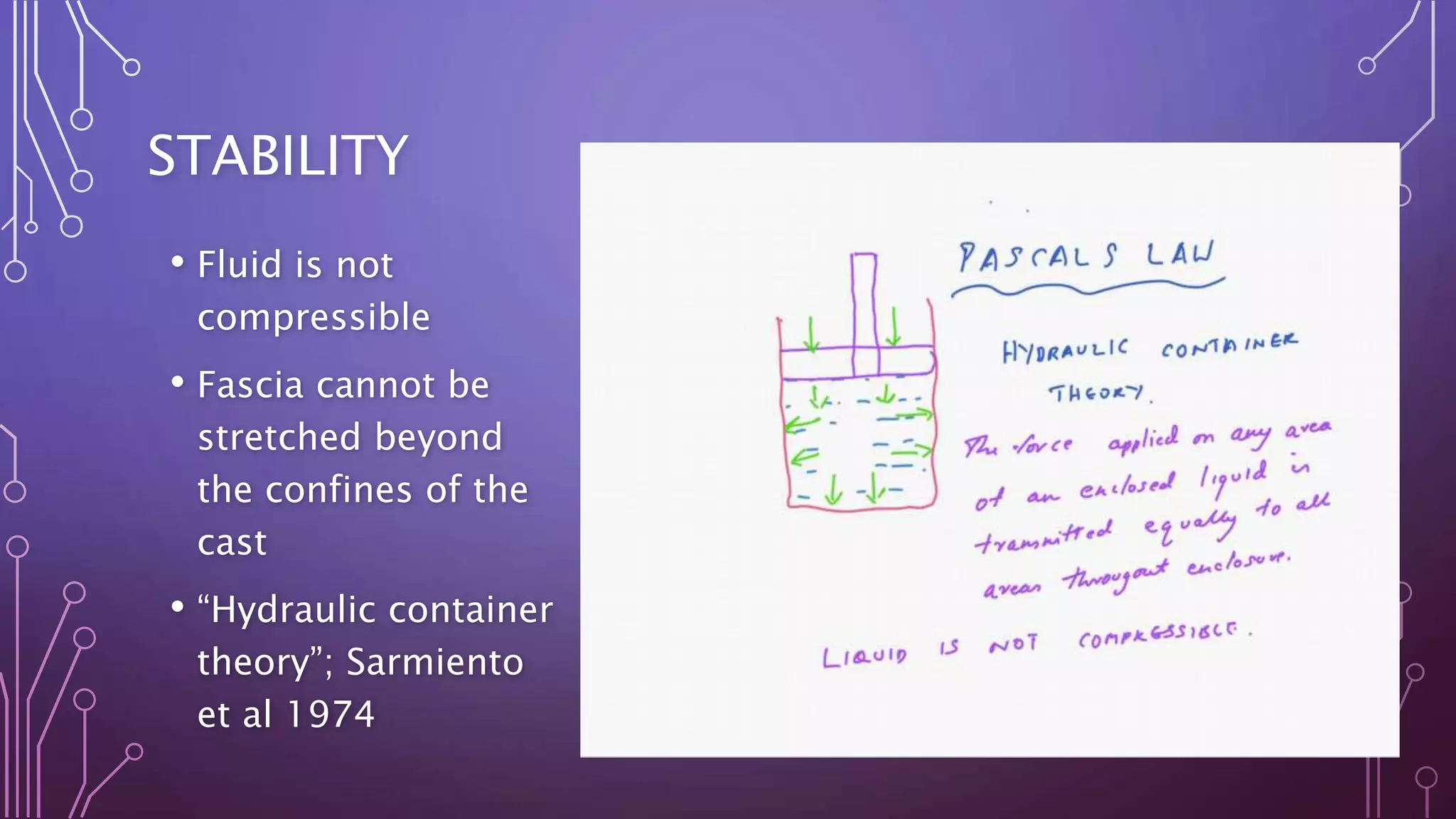
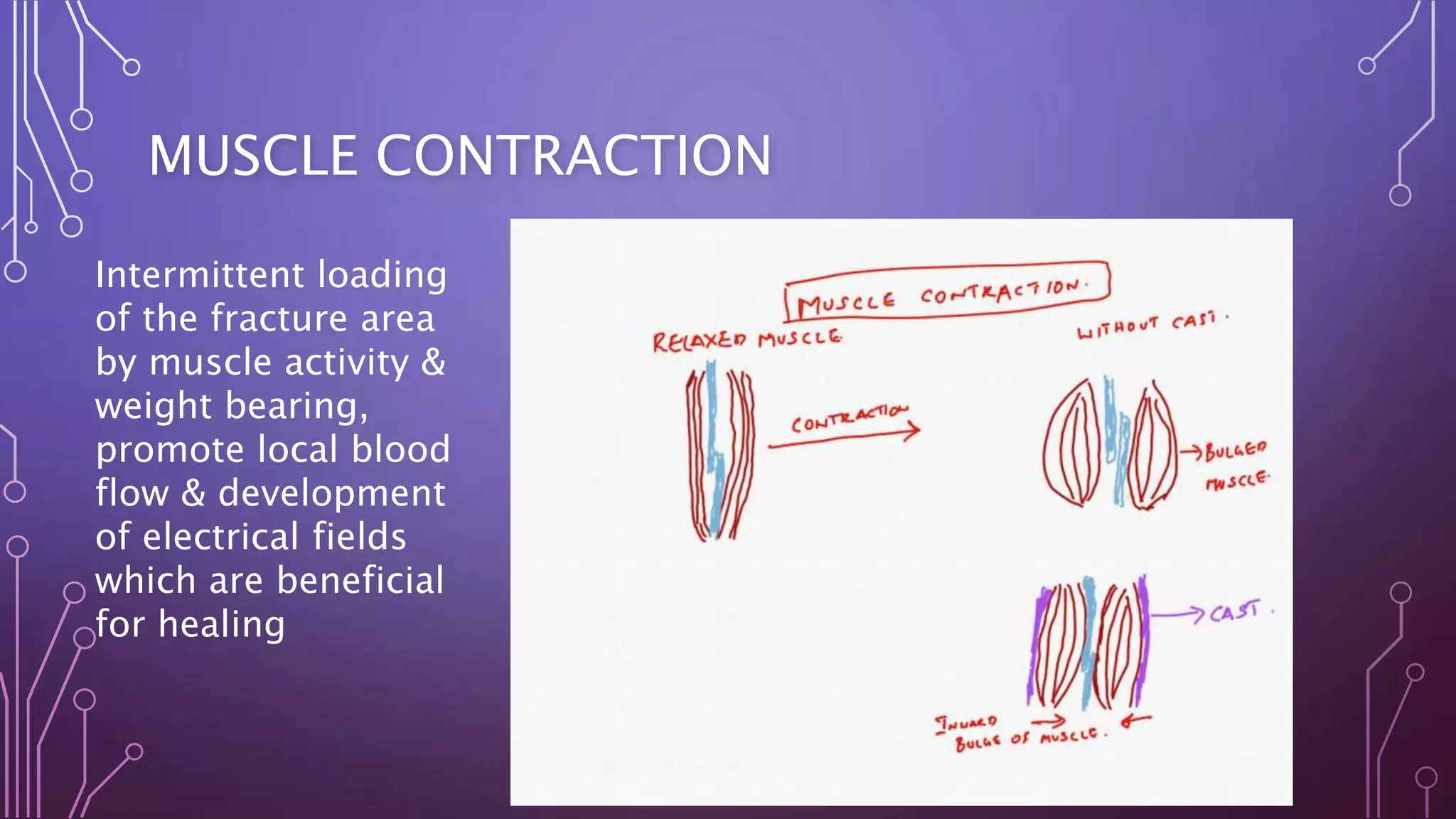
The document discusses functional casting and bracing techniques used to treat fractures while allowing restricted movement. It describes the principles of functional casting which include maintaining stability and reduction while promoting blood flow and muscle contraction to encourage healing. Specific casts for treating fractures of the humerus, tibia, femur and hip are outlined, including the Sarmiento cast and hip spica cast. The timing, positioning and complications of different casts are summarized. Functional casting aims to continue function during fracture healing to accelerate rehabilitation.










![CONTRAINDICATION
• Intraarticular fractures.
• Compound fractures
• Lack of co-operation by the pt.
• Patient with spastic disorders
• Bed-ridden & mentally incompetent pts.
• Deficient sensibility of the limb [D.M with P.N]
• Fractures of both bones forearm when reduction is difficult.](https://image.slidesharecdn.com/dr-171010183241/75/Dr-S-Senthil-Sailesh-functional-cast-bracing-PTBcast-sarmiento-principle-14-2048.jpg)
![NOT USED IN
• Galeazzi fractures
• Monteggia fractures
• Proximal half of shaft of femur [tends to angulate in to varus
only used by expert]
• Isolated # of tibia, fibula
• Tends to cause varus angulation and to delay in consolidation
of #.](https://image.slidesharecdn.com/dr-171010183241/75/Dr-S-Senthil-Sailesh-functional-cast-bracing-PTBcast-sarmiento-principle-15-2048.jpg)