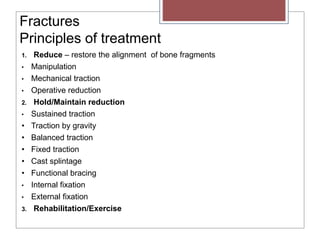
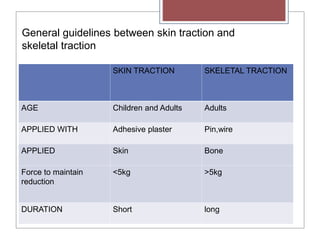
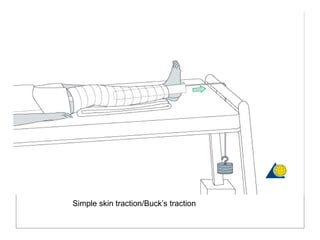
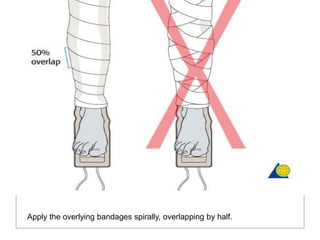
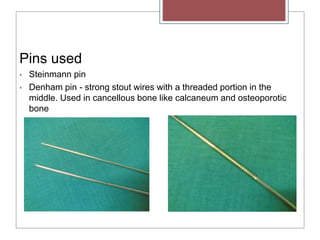
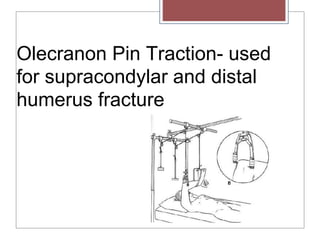
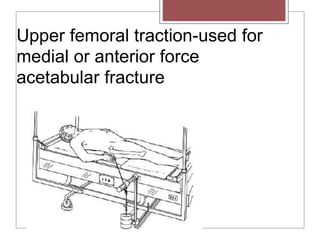
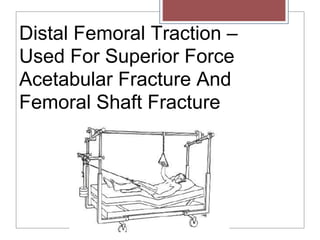
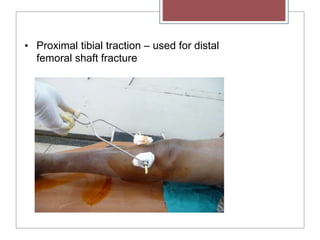
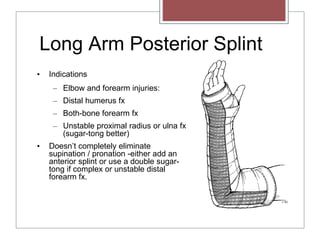
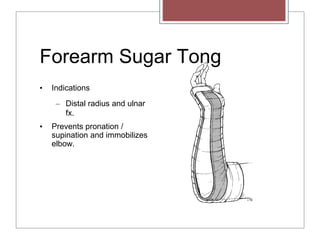
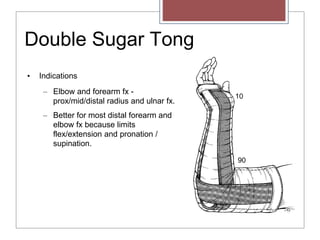
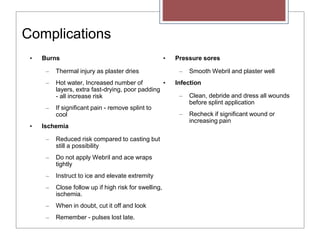
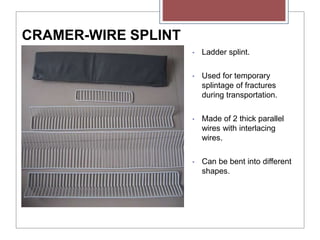
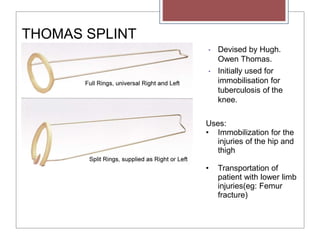
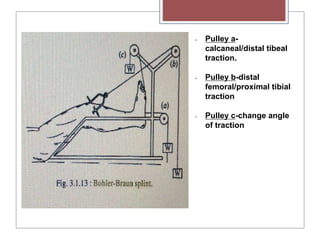
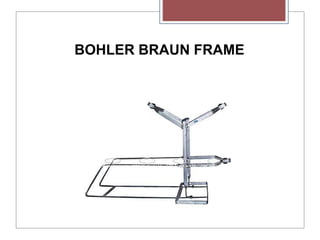
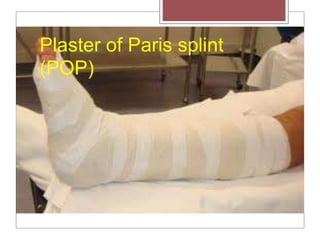
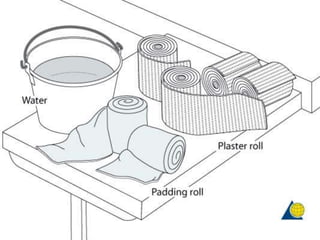
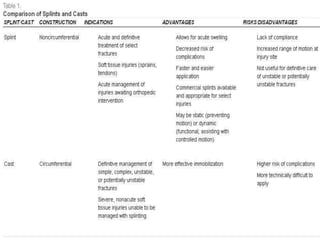
This document discusses various methods of fracture treatment including traction, splinting, and plaster of Paris. It provides details on skin traction and skeletal traction, including indications, application techniques, and complications. It also outlines different types of splints and how to properly apply and care for plaster of Paris casts. The goal of these treatments is to reduce fractures, maintain alignment, and allow rehabilitation through immobilization and gradual reduction of muscular forces.