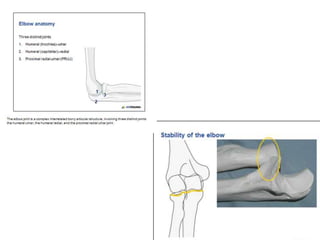
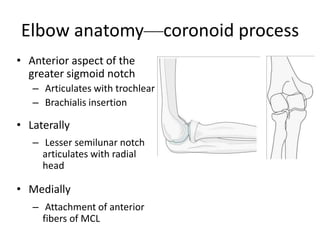
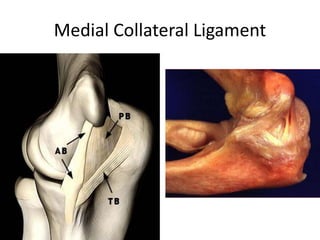
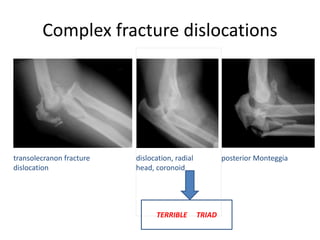
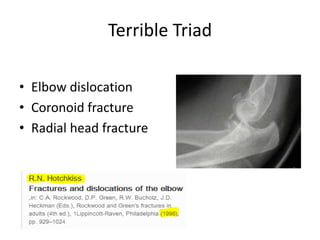
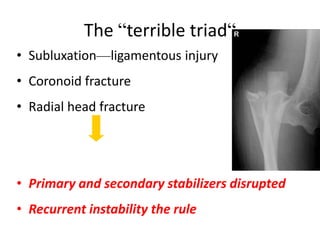
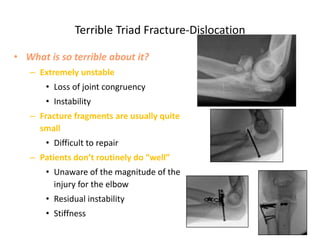
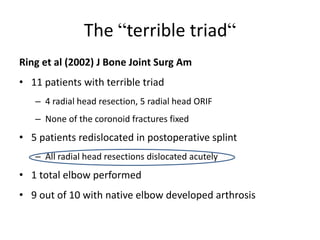
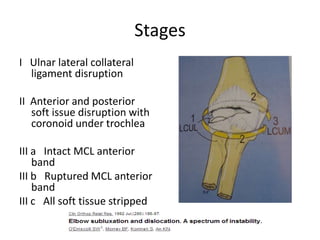
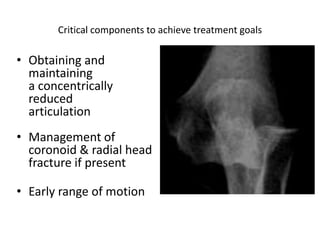
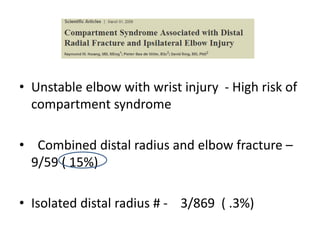
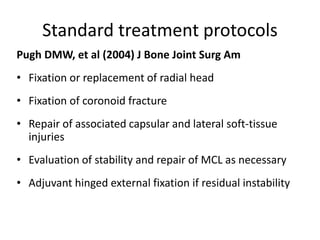
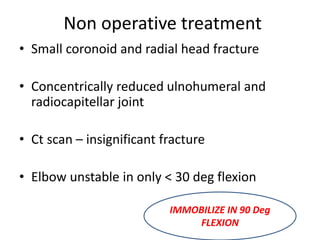
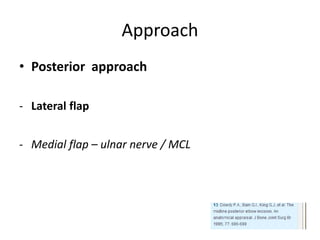
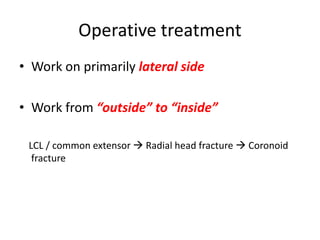
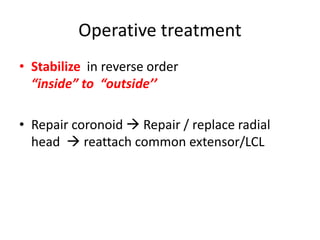
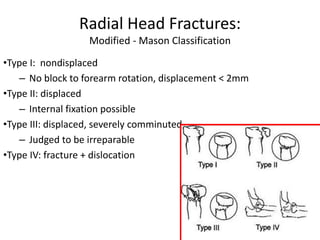
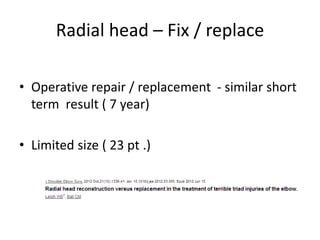
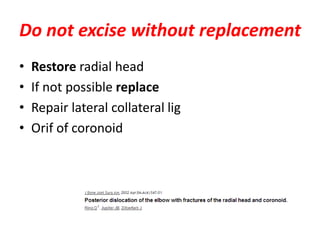
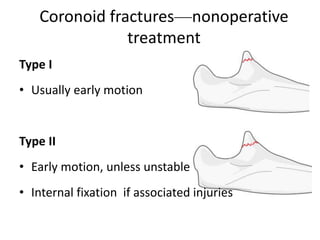
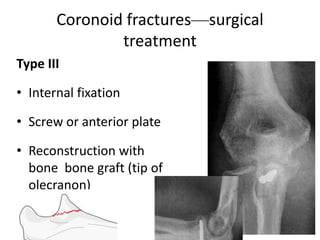
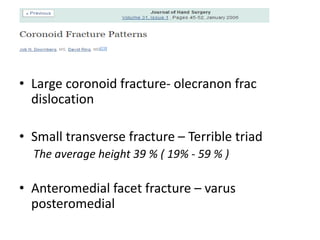
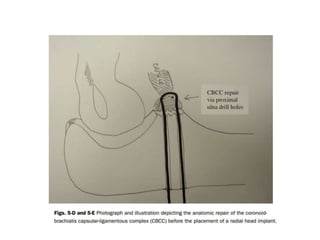
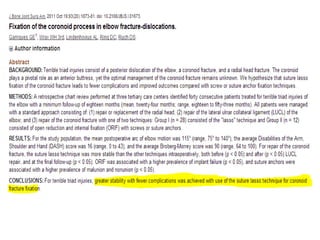
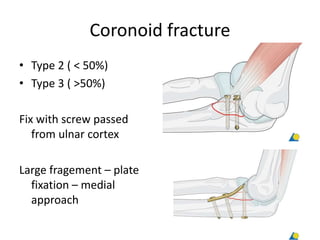
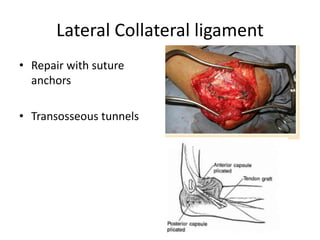
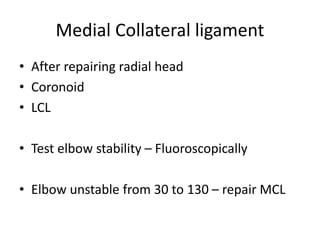
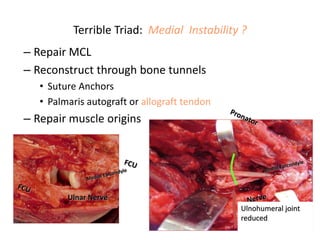
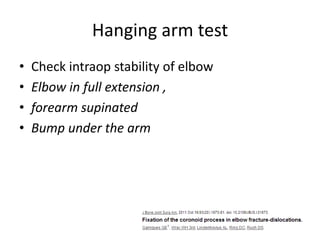
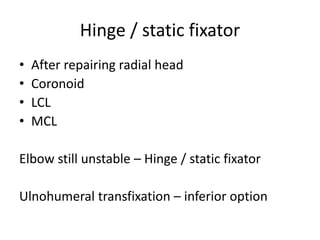
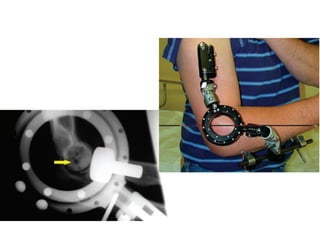
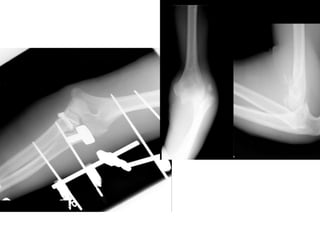
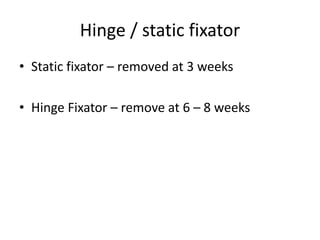
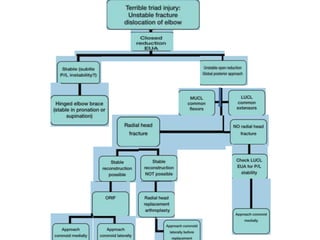
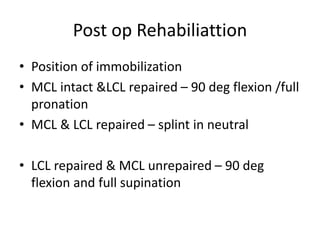
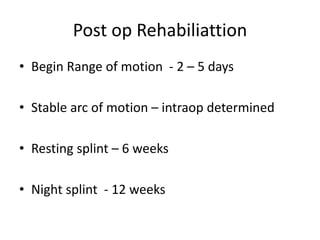
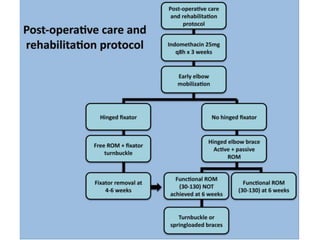
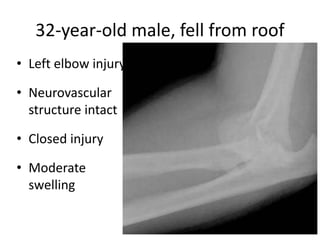
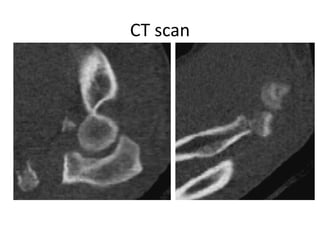
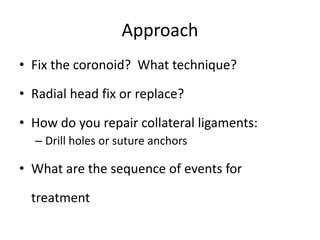
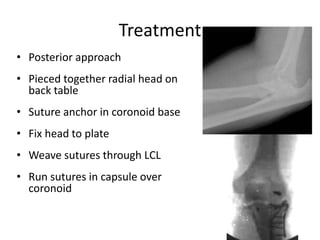
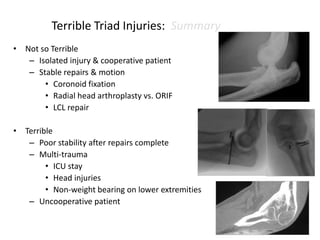
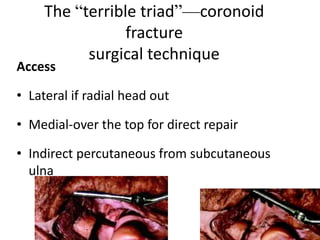
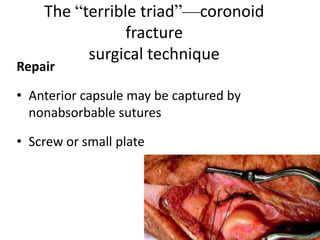
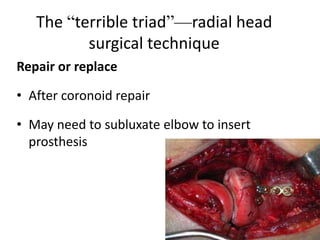
The "terrible triad" refers to an elbow dislocation with fractures of the coronoid process and radial head. This is an extremely unstable injury that often leads to recurrent instability, stiffness, and arthritis. Surgical treatment aims to address all fractures, repair ligaments, and restore stability through techniques like internal fixation, replacement, and external fixation. Postoperative rehabilitation focuses on early range of motion while protecting the repair.