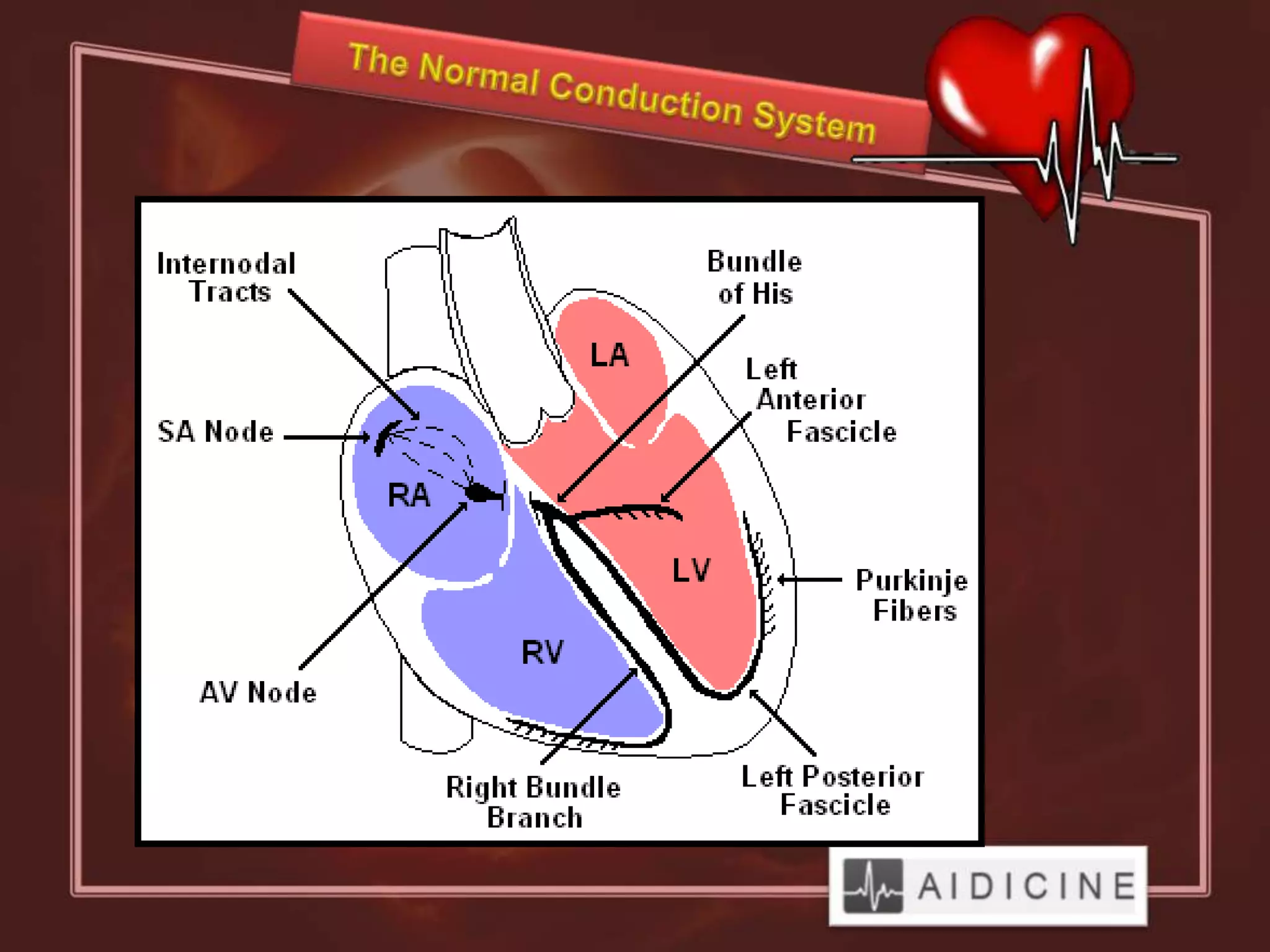
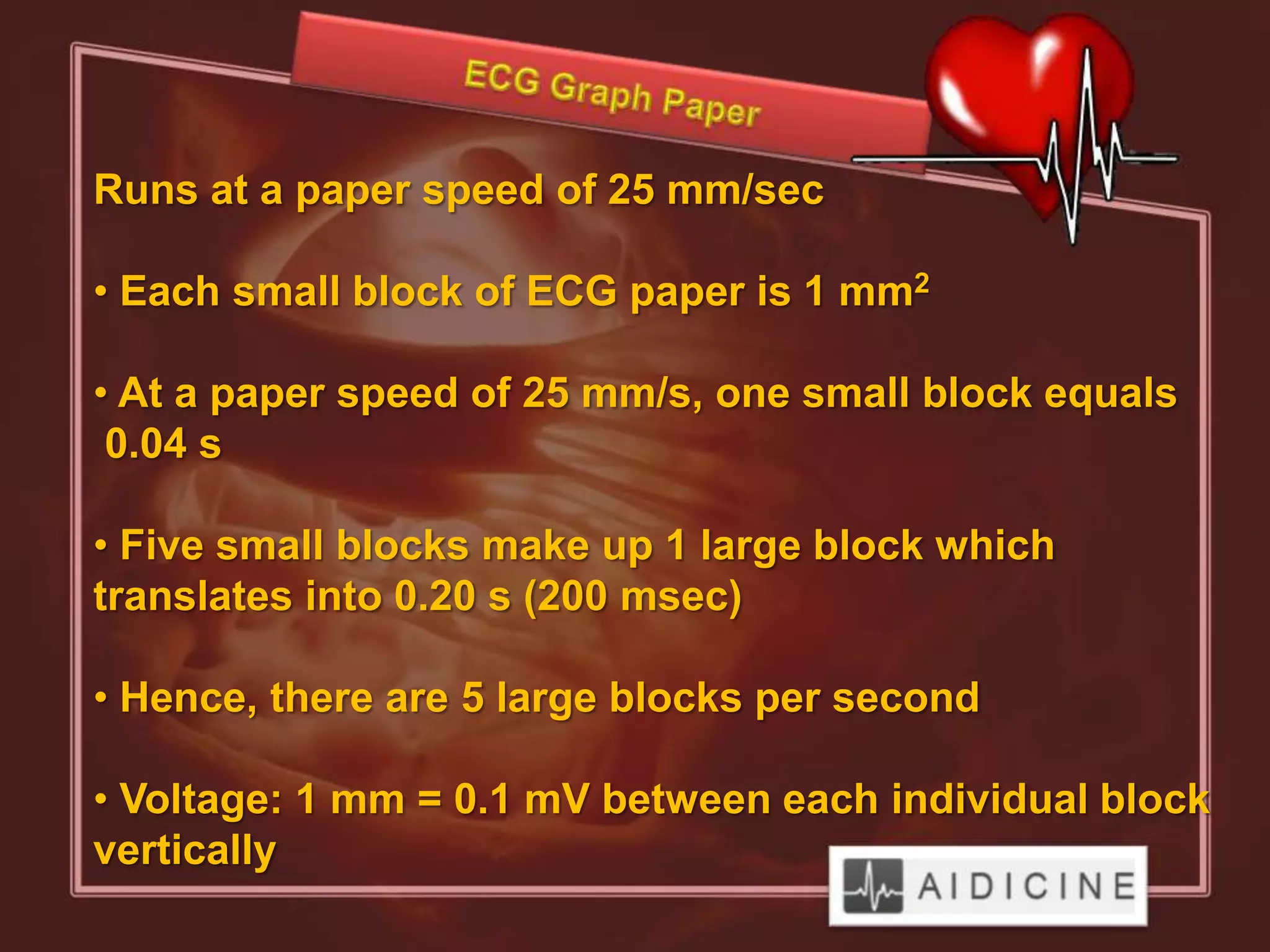
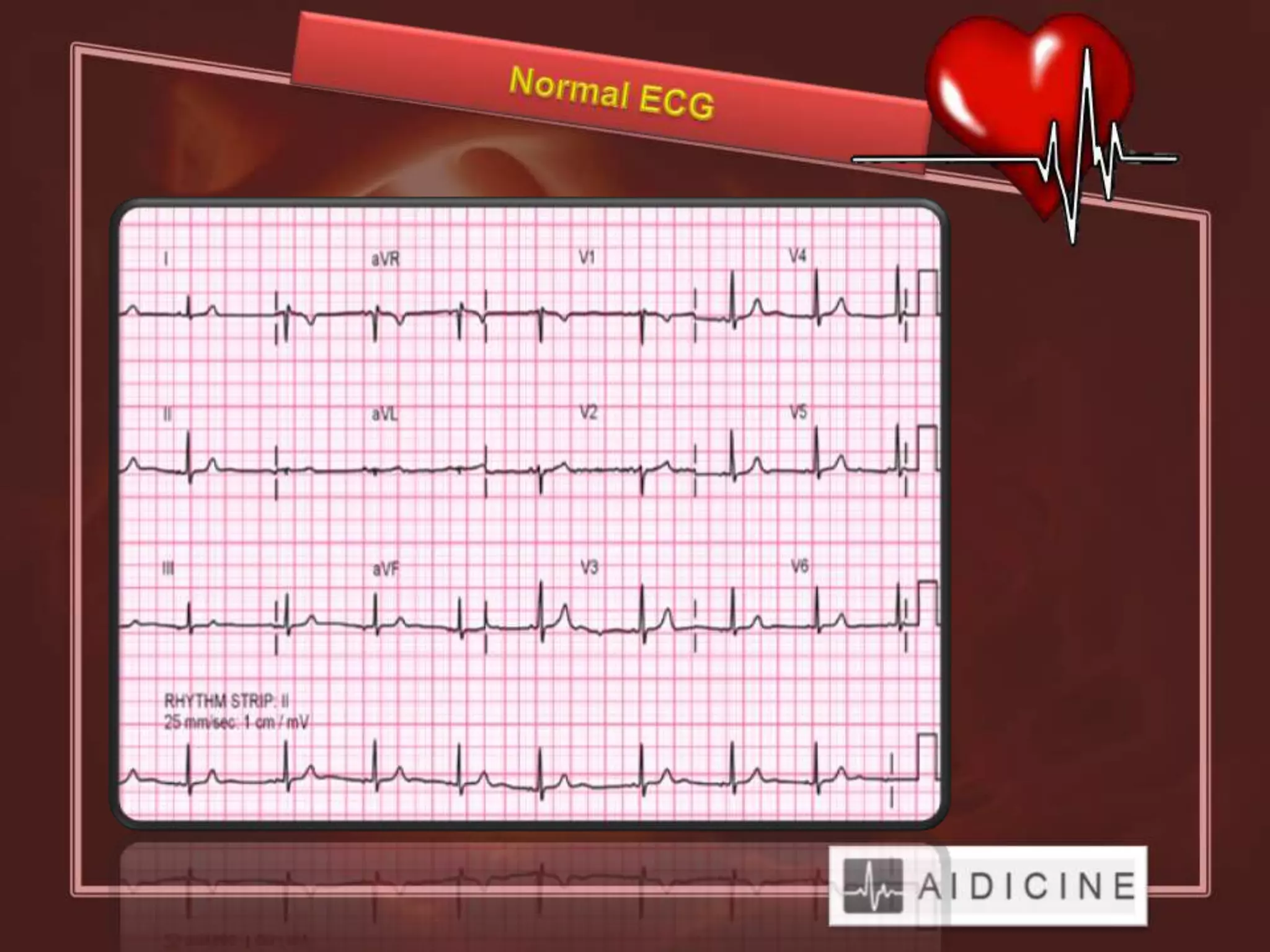
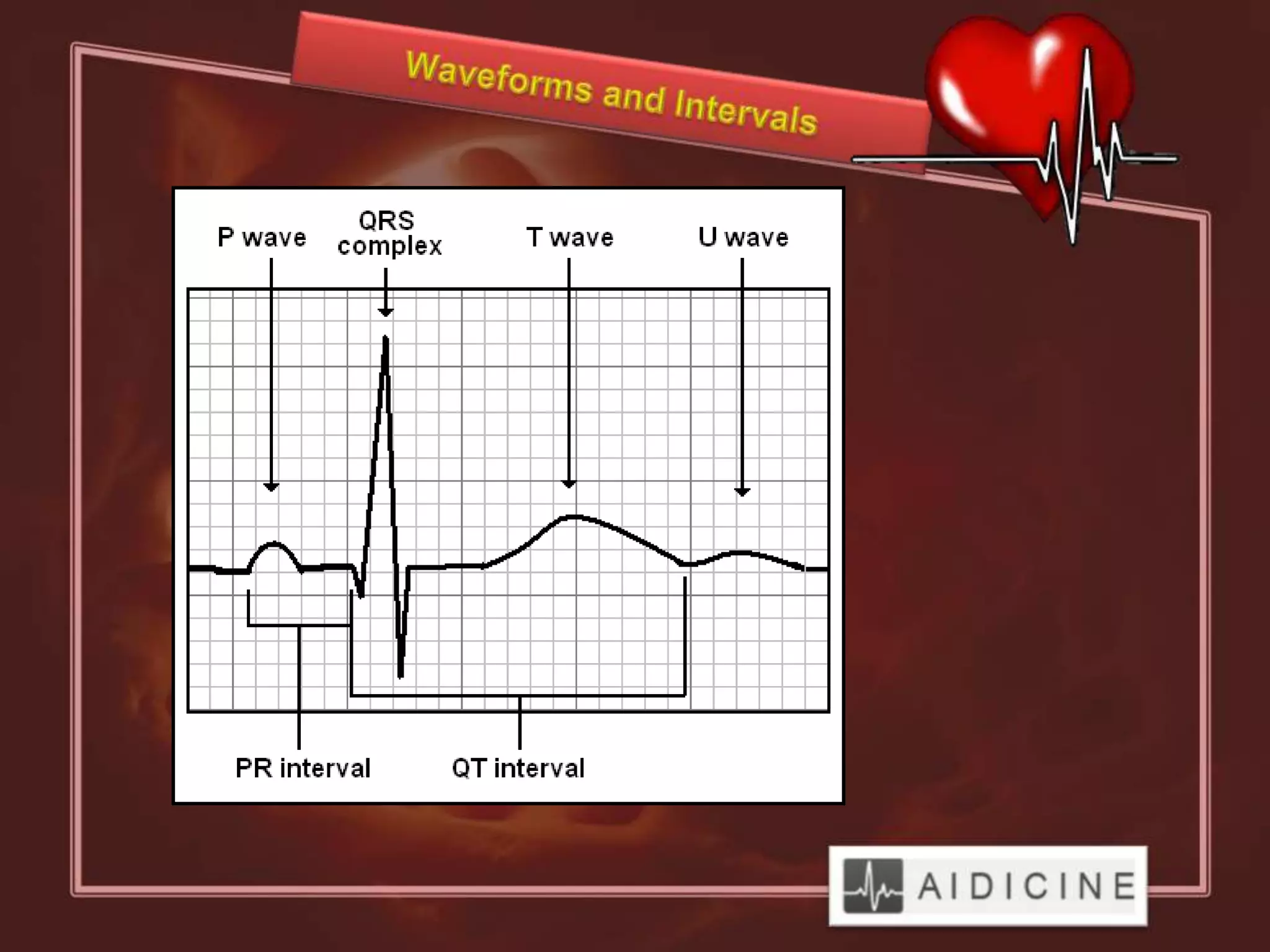
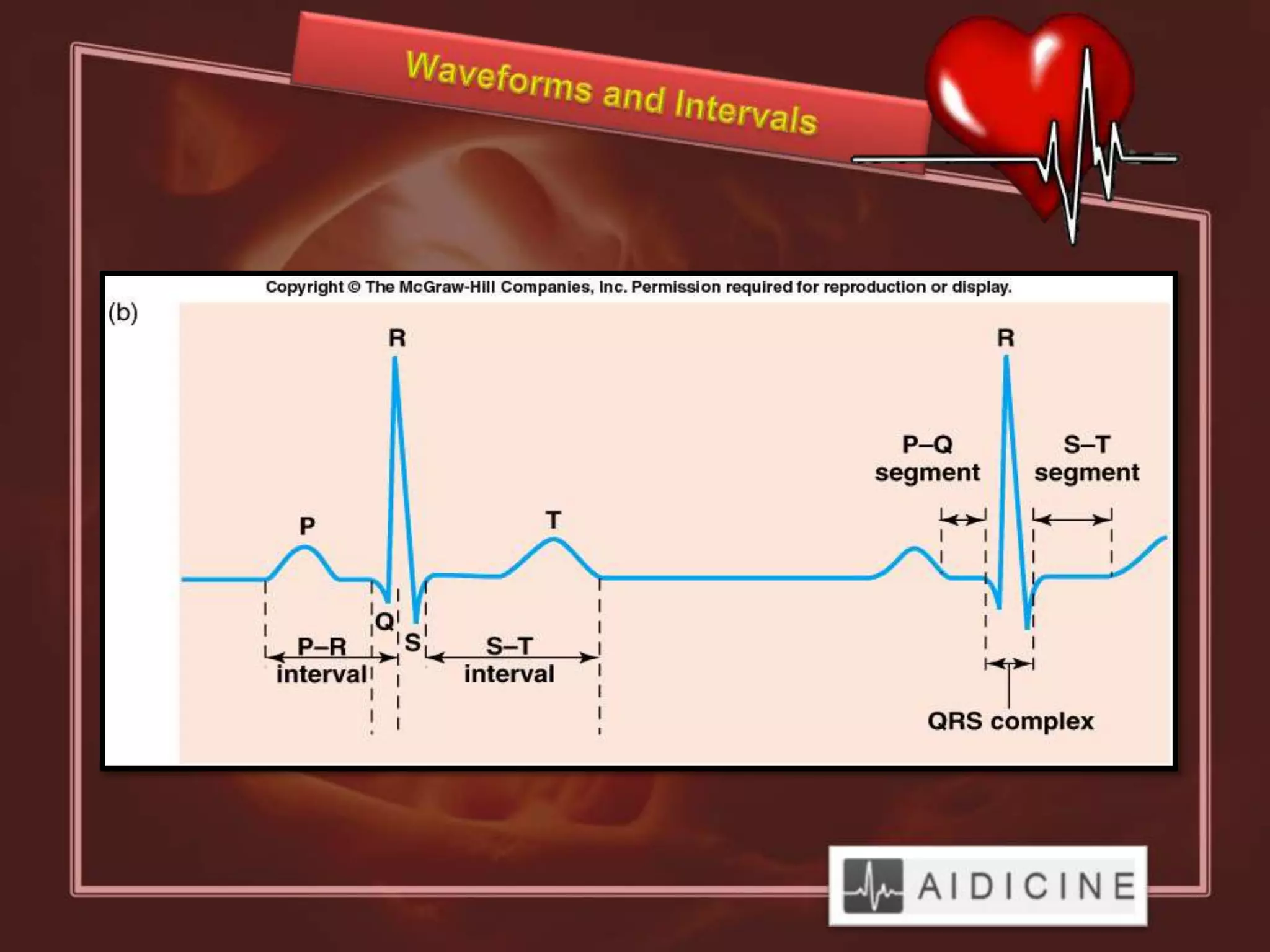
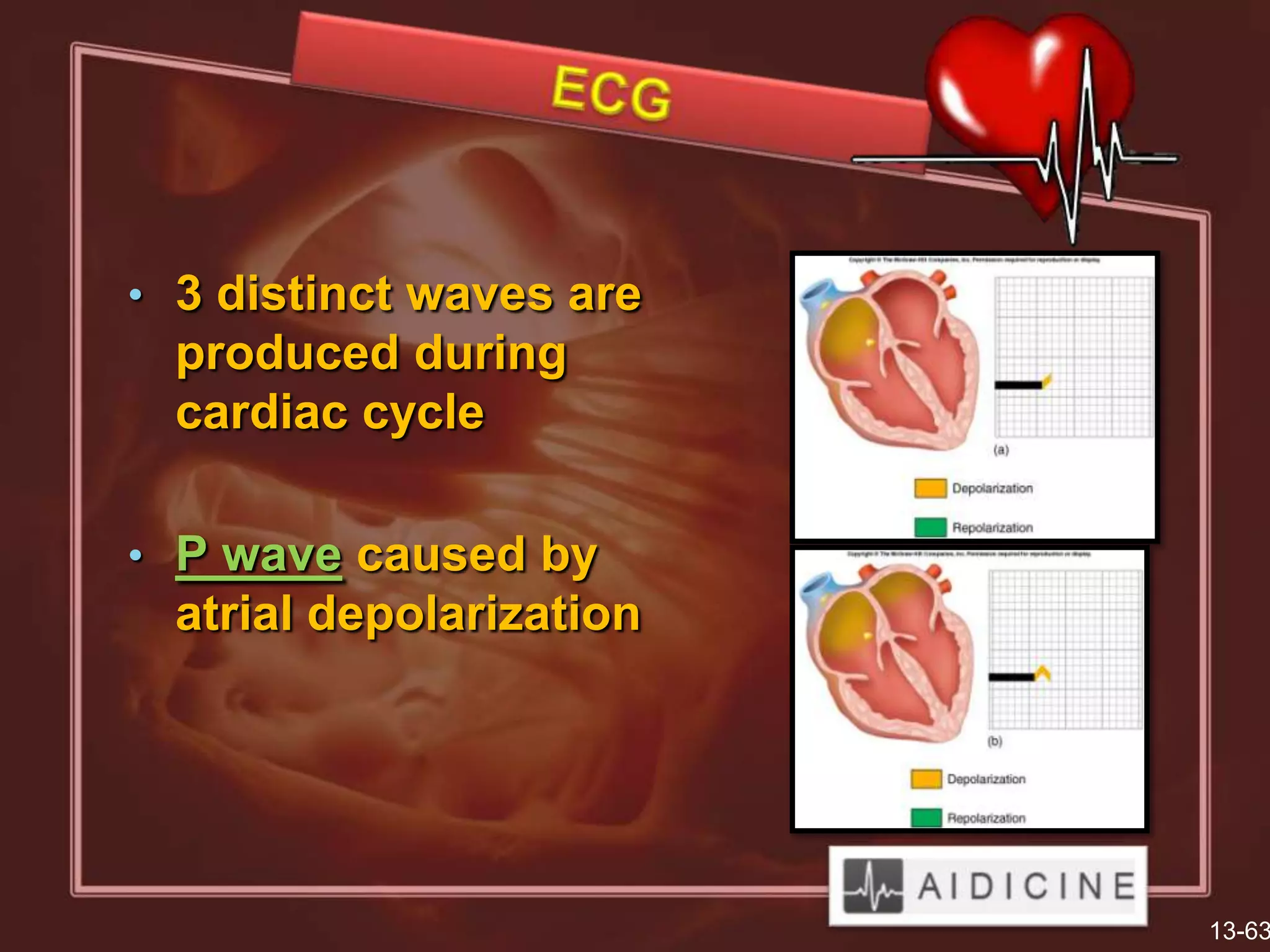
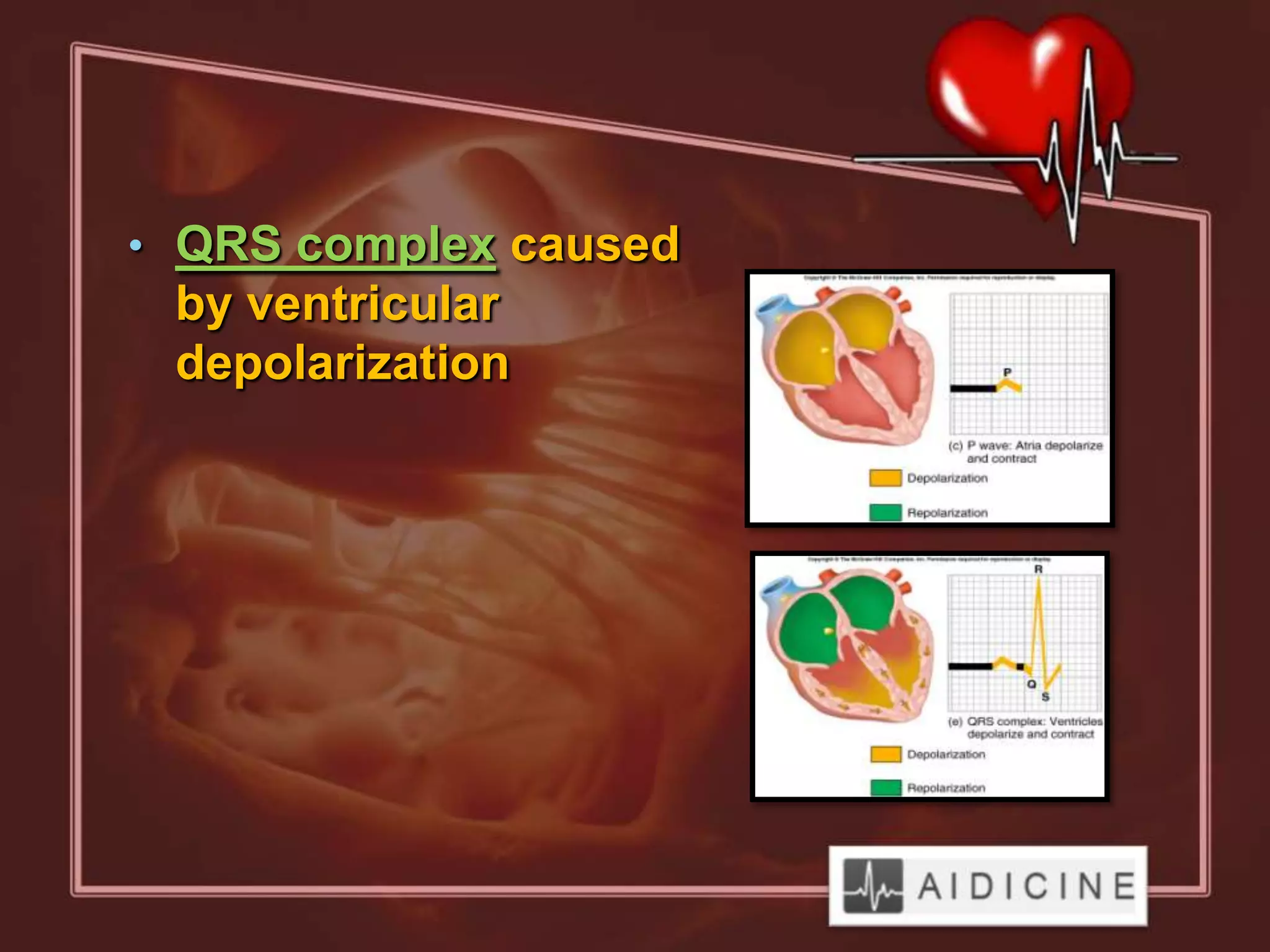
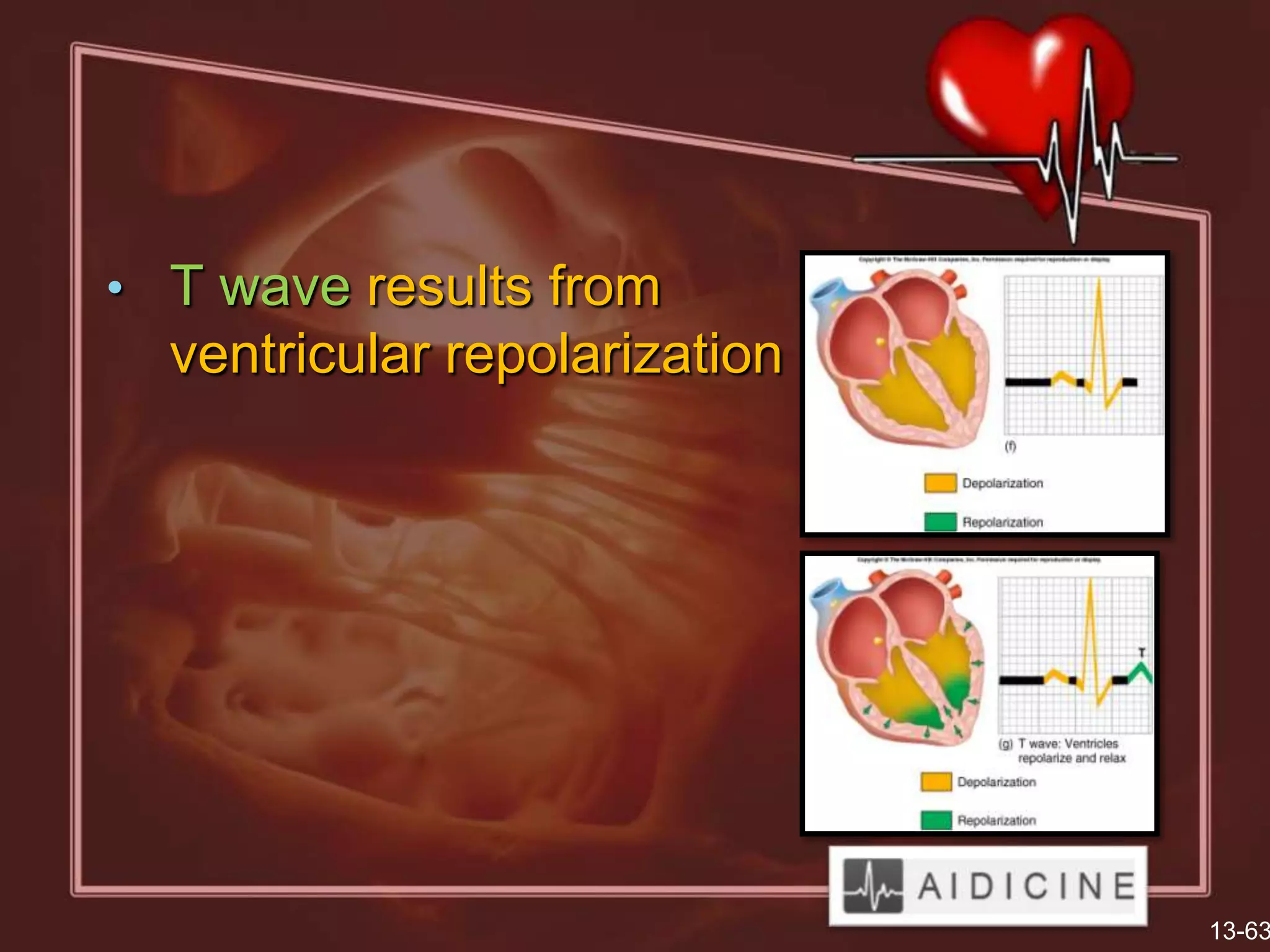
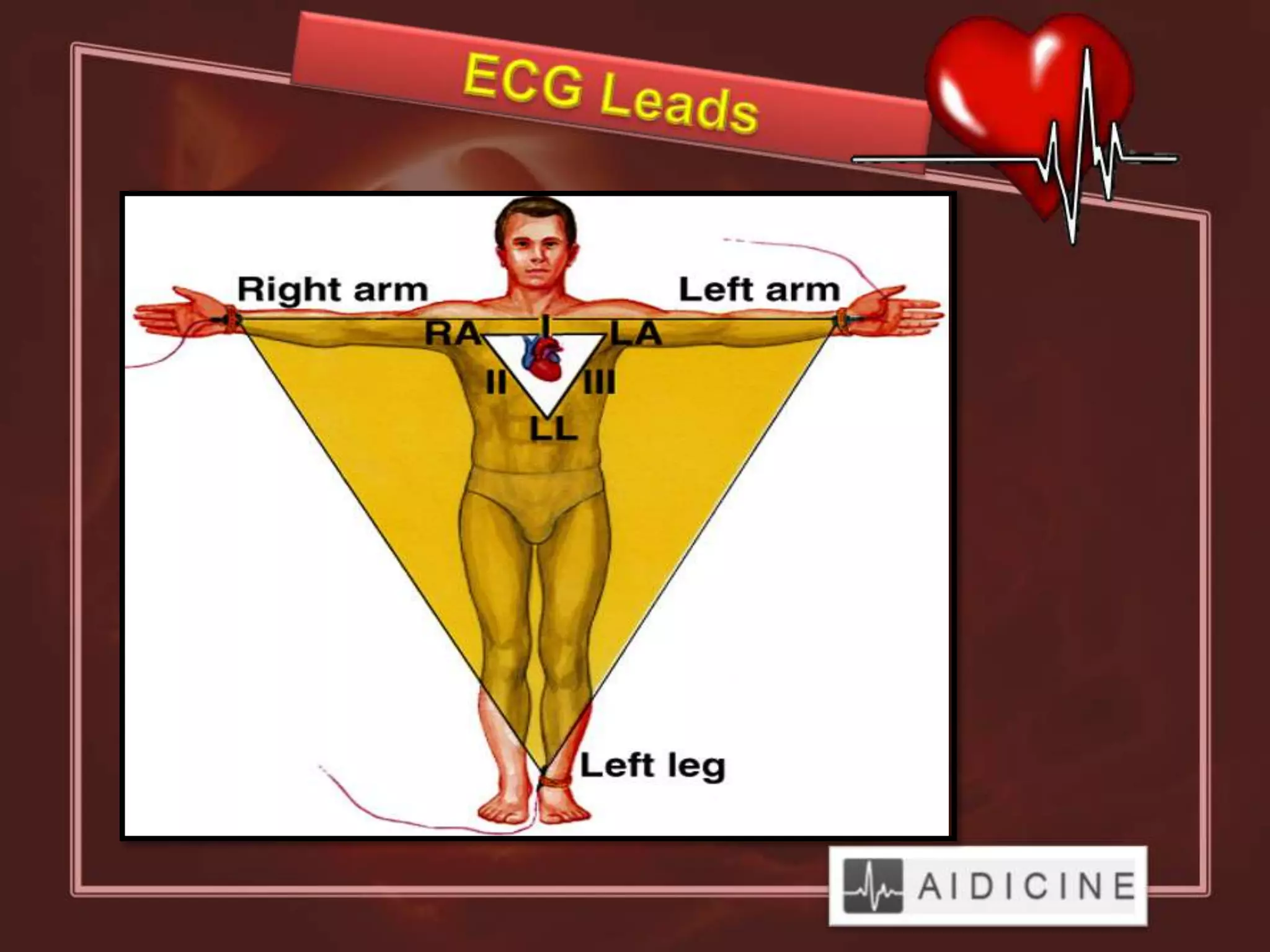
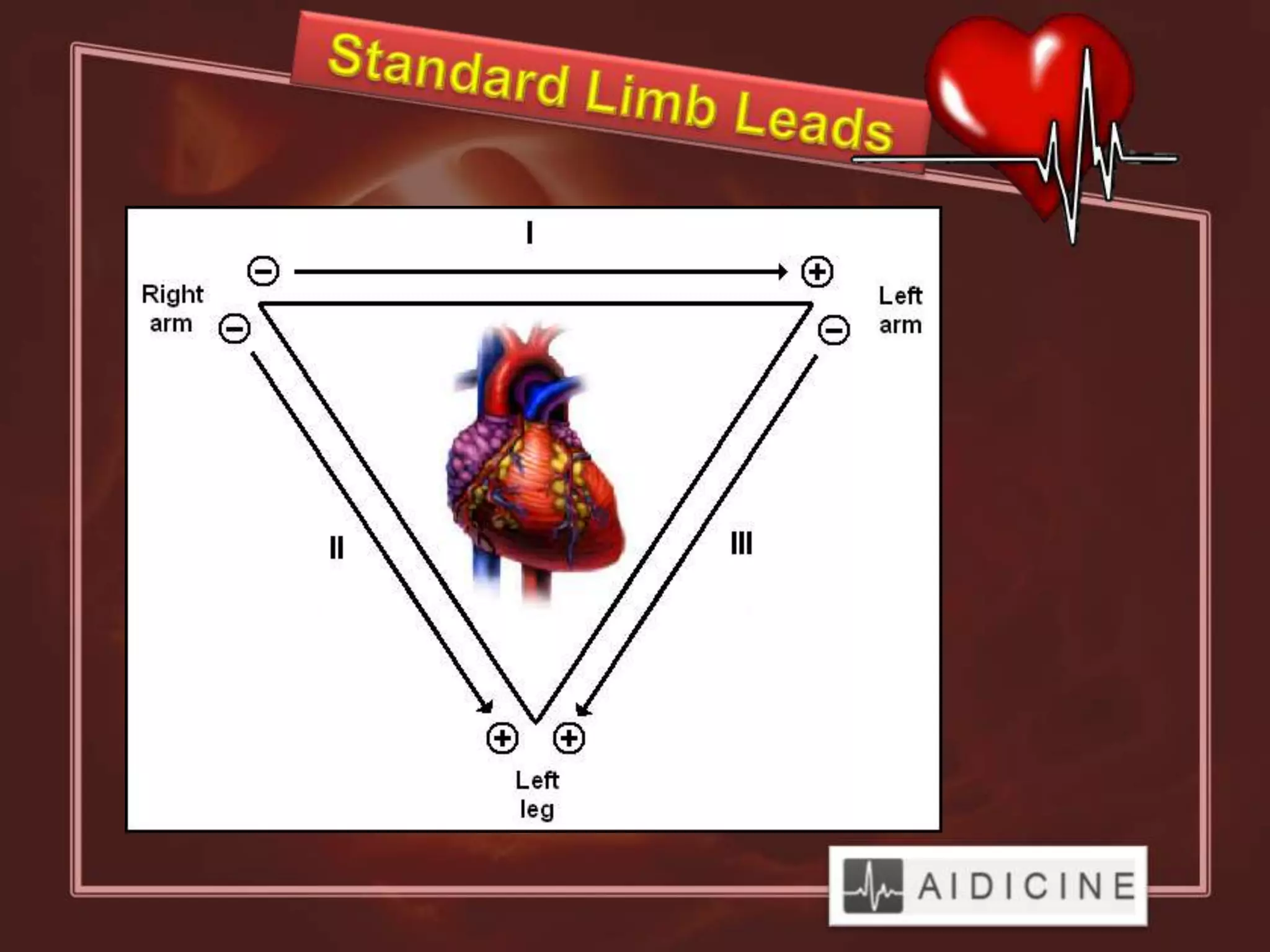
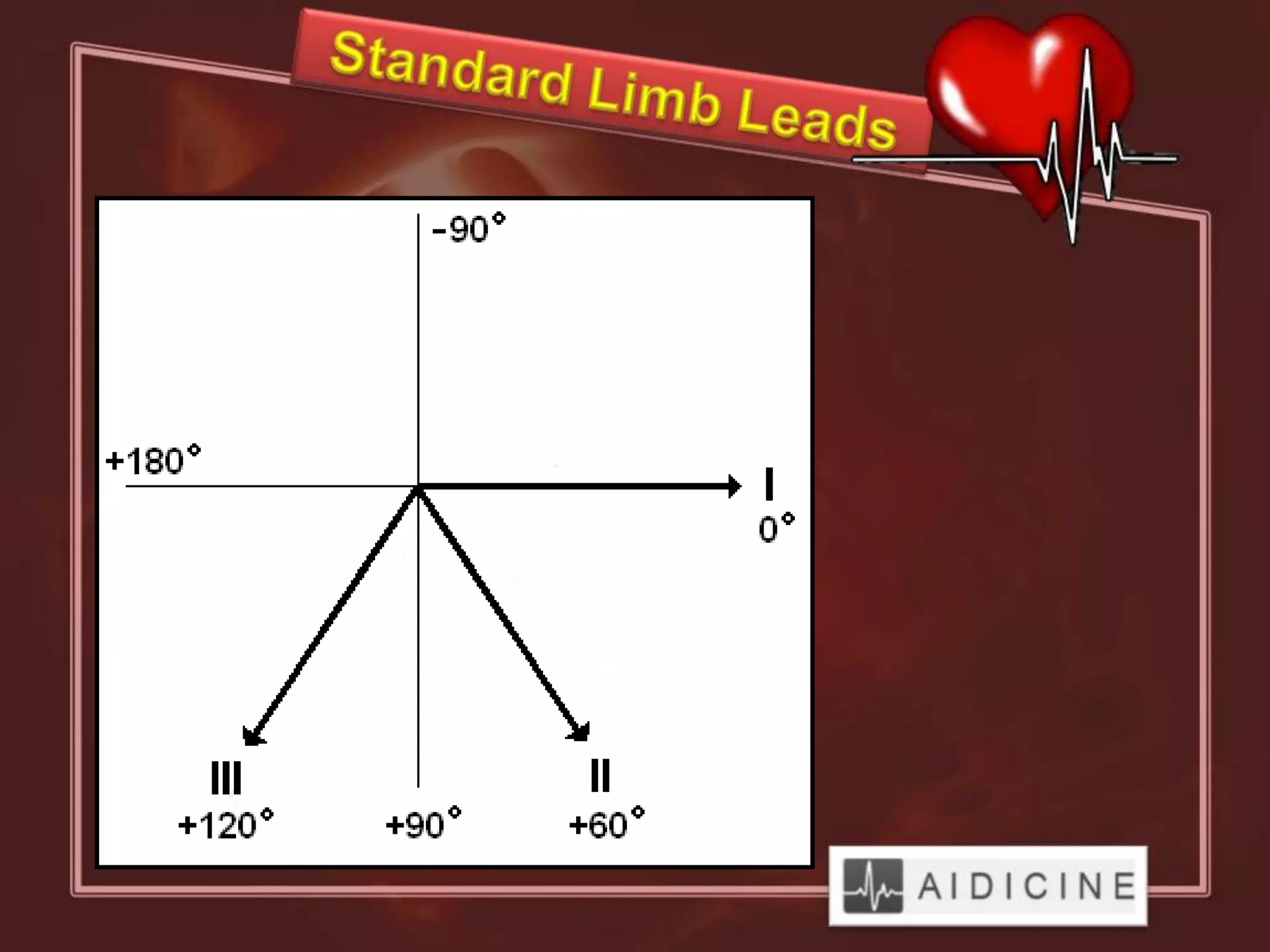
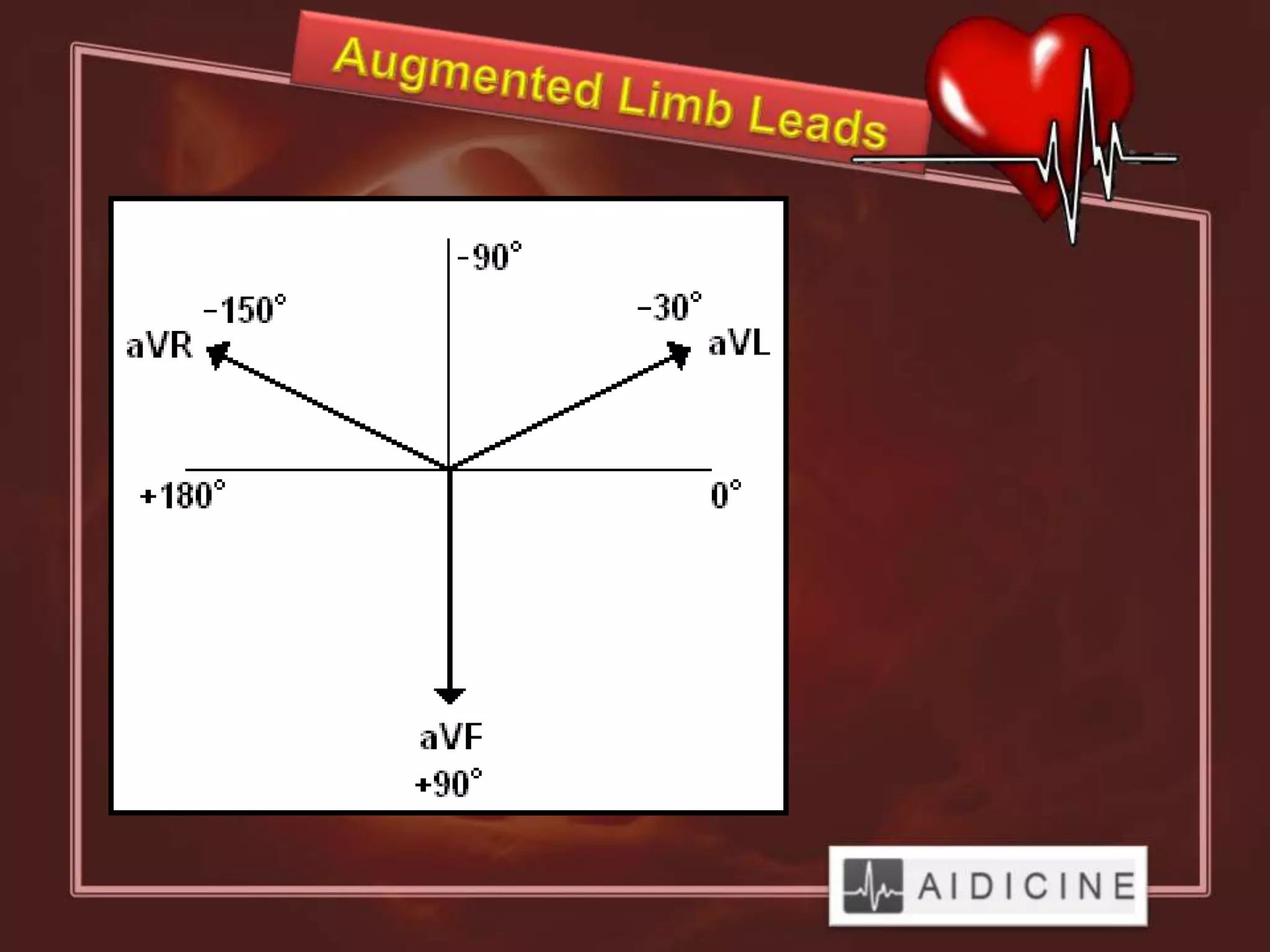
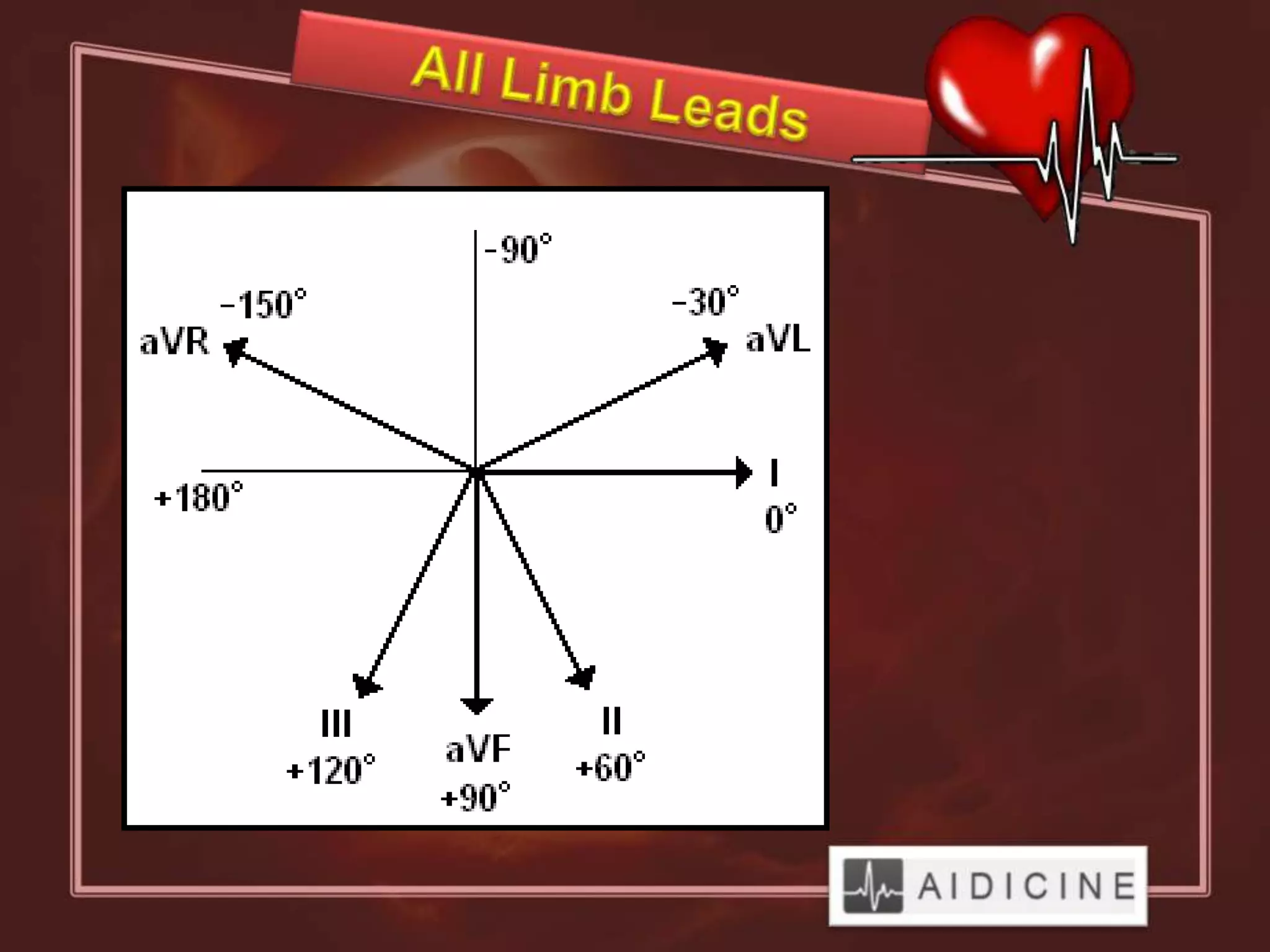
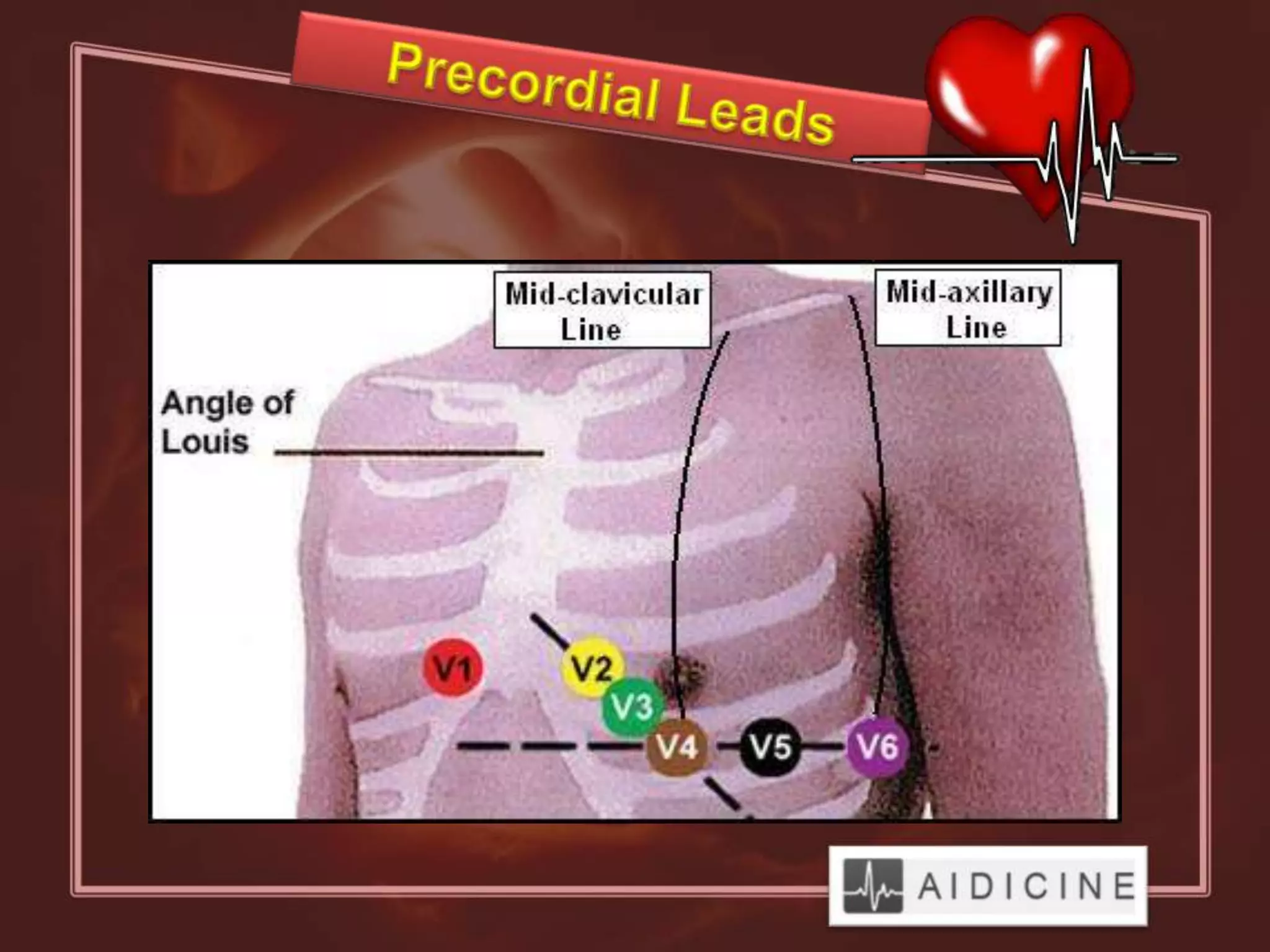
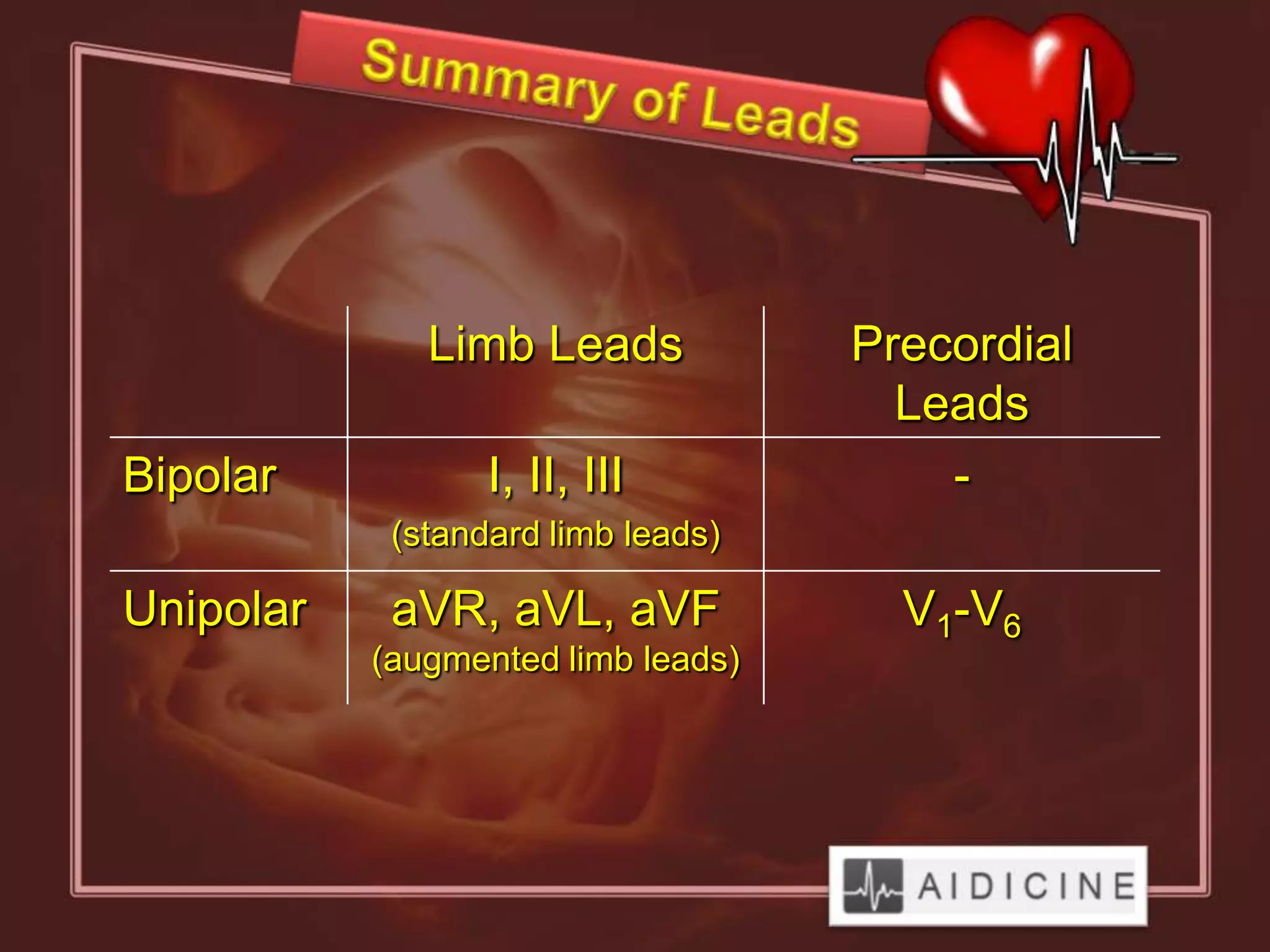
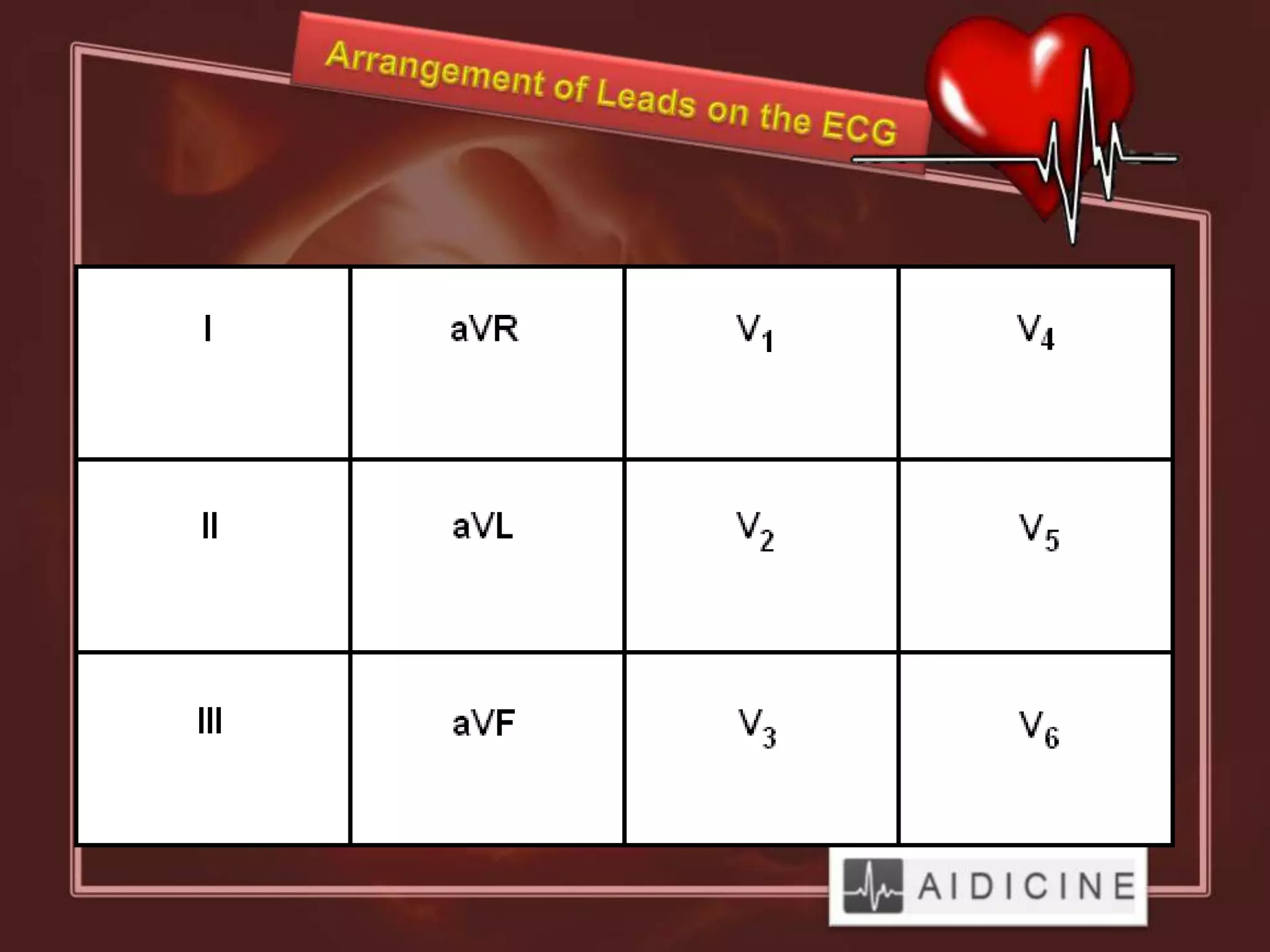
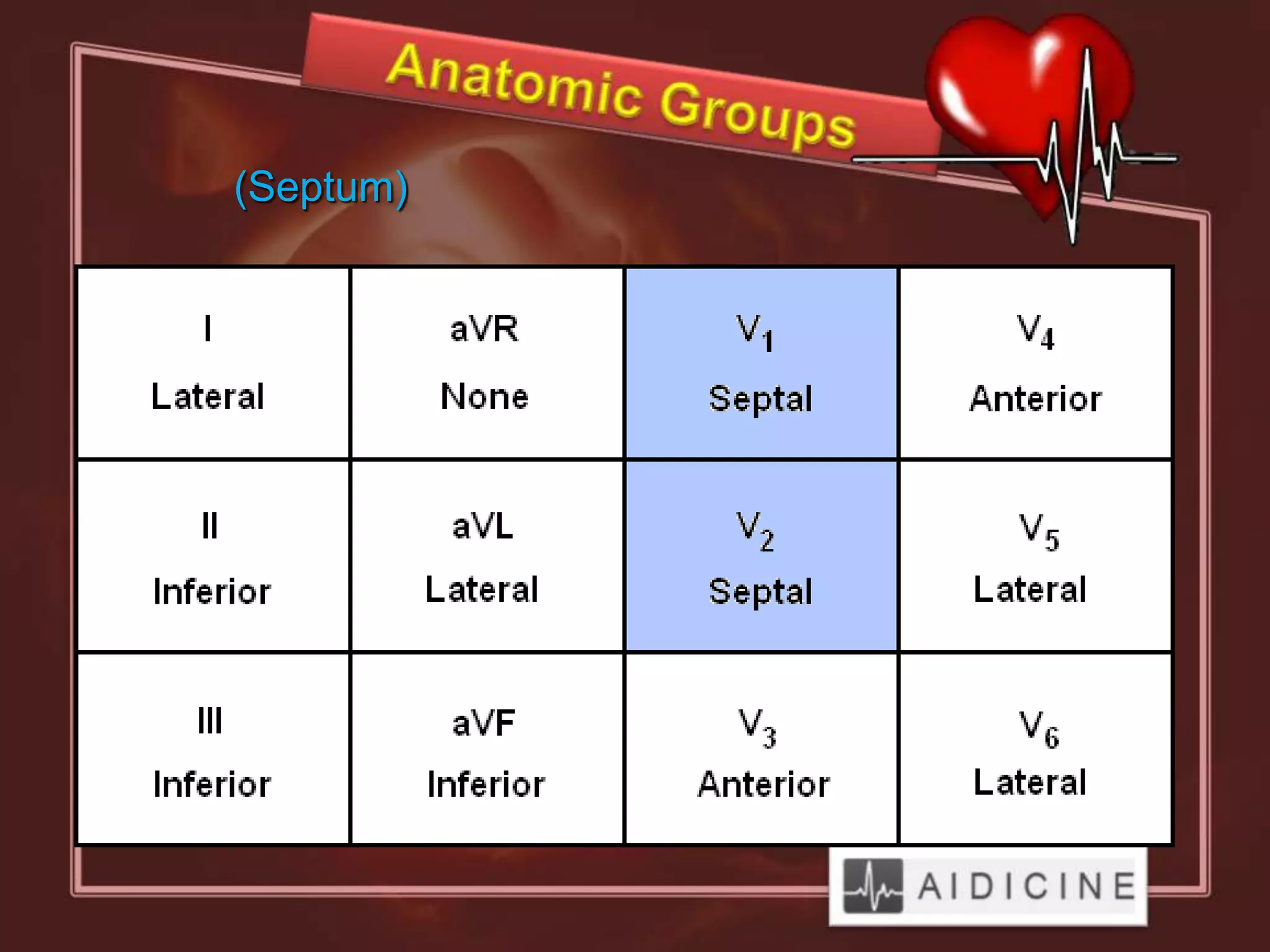
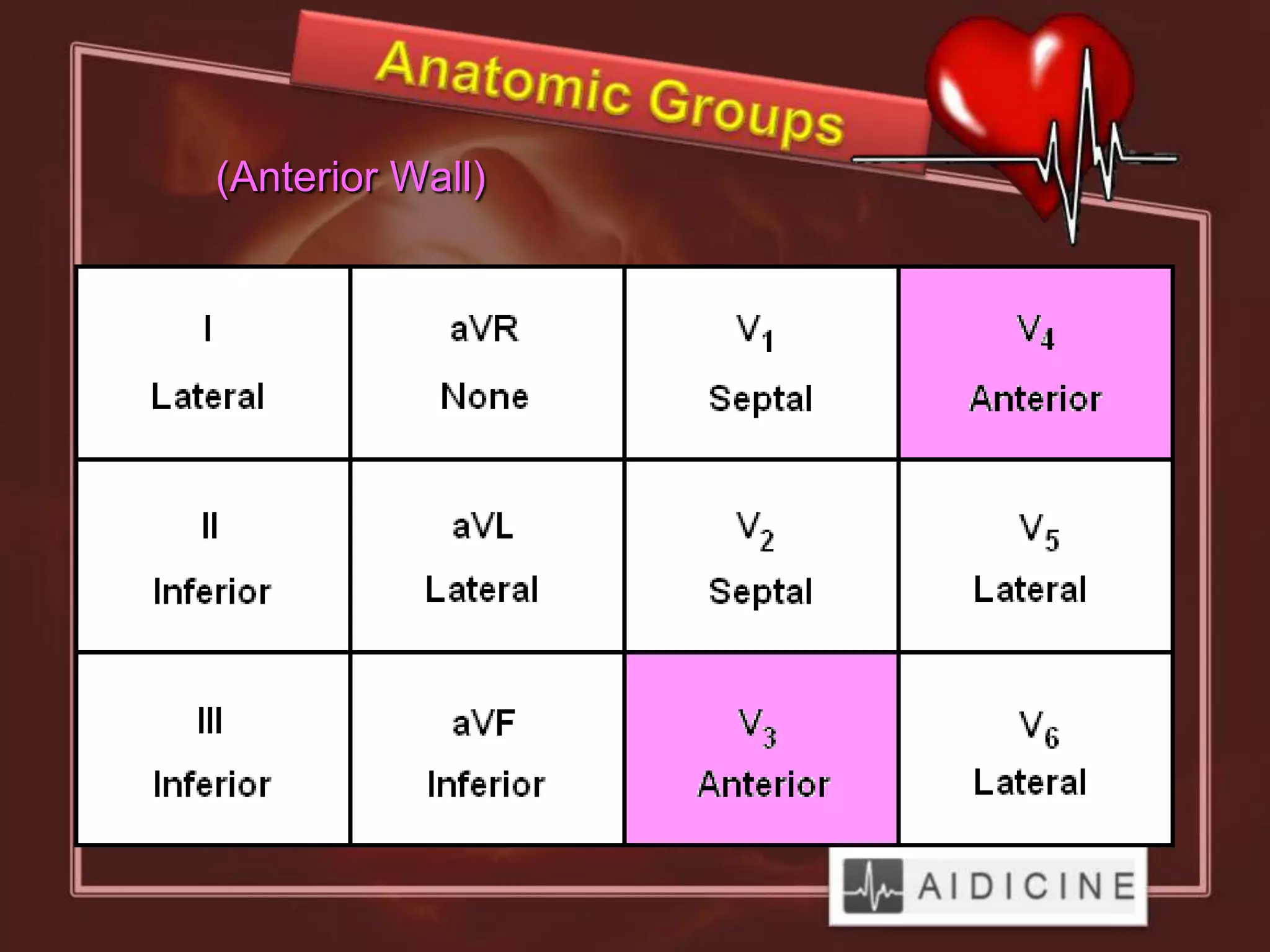
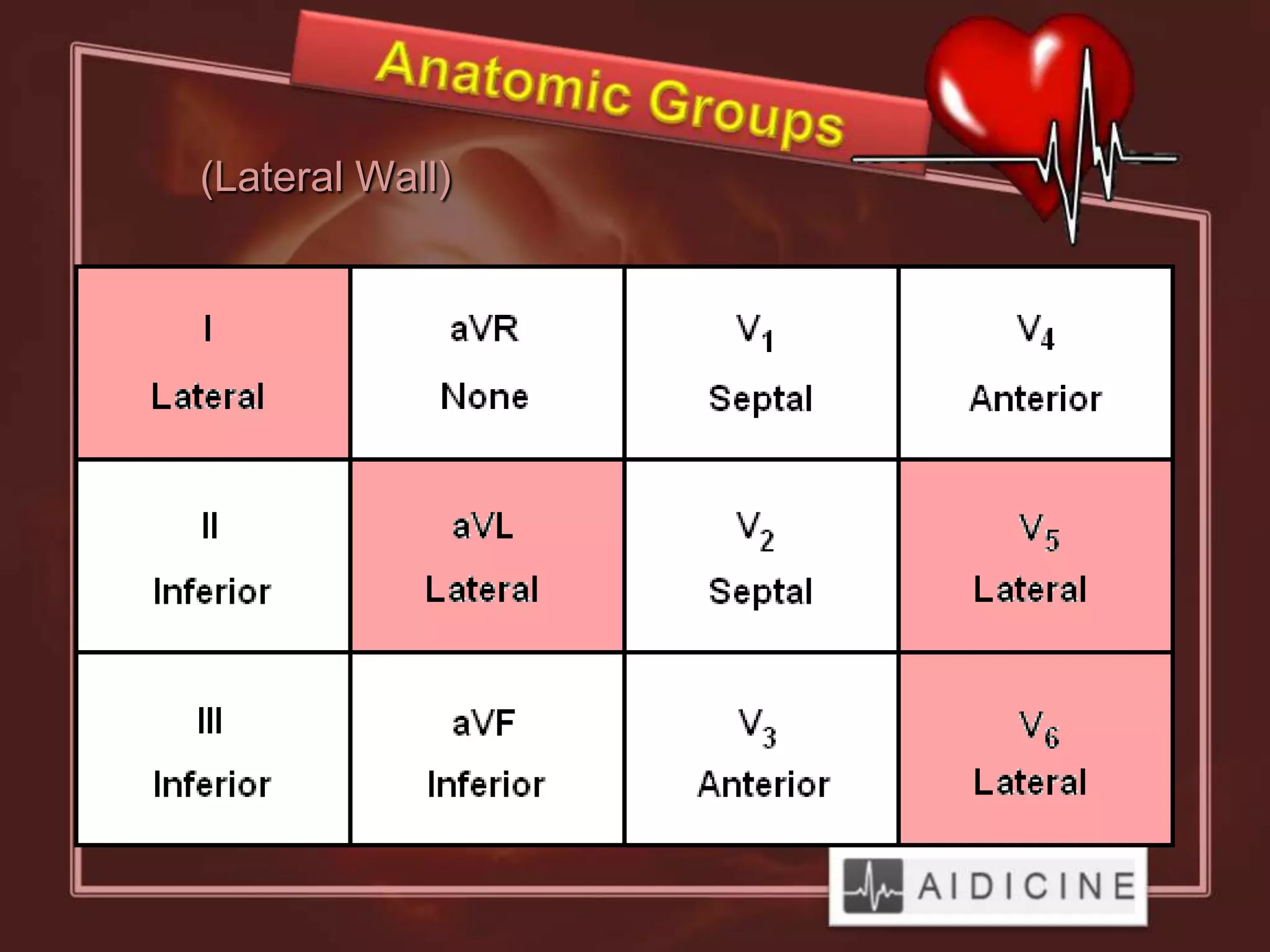
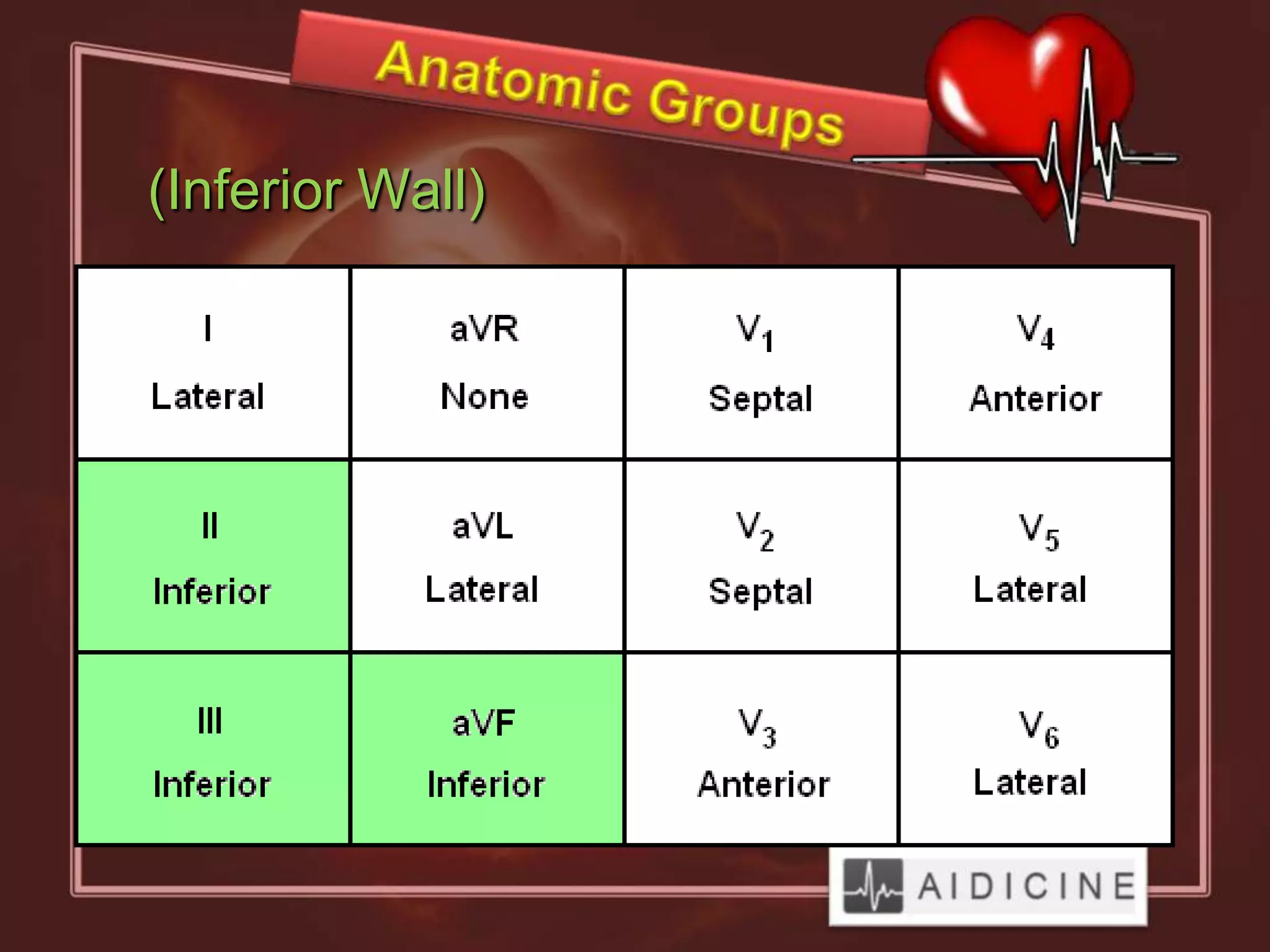
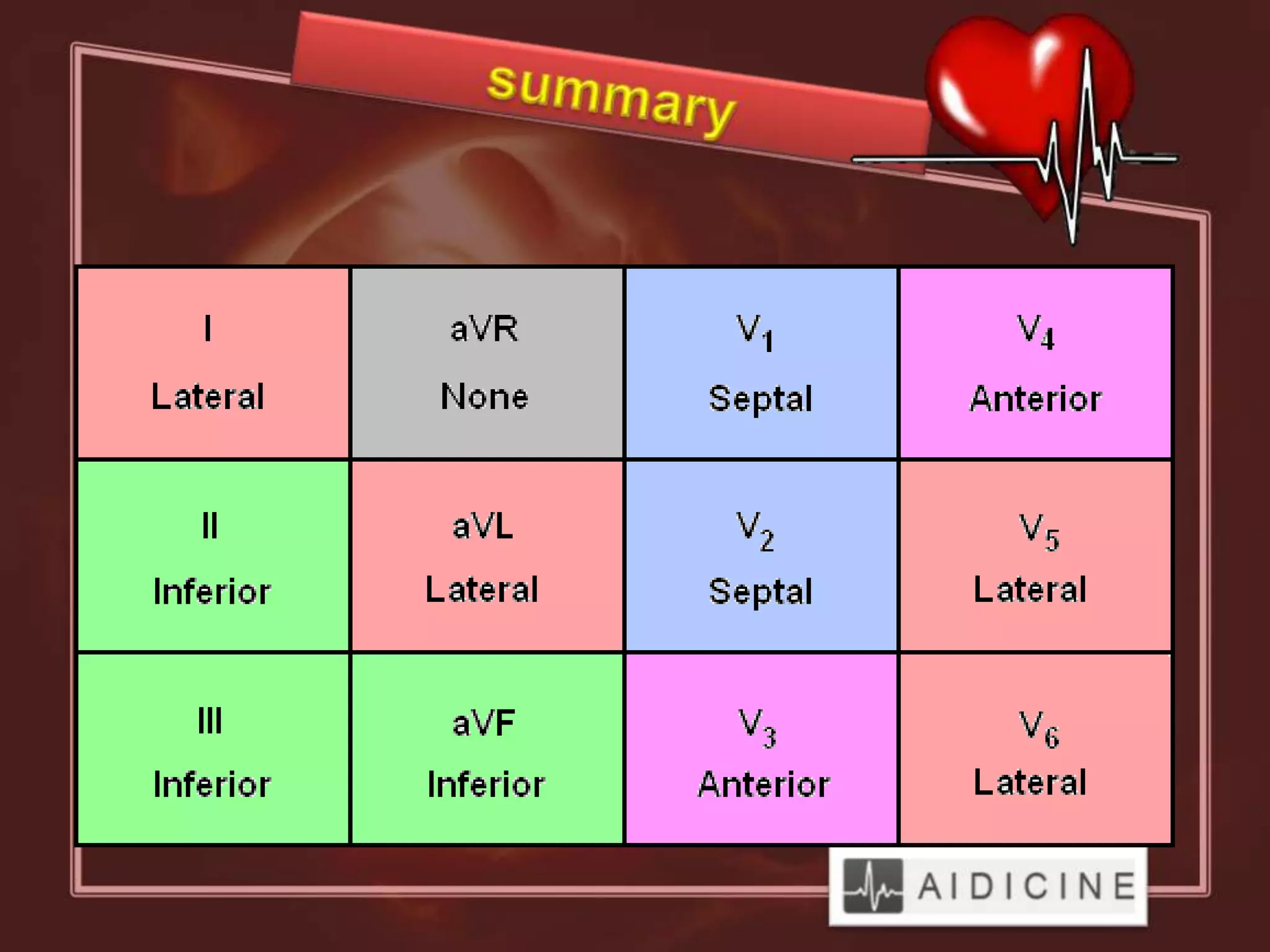
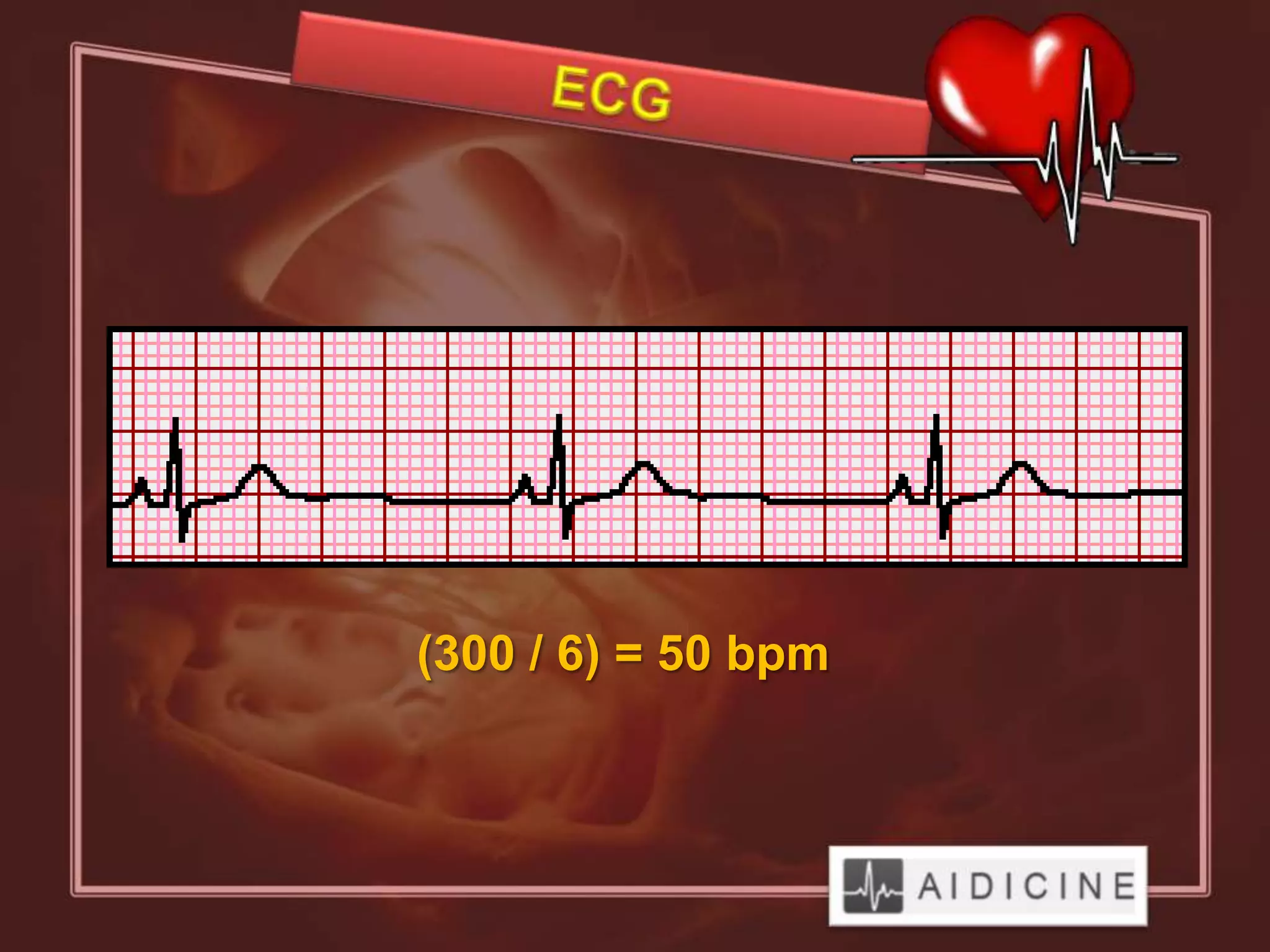
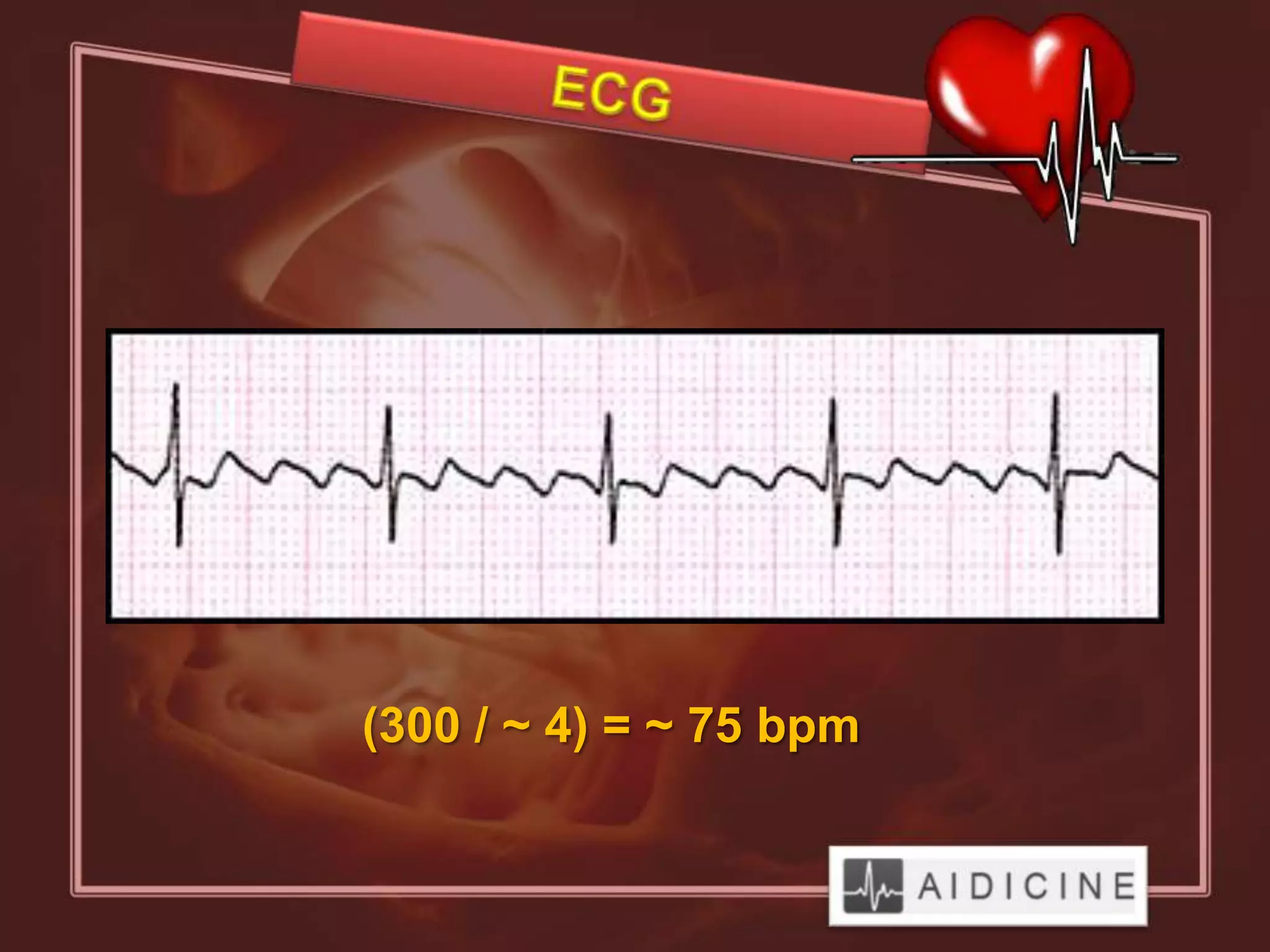
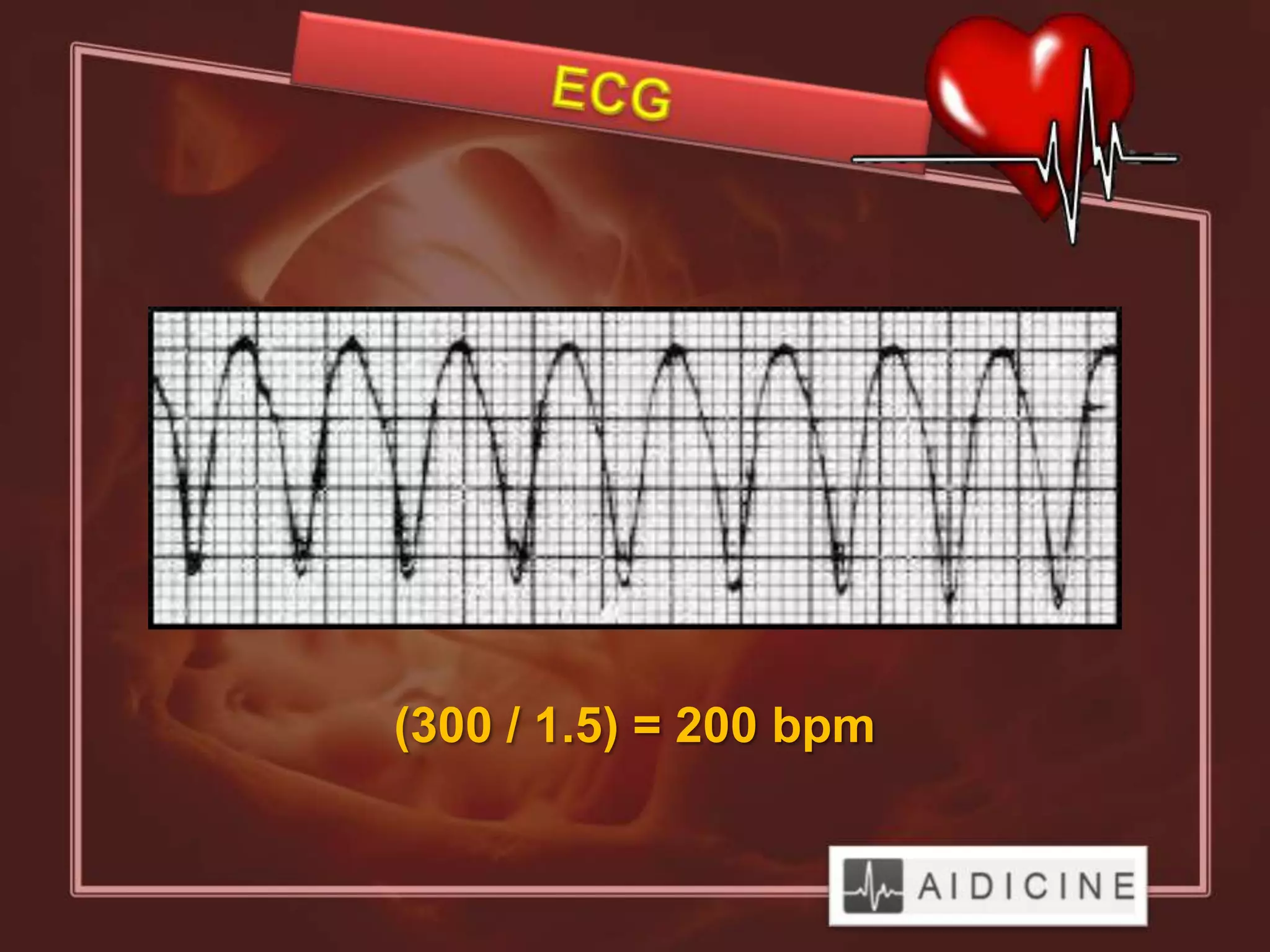
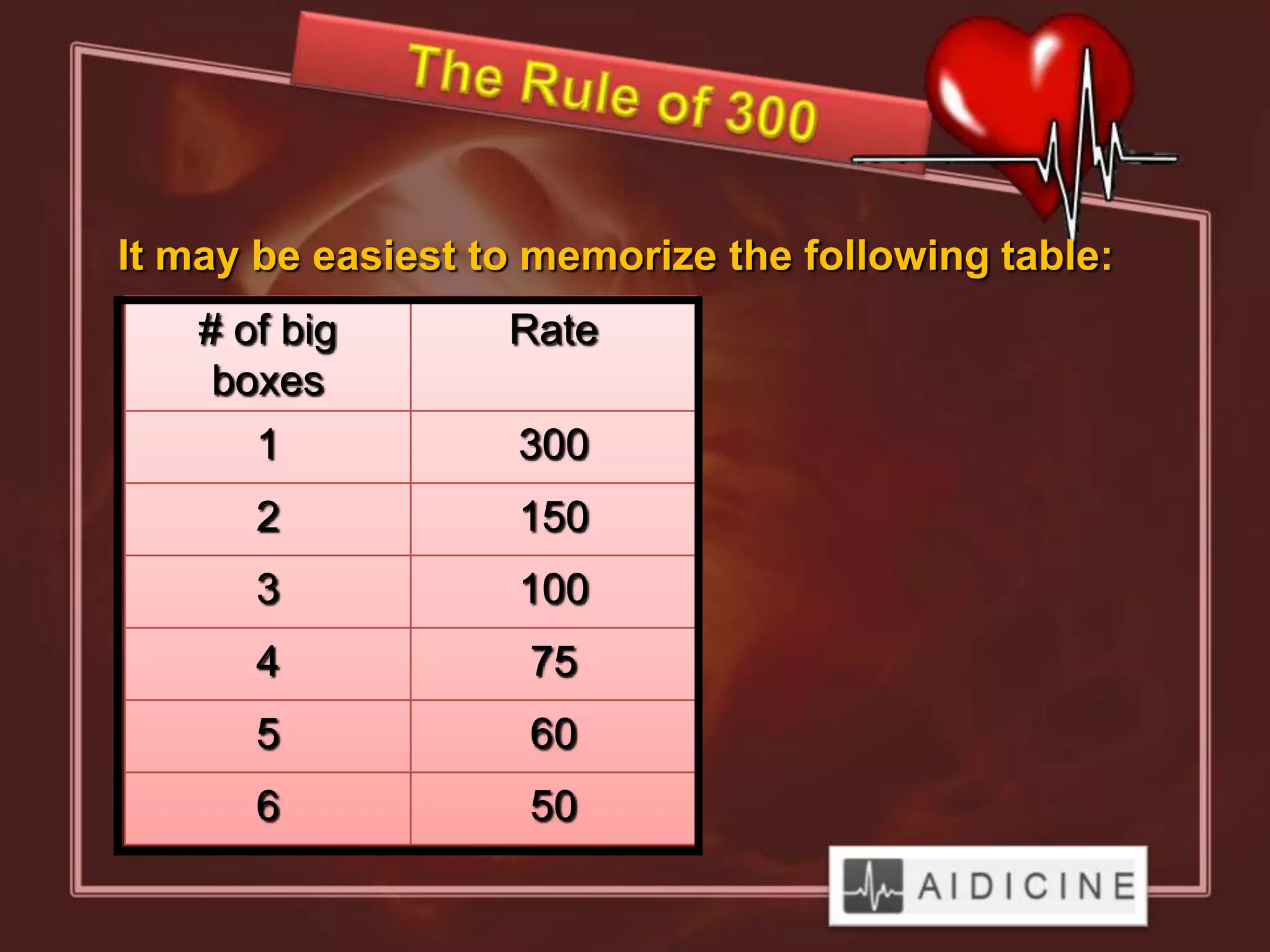
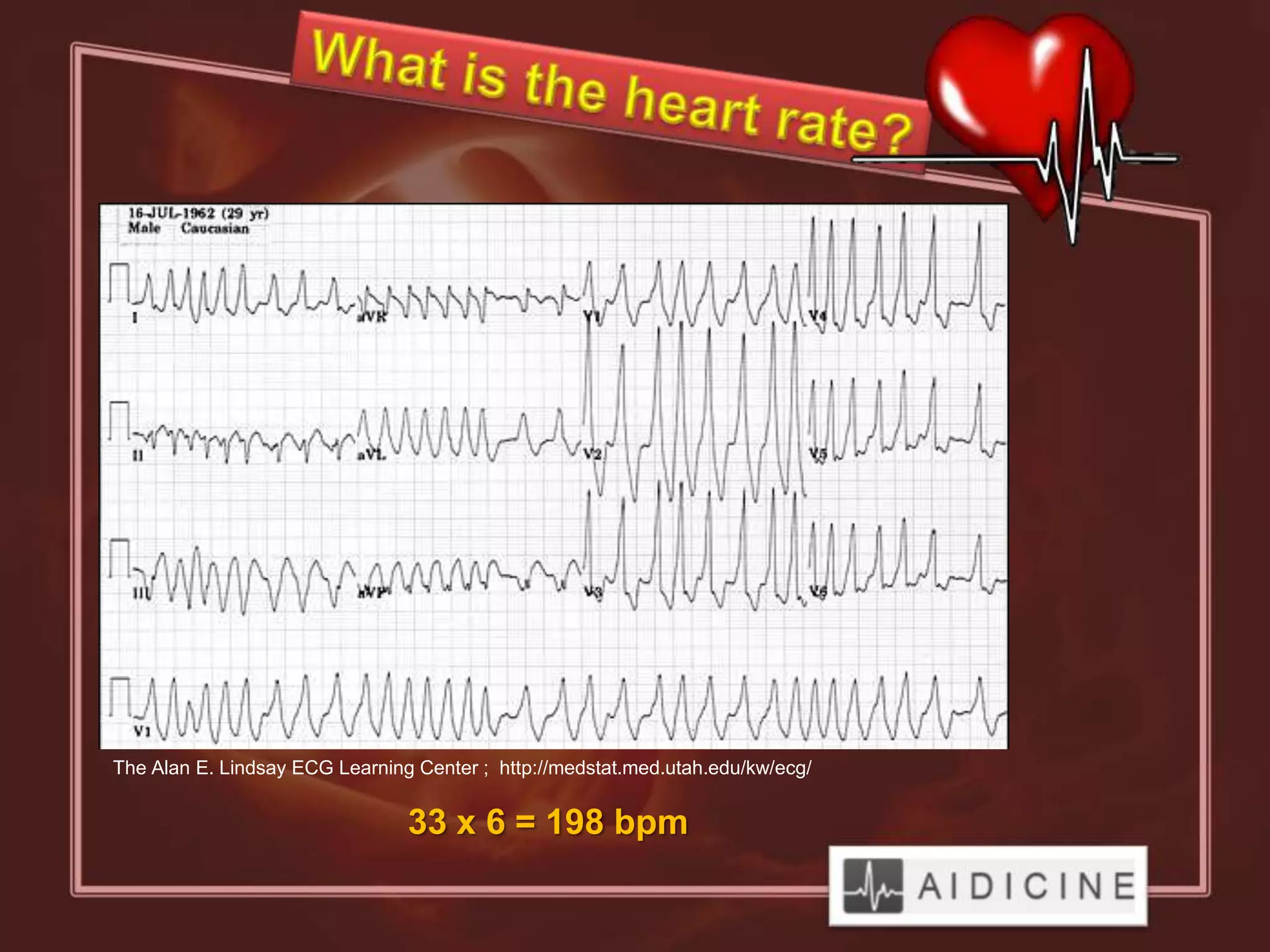
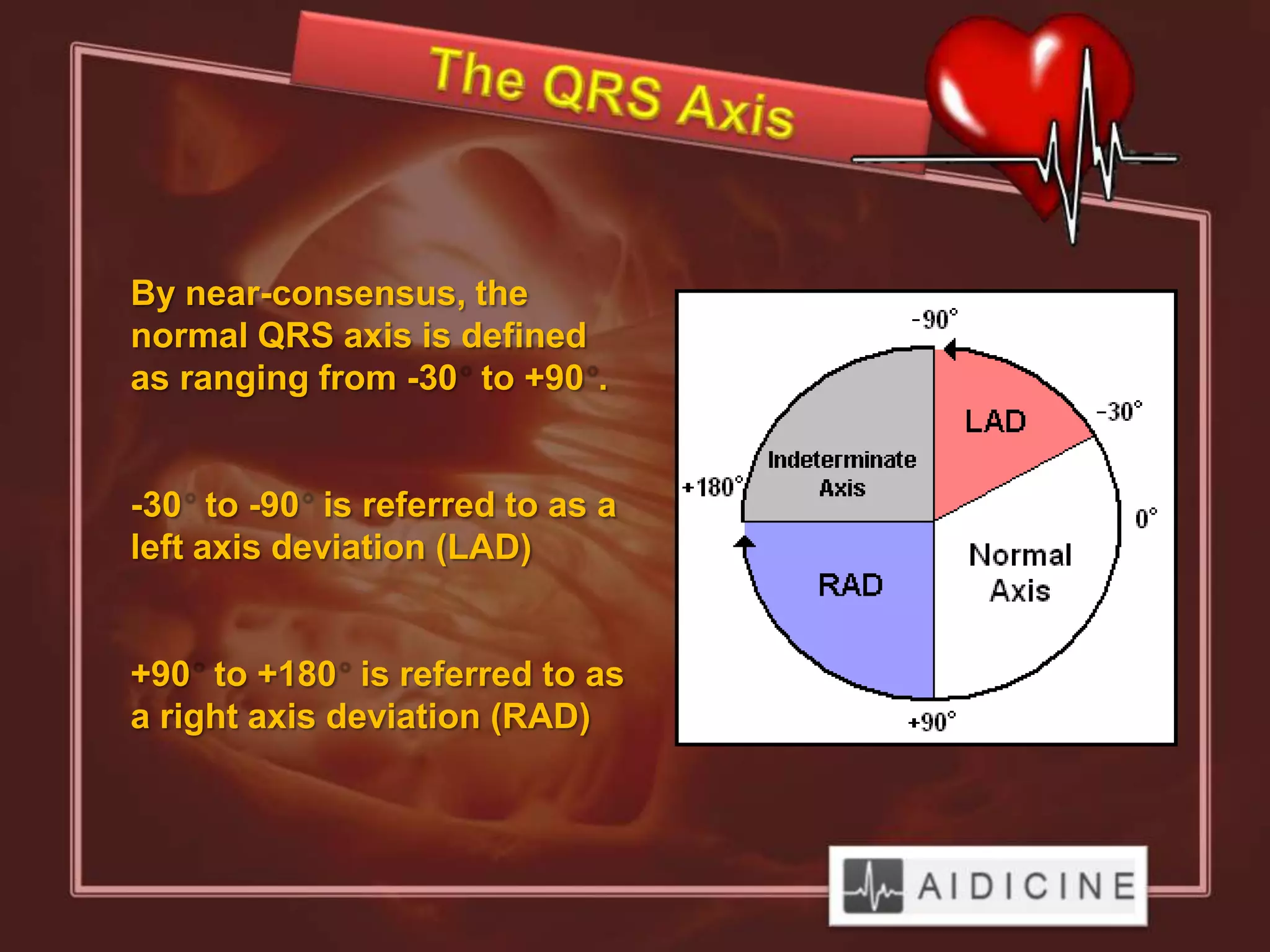
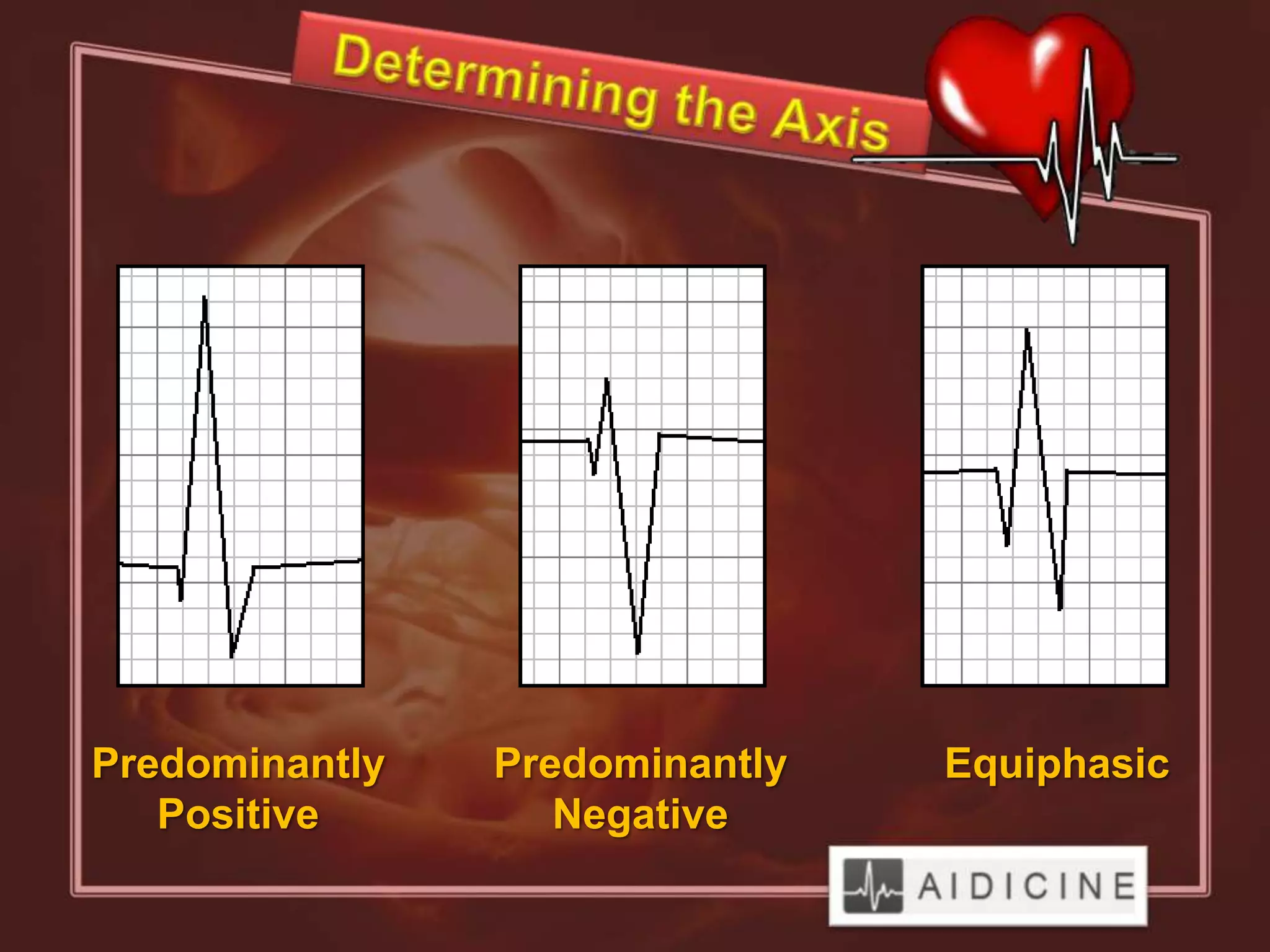
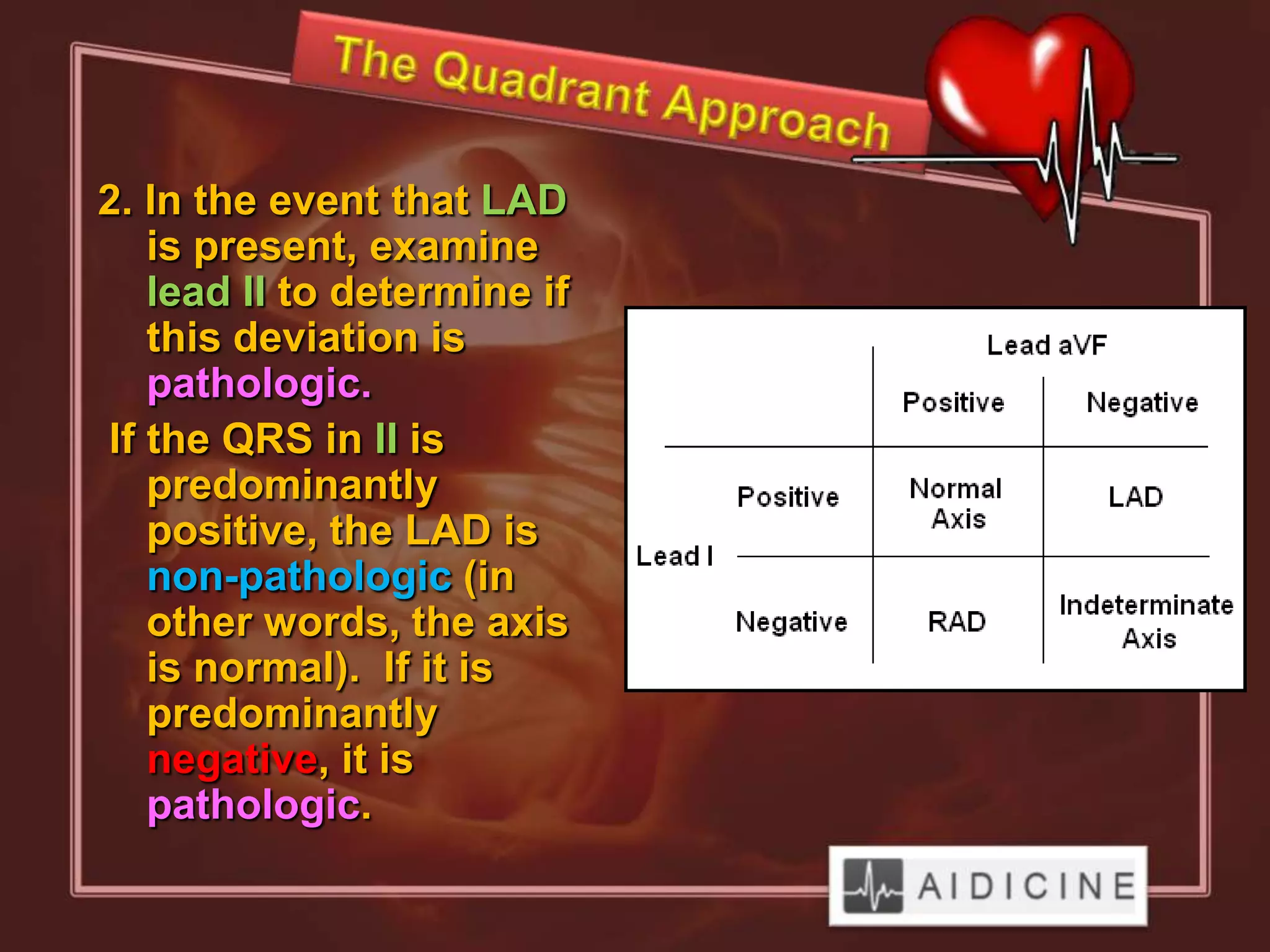
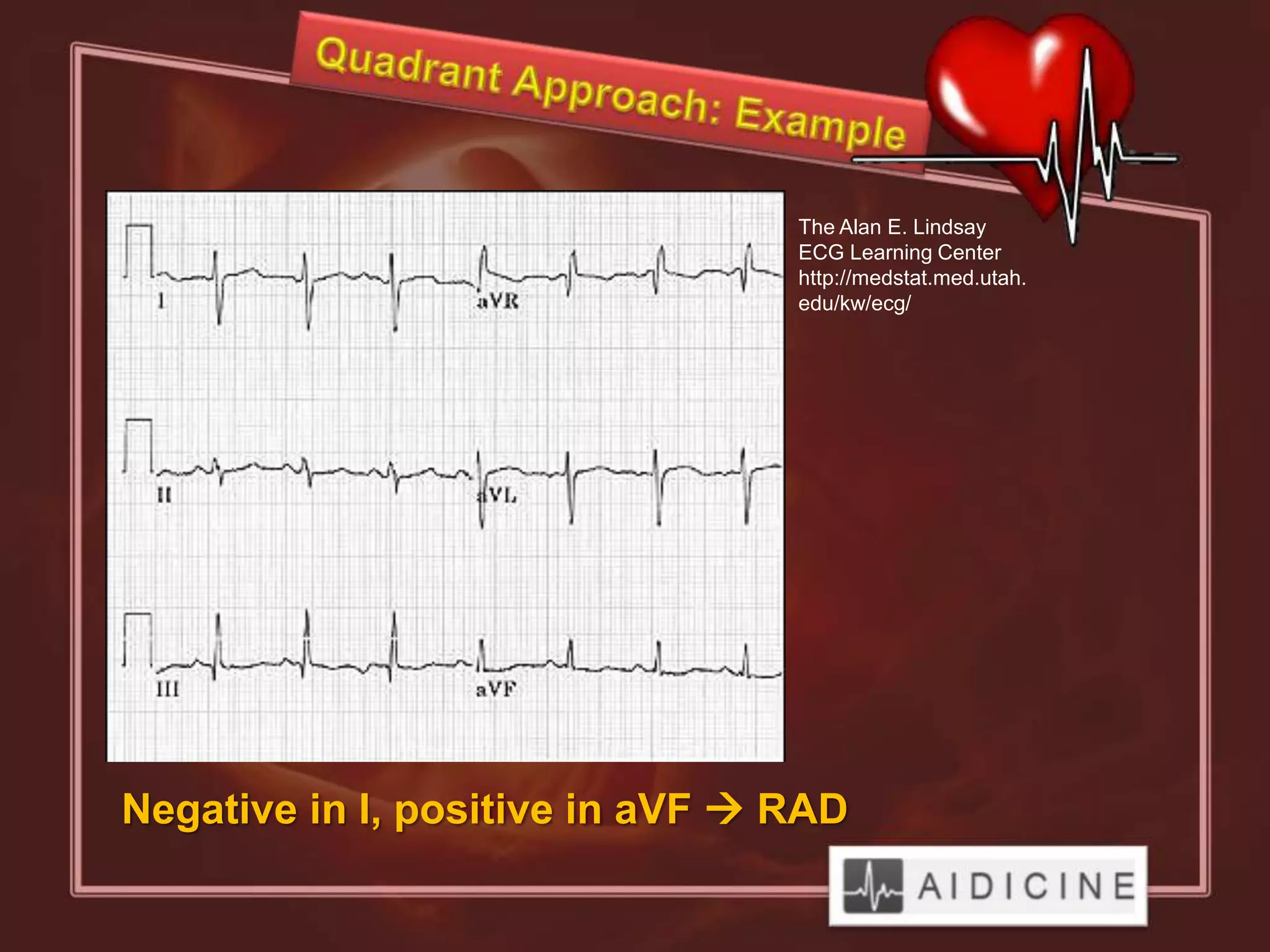
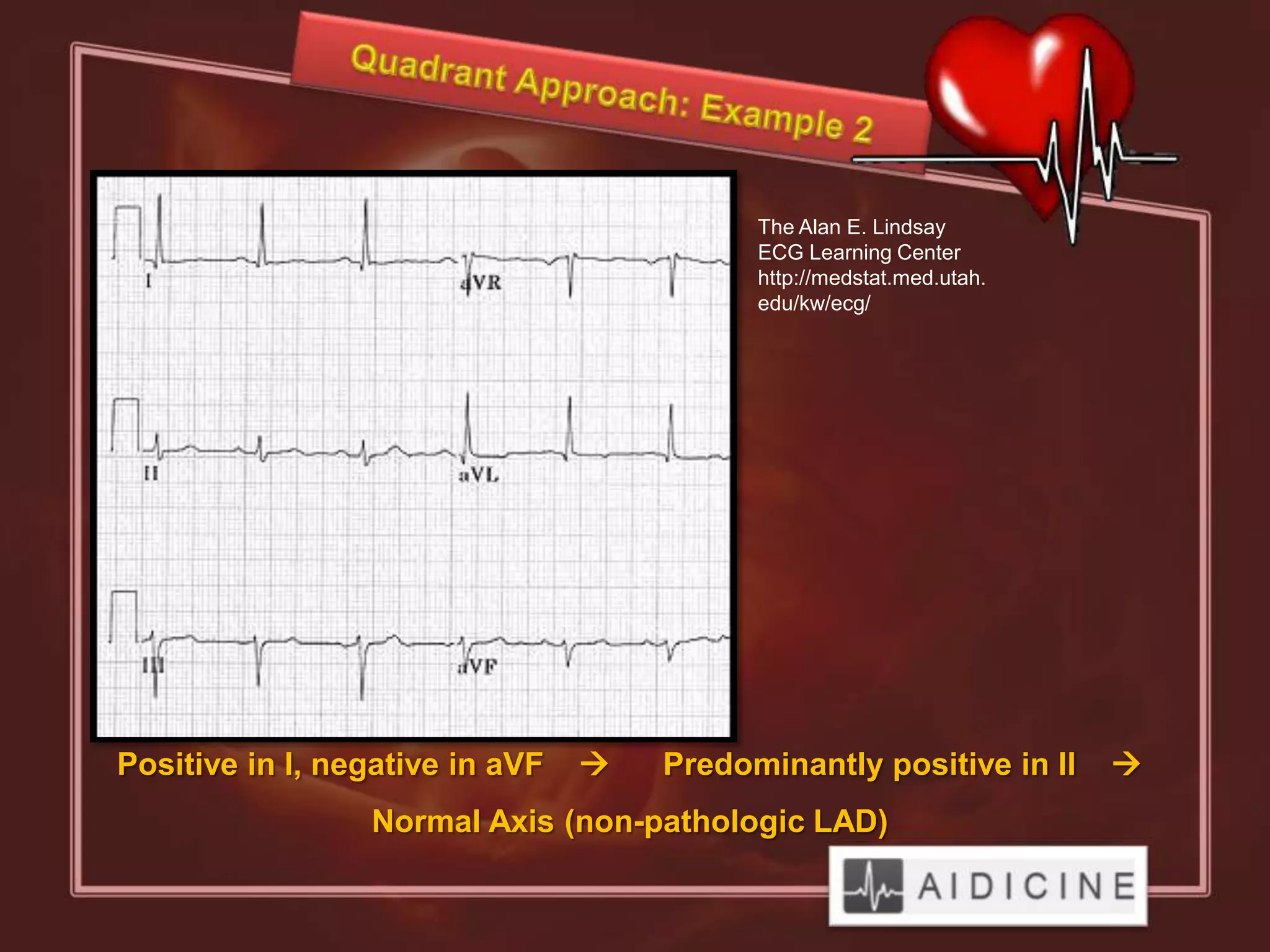
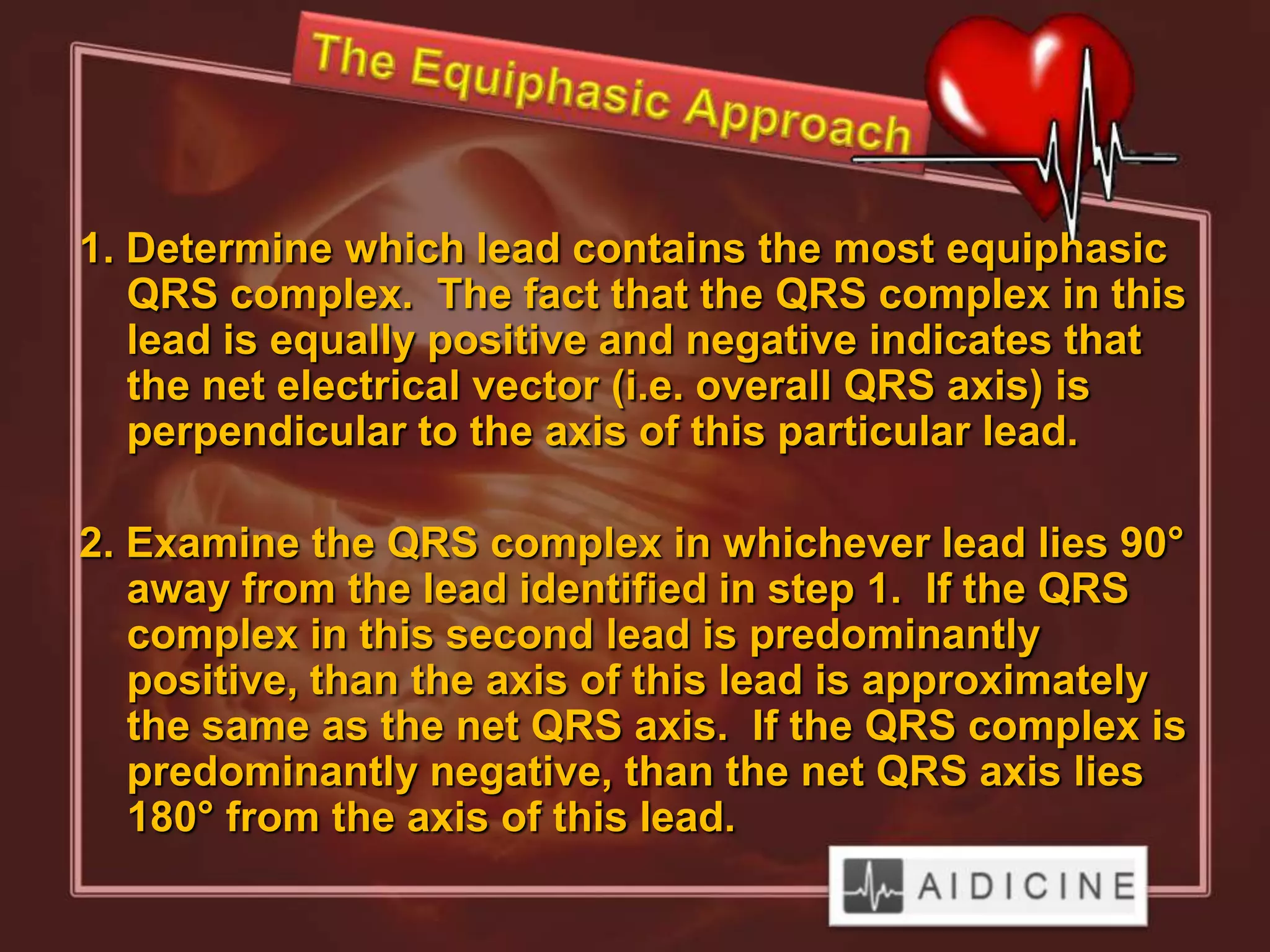
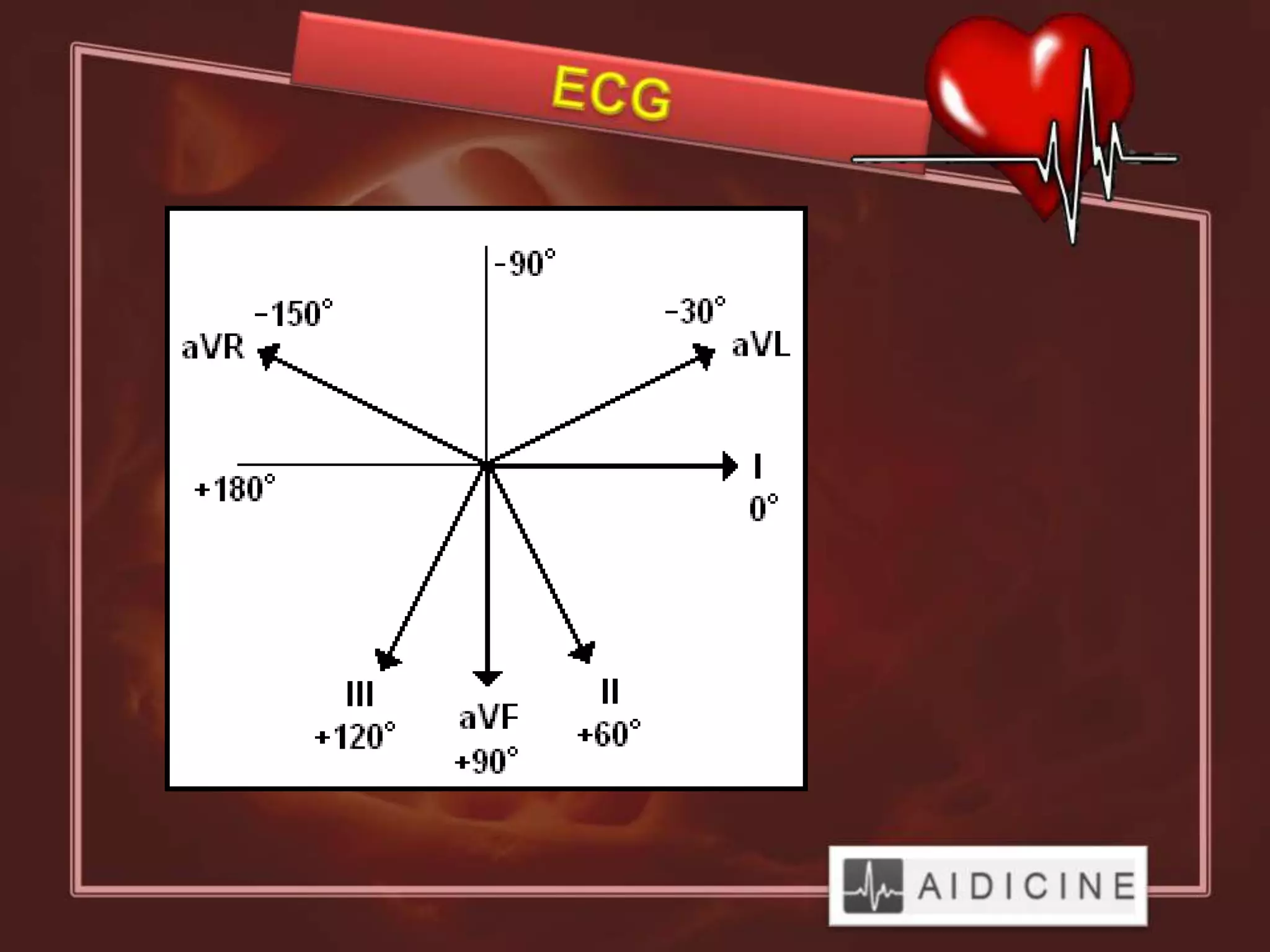
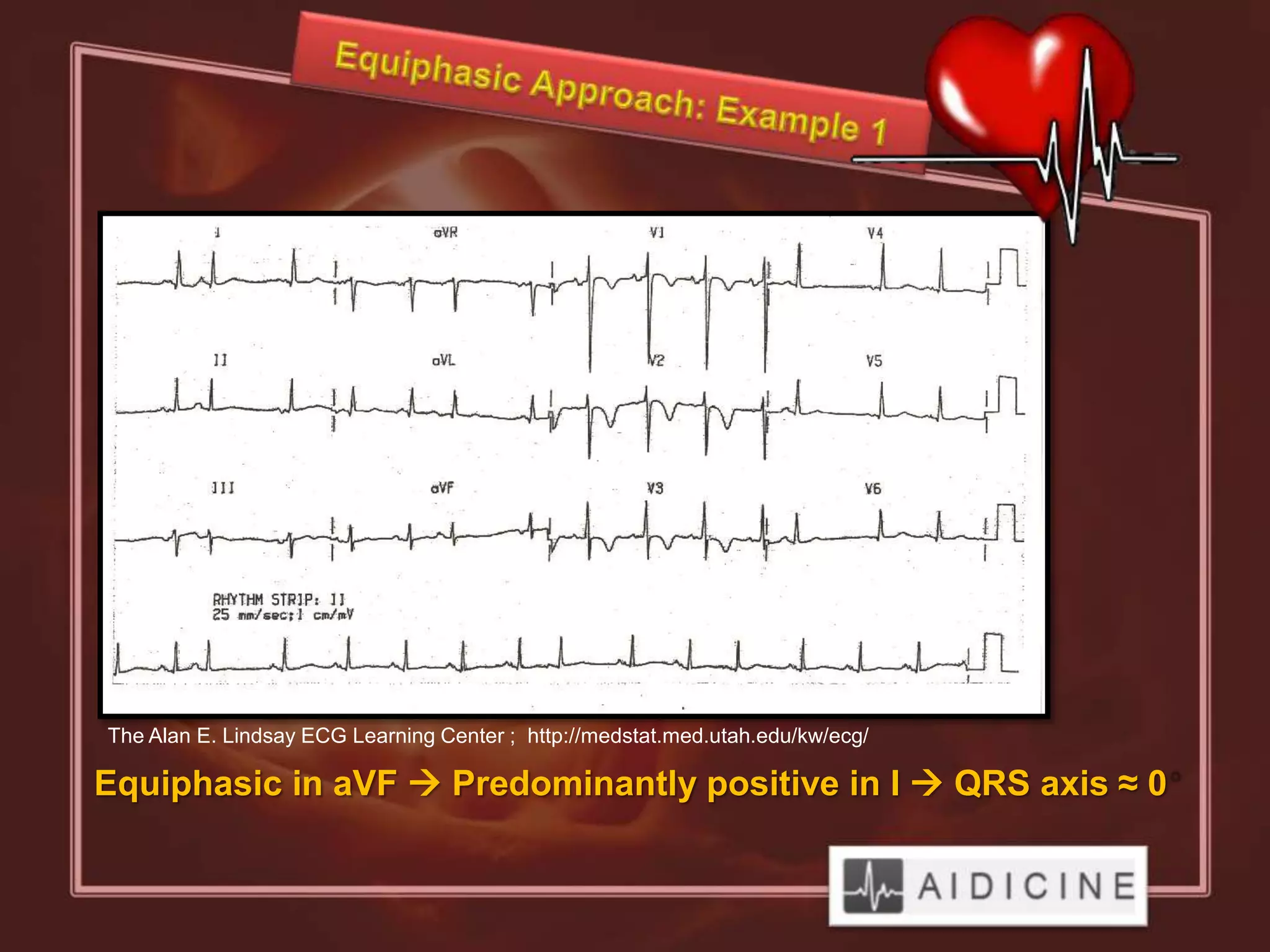
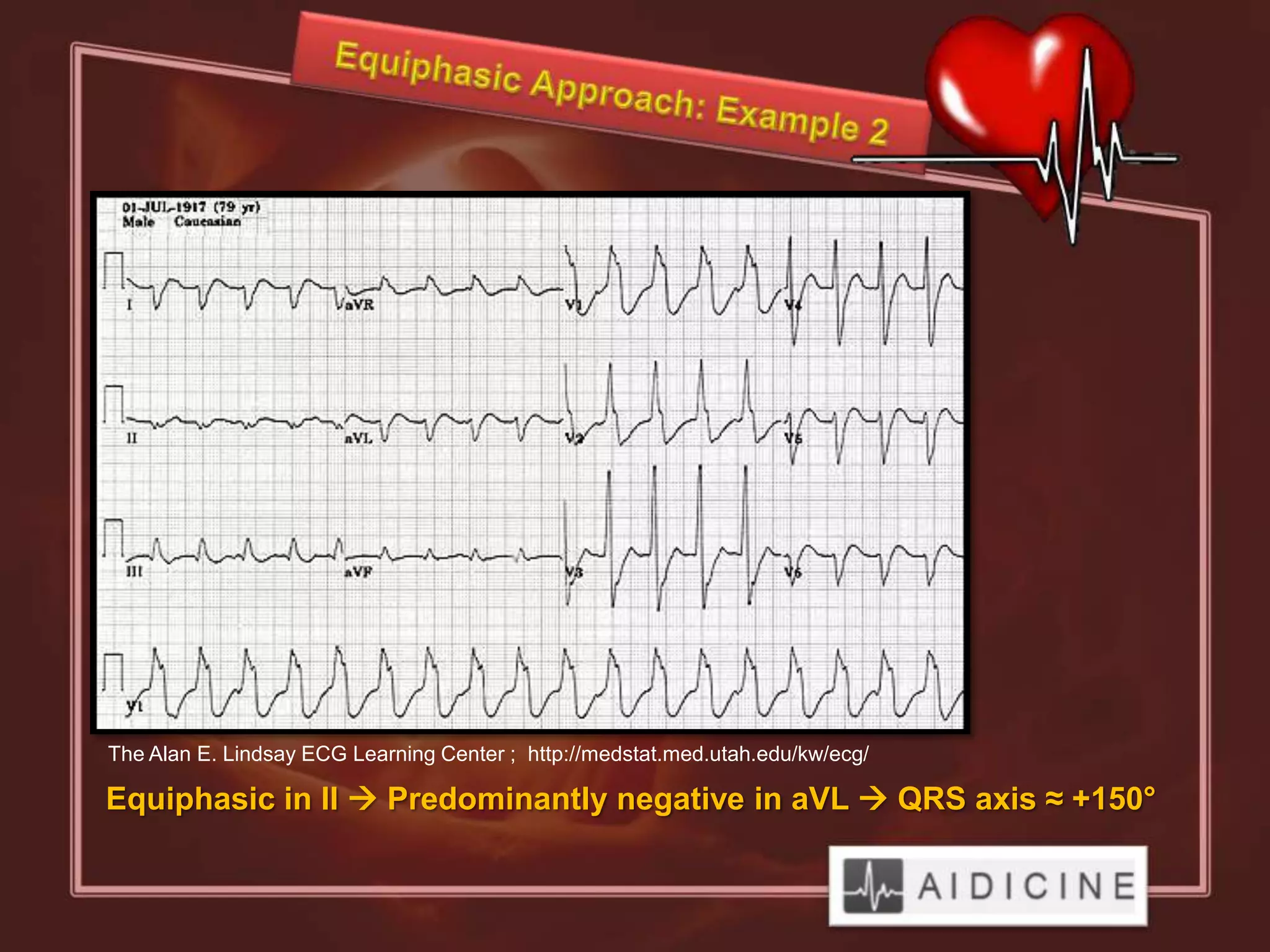
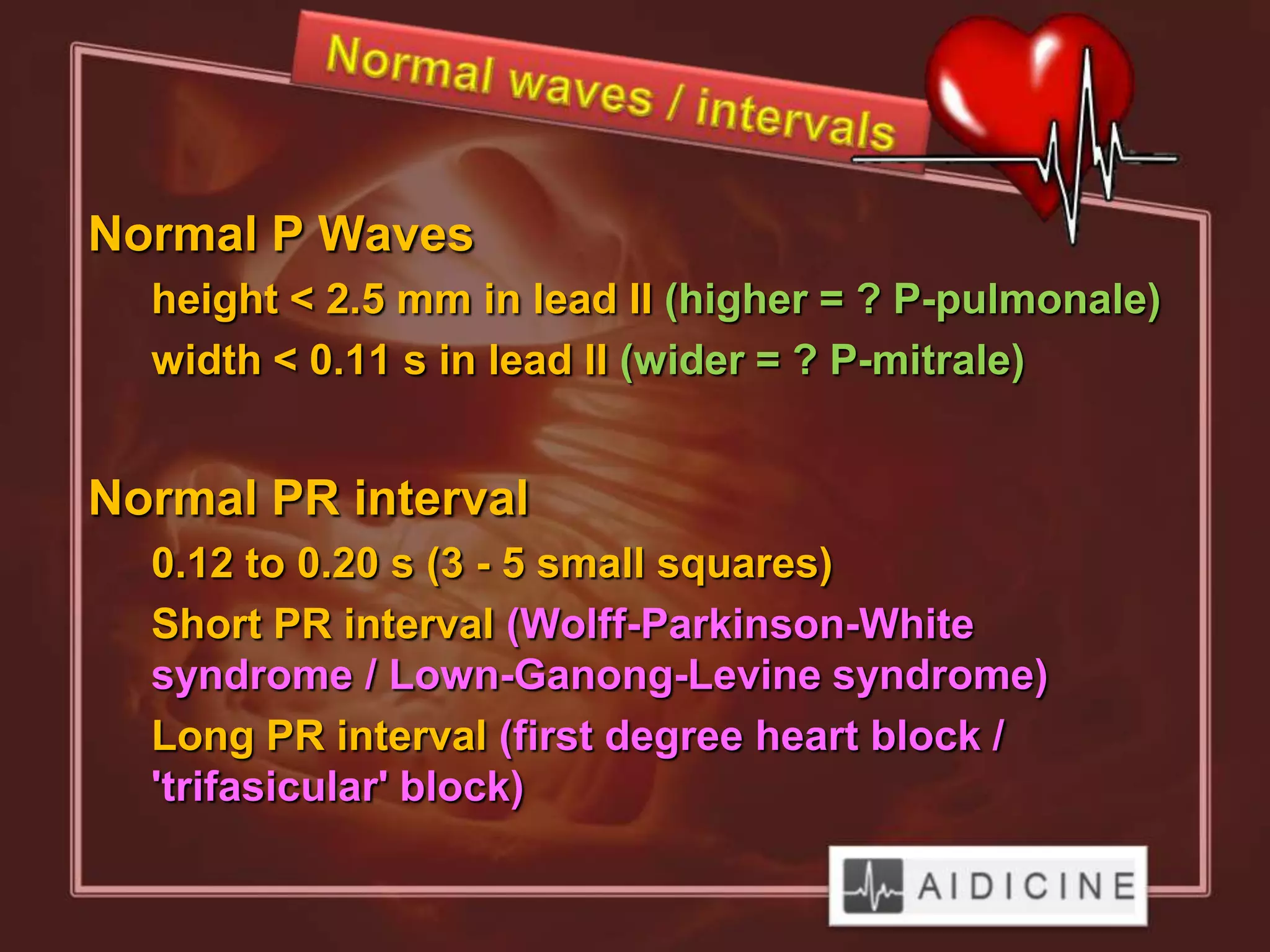
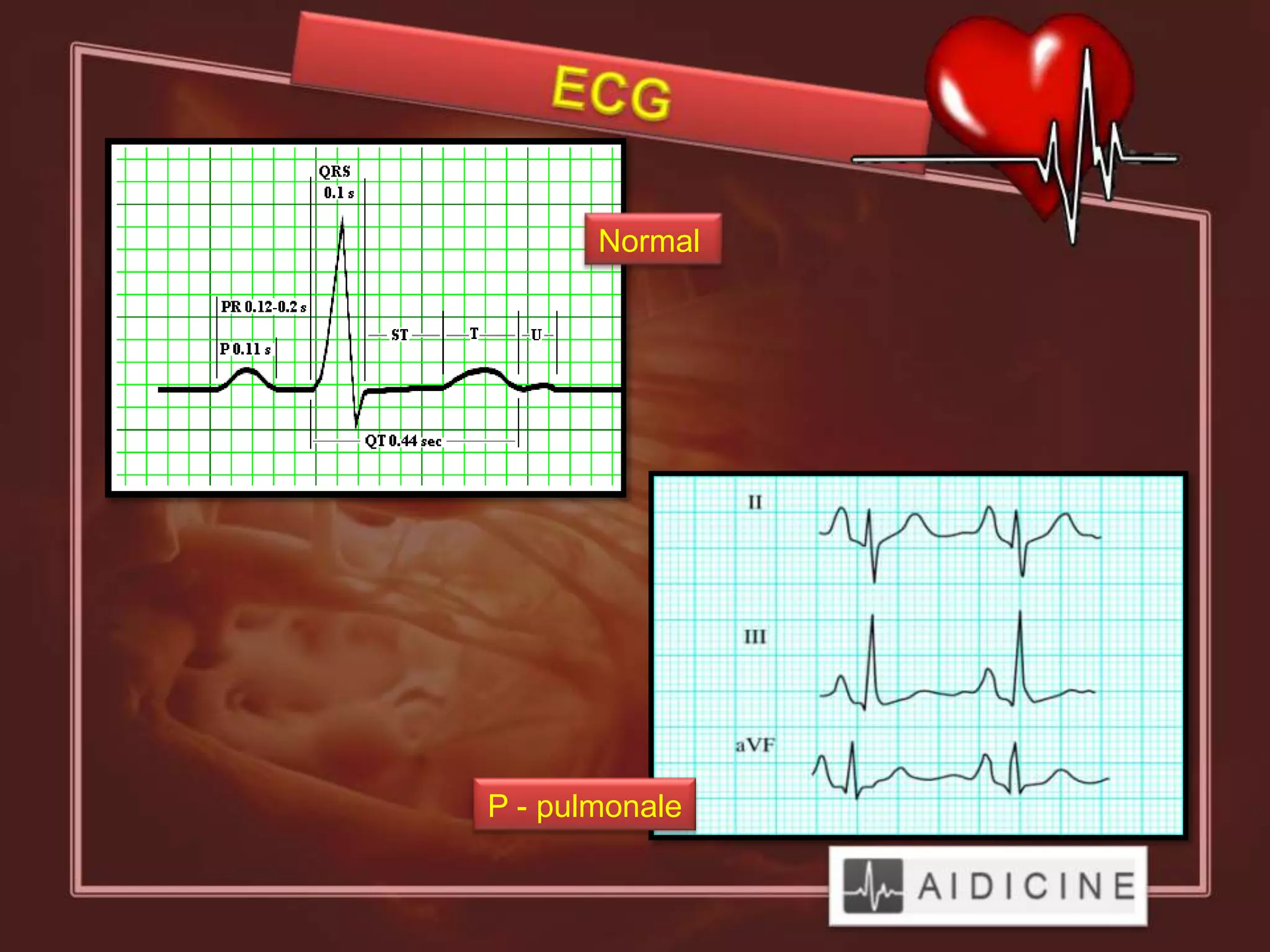
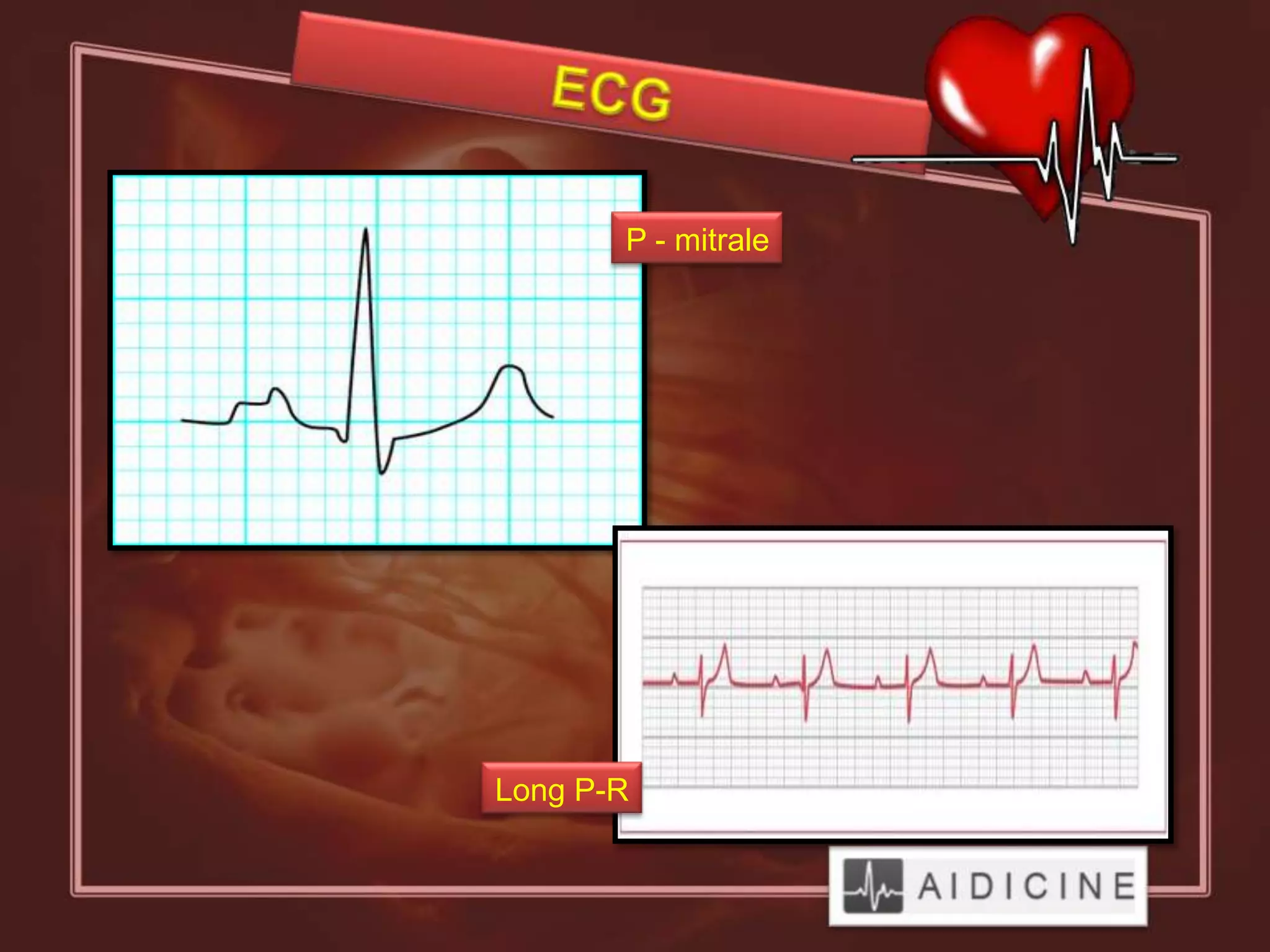
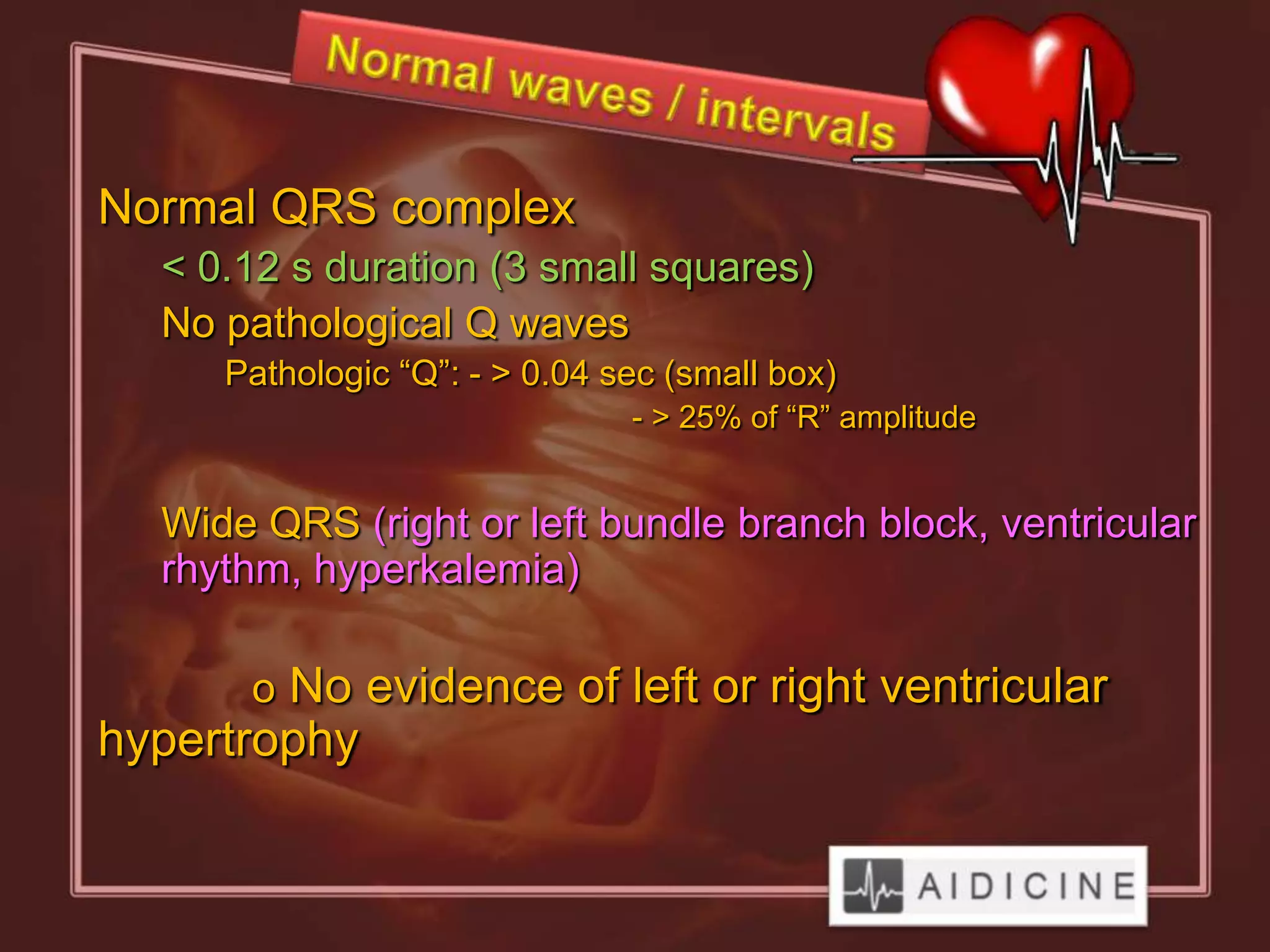
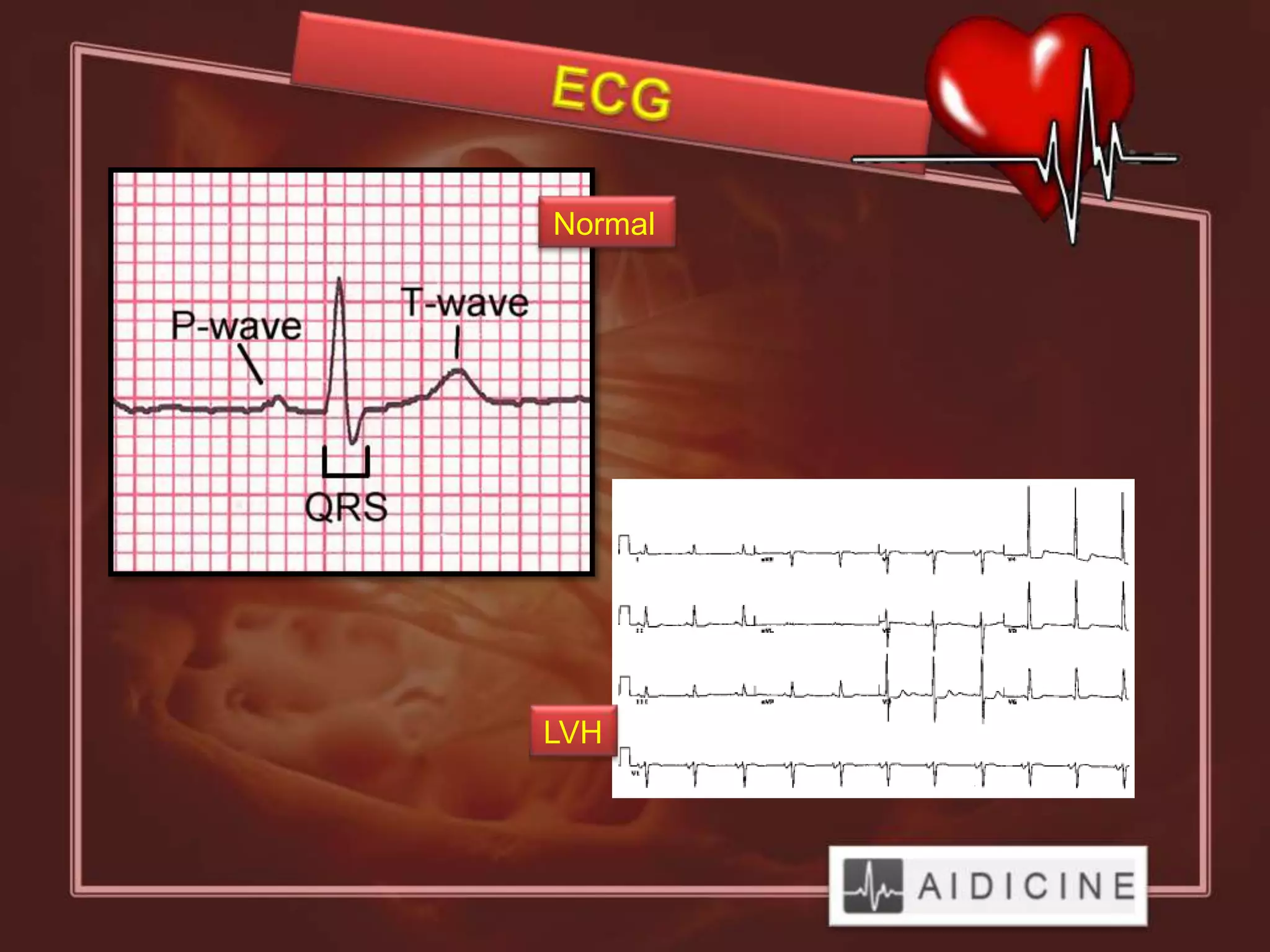
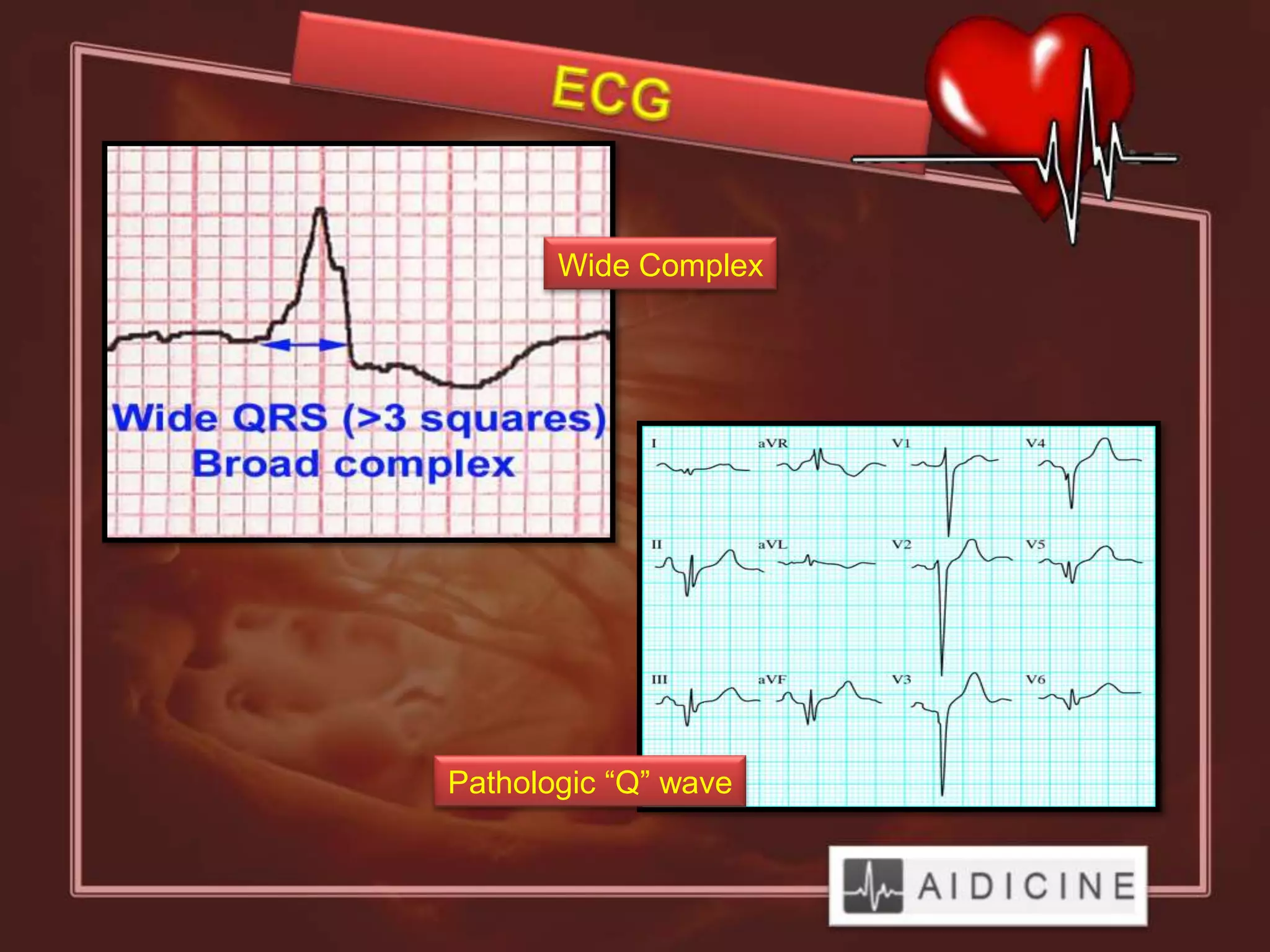
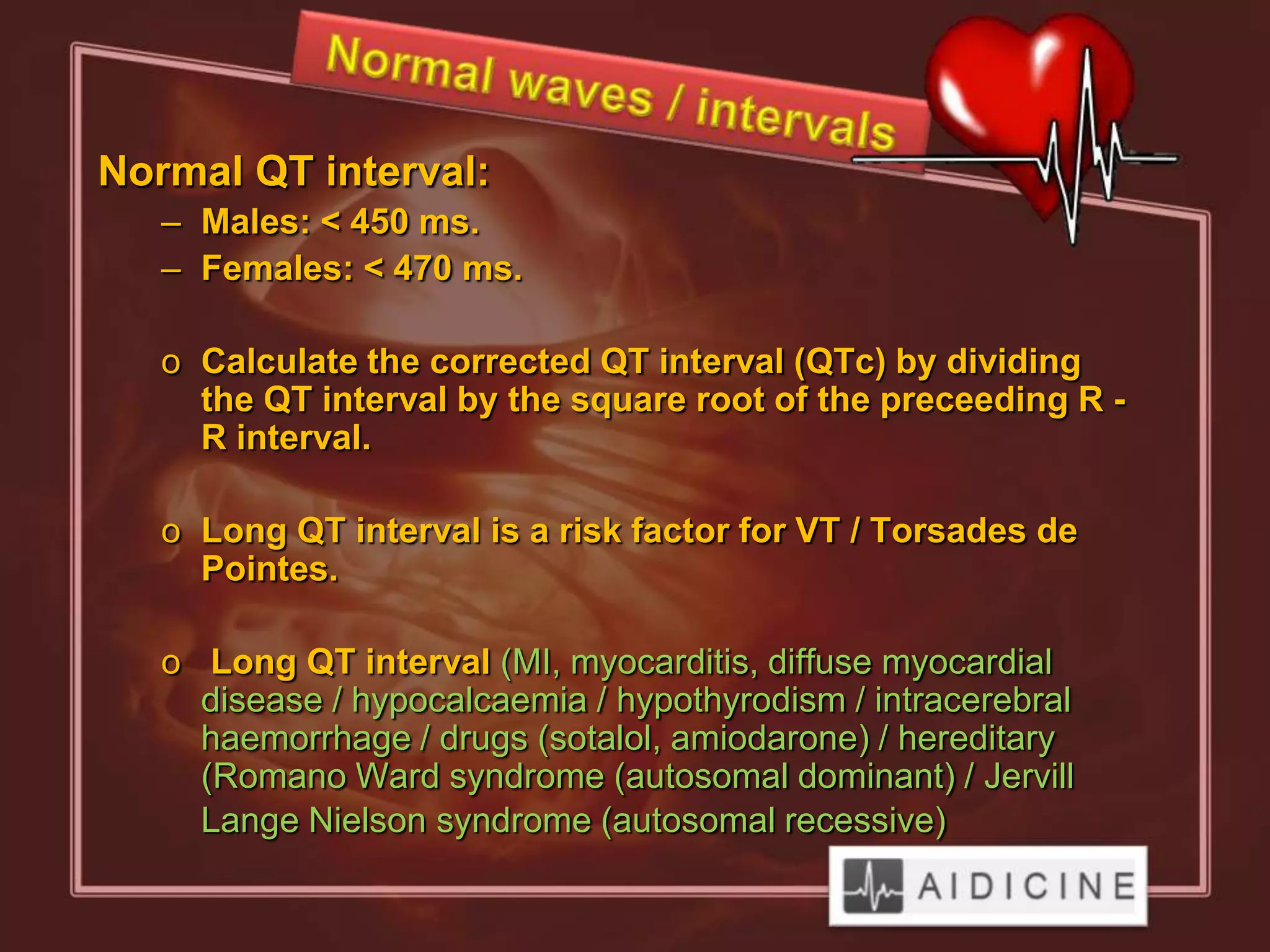
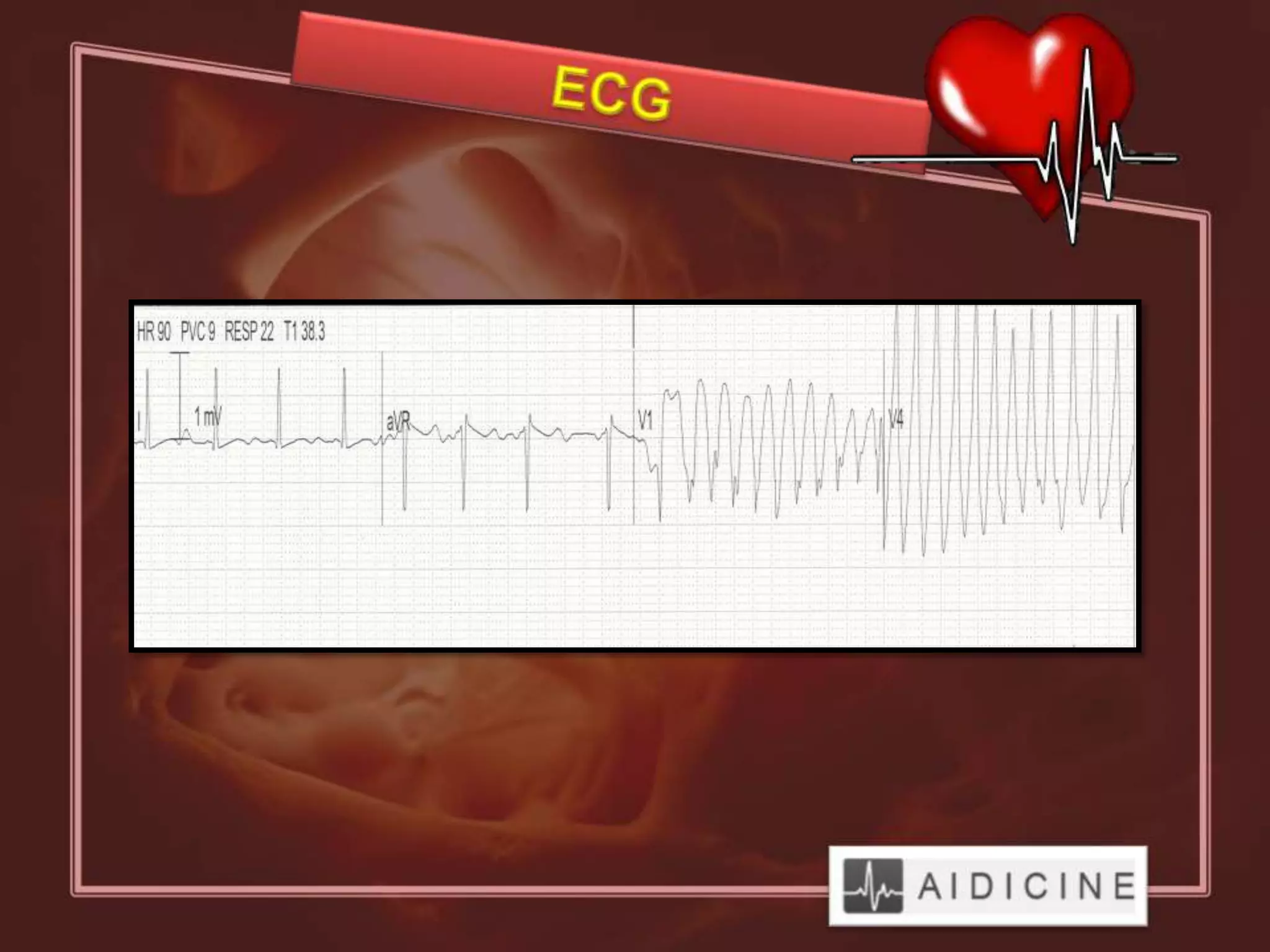
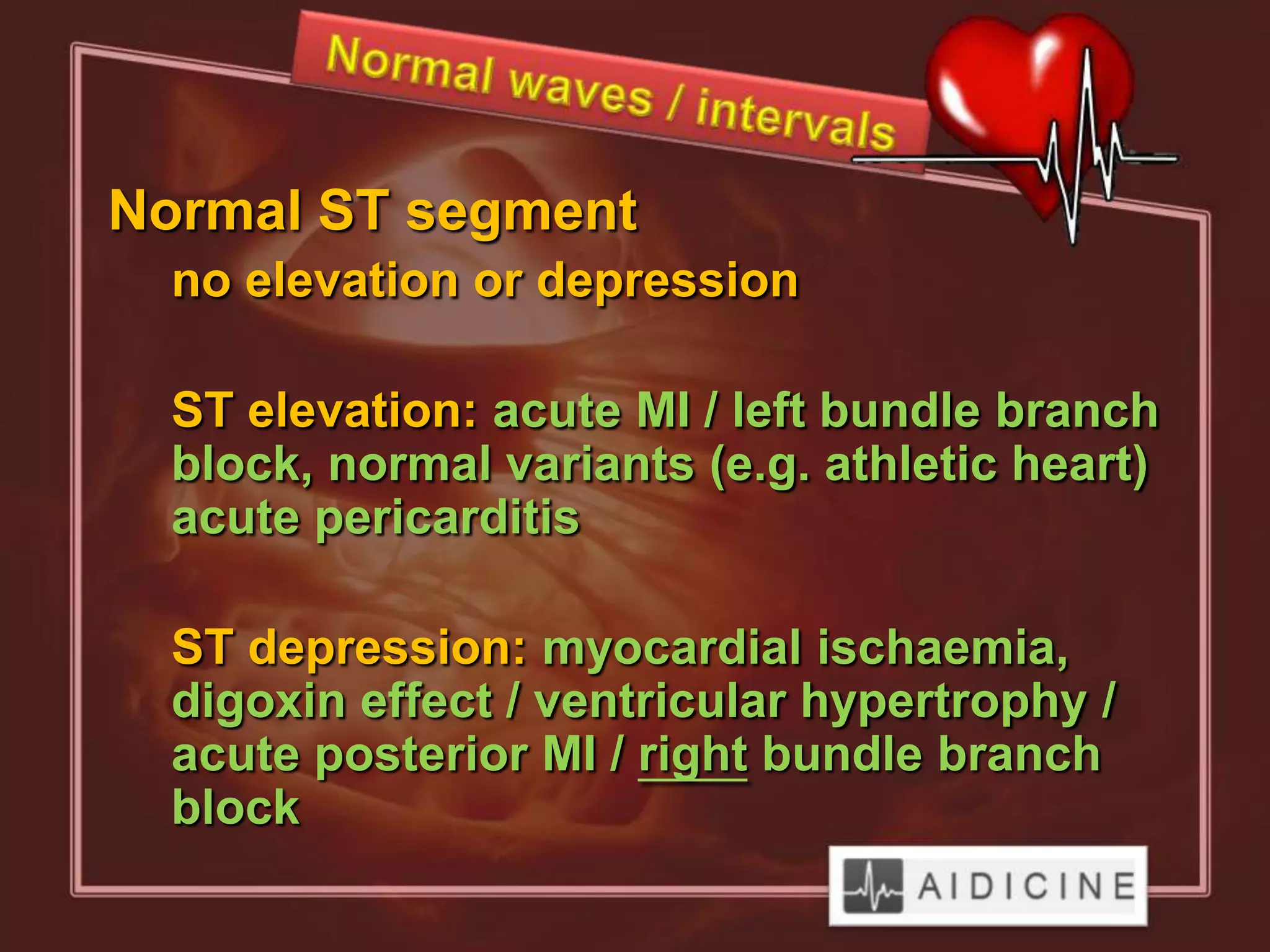
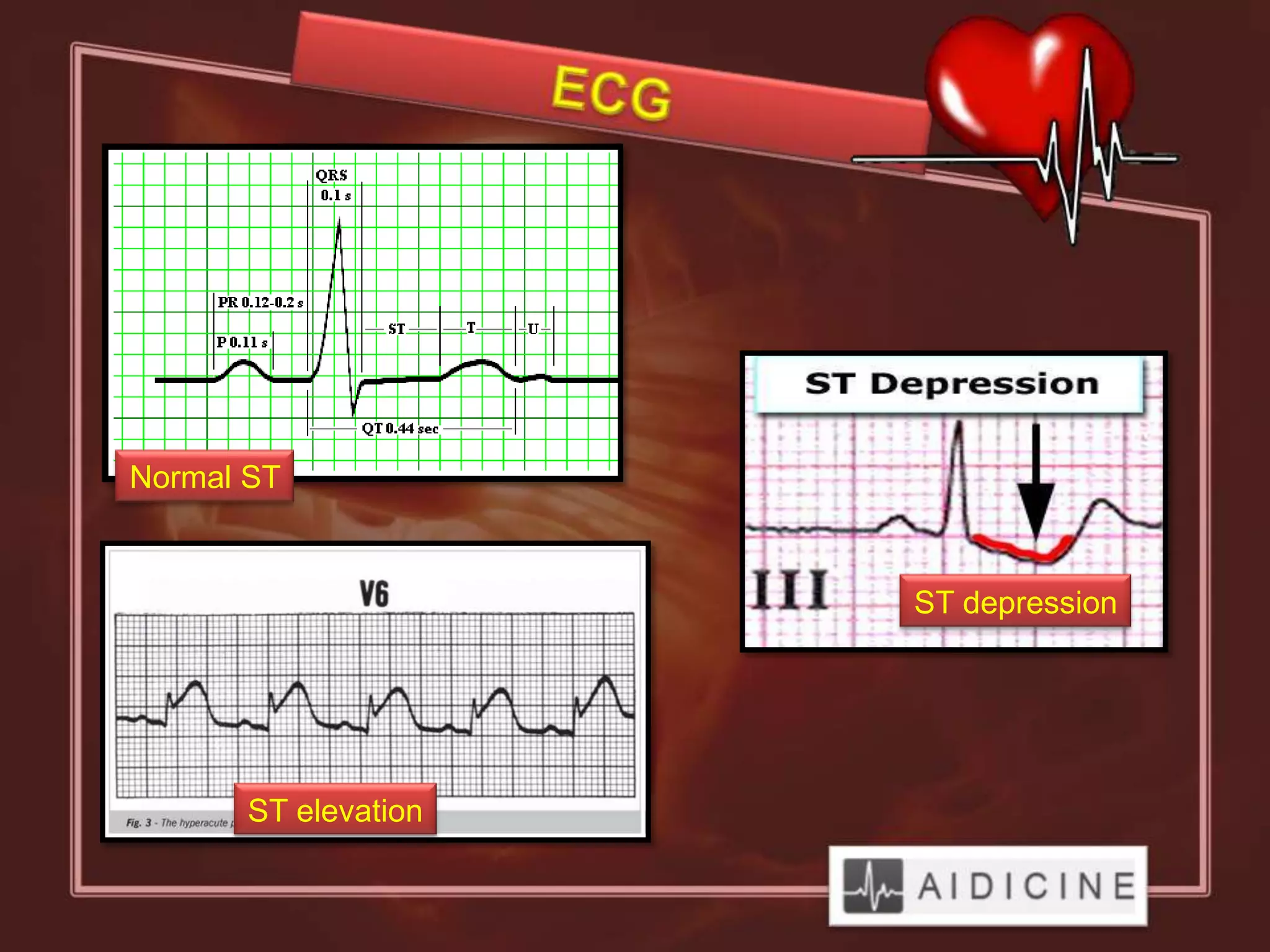
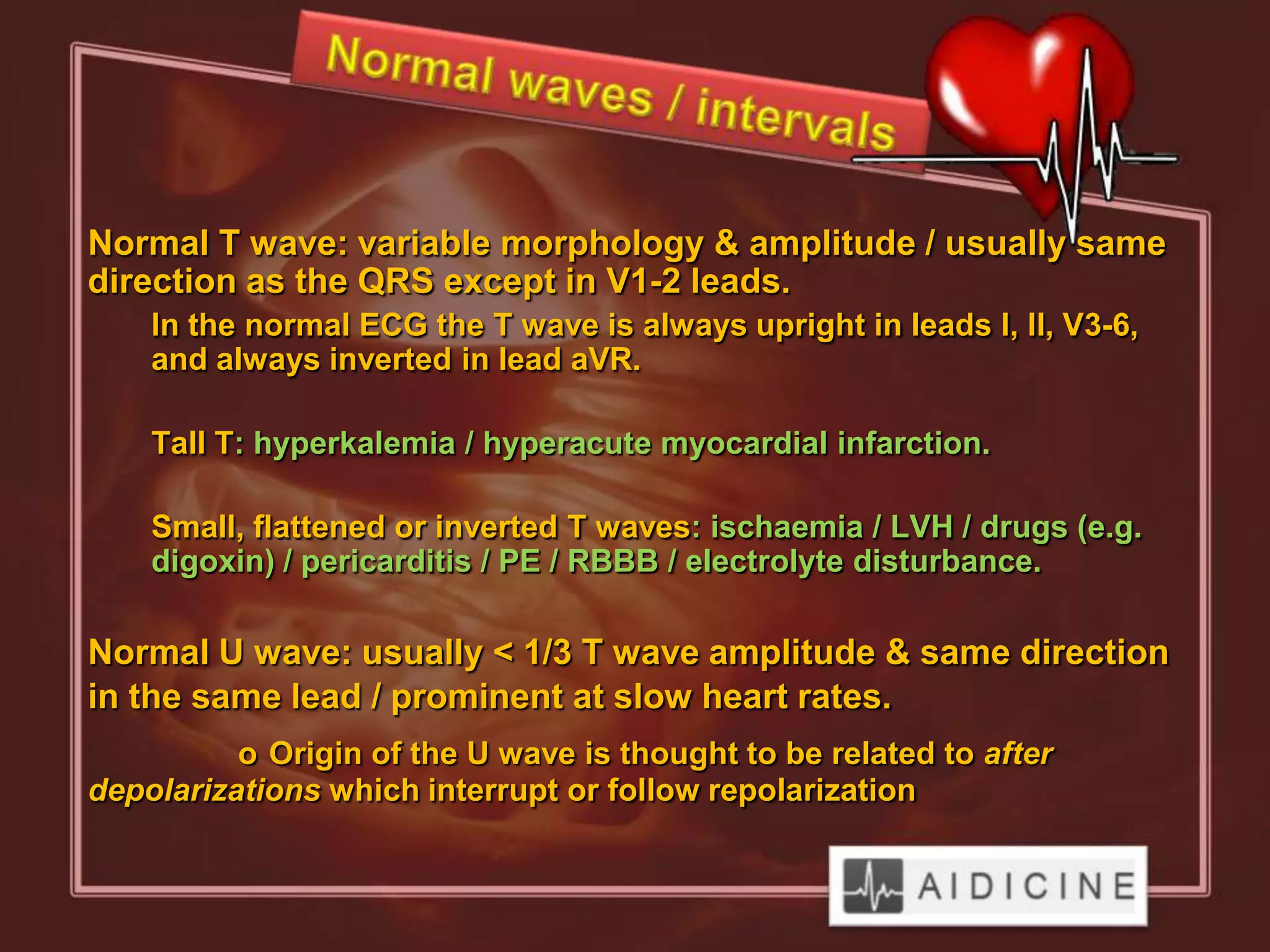
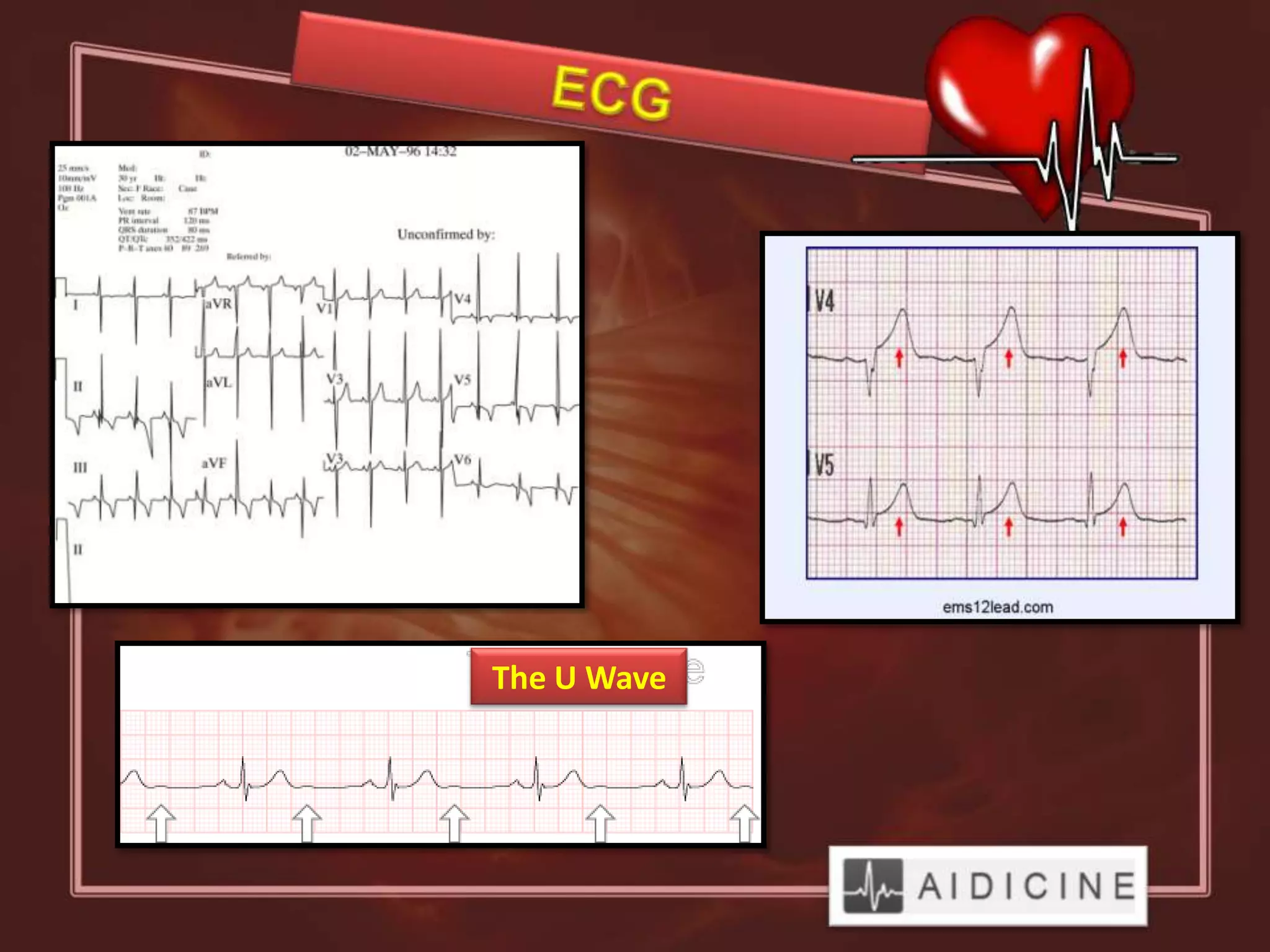
The document provides a detailed overview of electrocardiogram (ECG) fundamentals, including waveforms, leads, and heart rhythm determination. It discusses the significance of different ECG components like the P wave, QRS complex, and T wave while also addressing potential pathologies and their implications. Key methods for interpreting heart rate and QRS axis deviations are outlined, along with conditions associated with abnormal wave patterns.