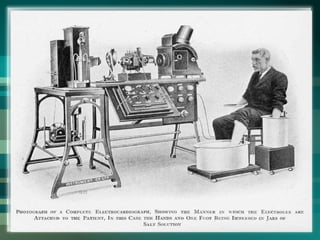
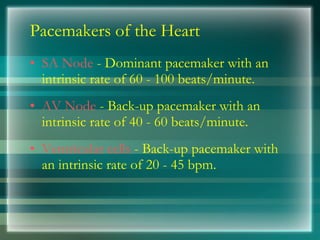
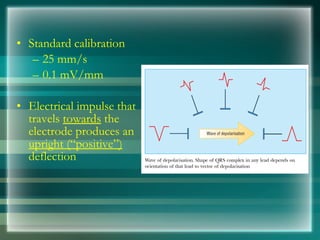
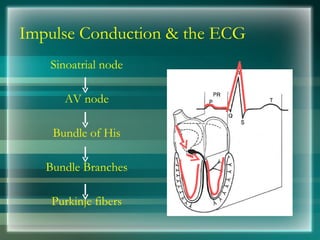
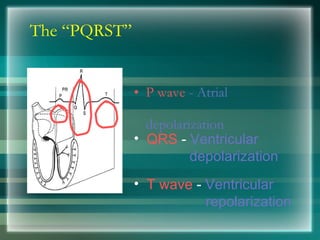
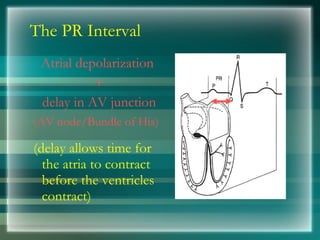
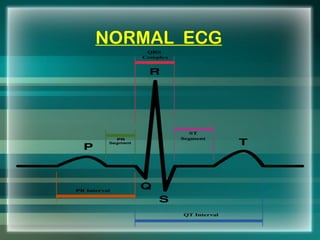
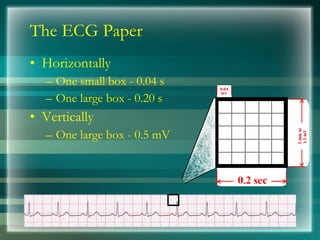
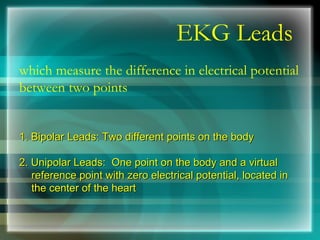
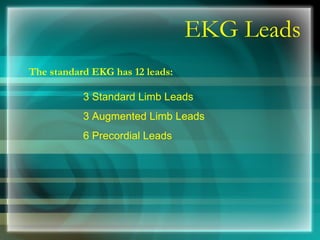
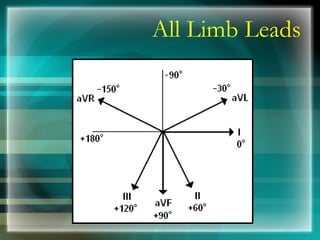
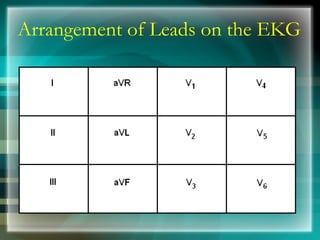
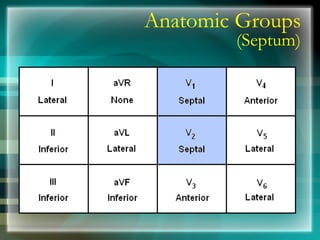
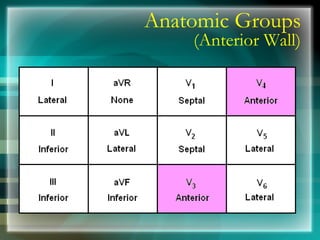
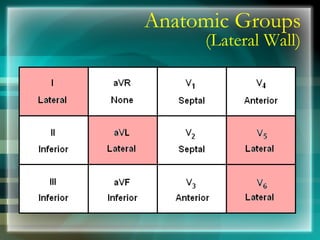
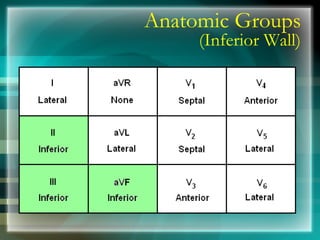
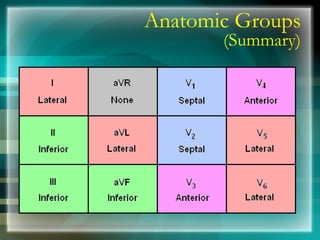
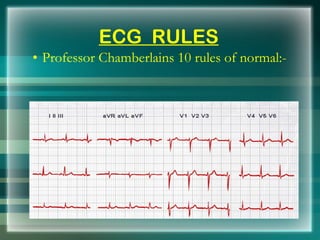
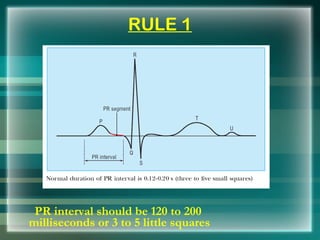
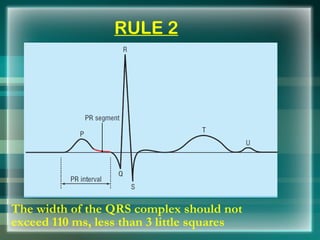
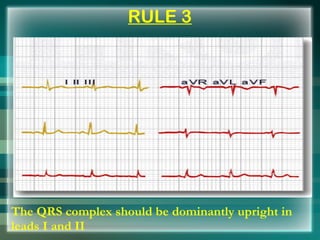
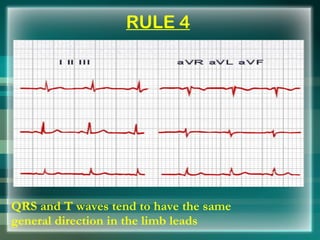
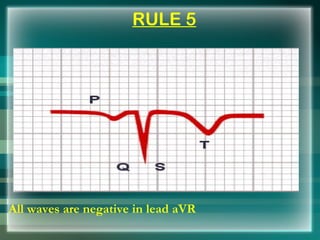
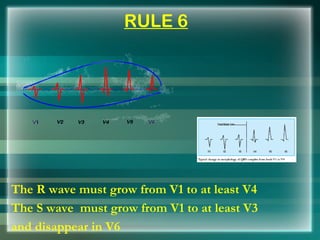
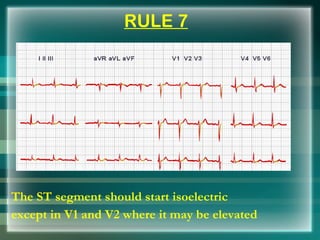
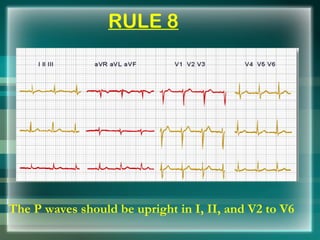
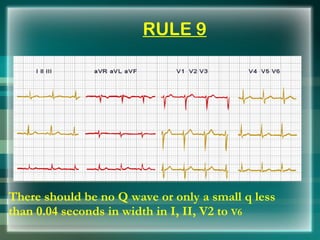
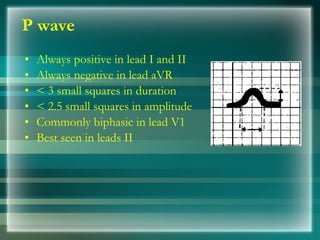
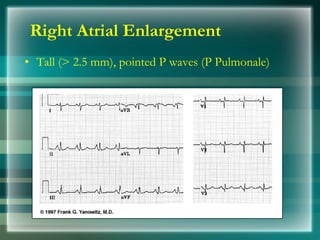
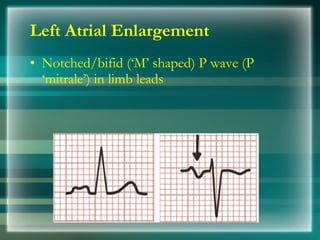
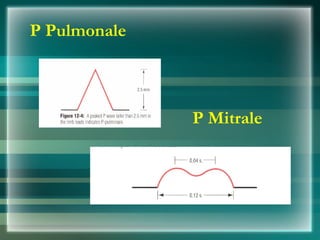
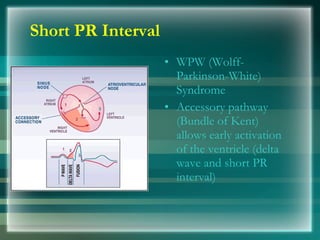
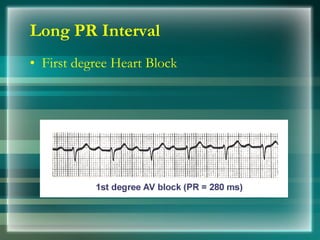
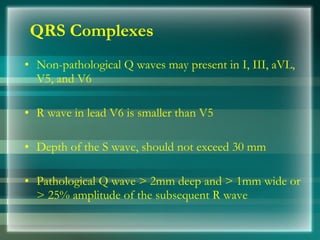
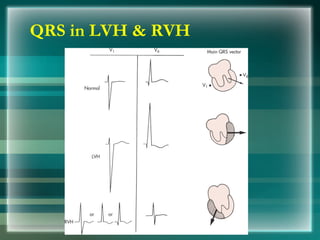
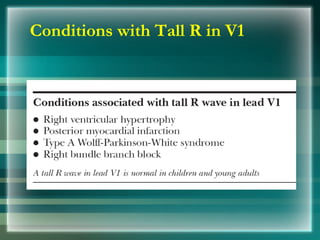
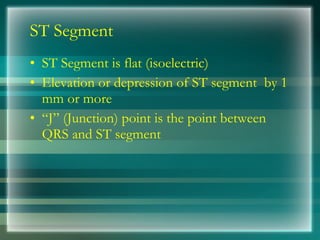
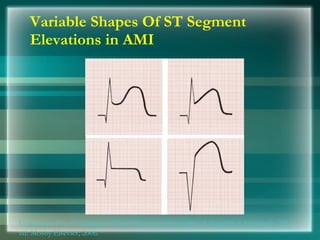
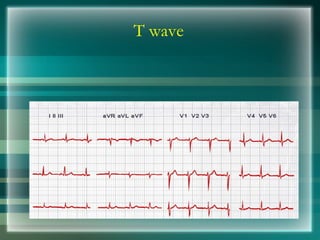
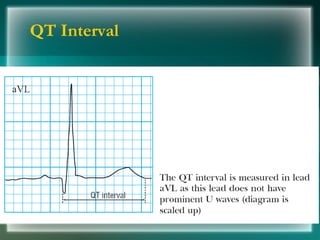
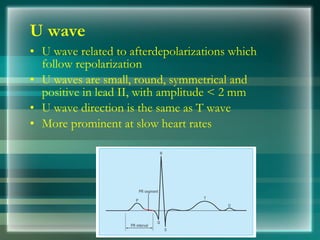
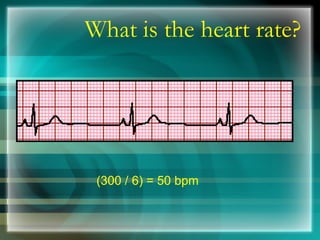
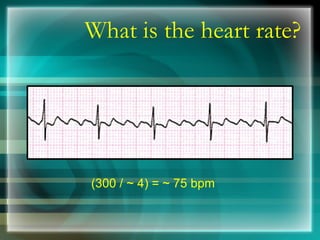
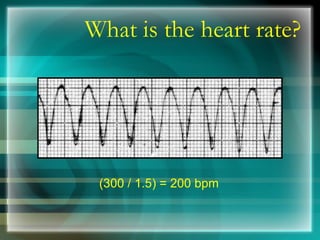
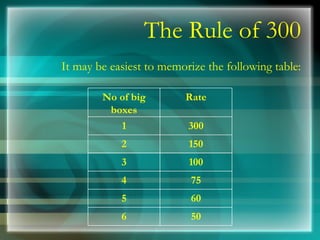
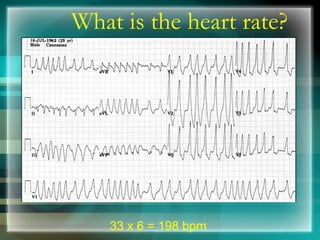
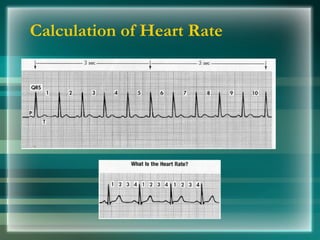
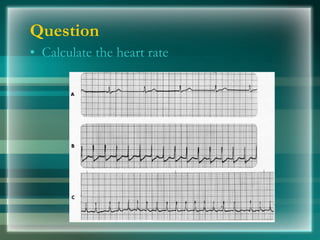
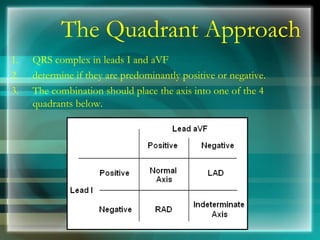
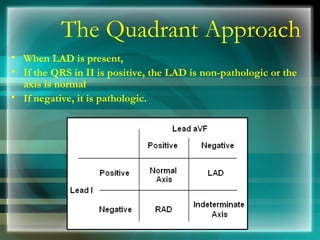
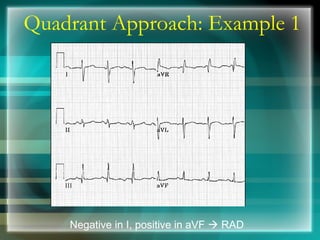
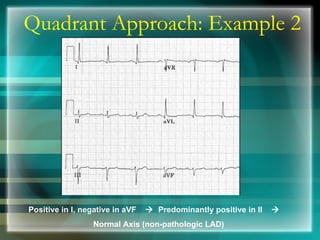
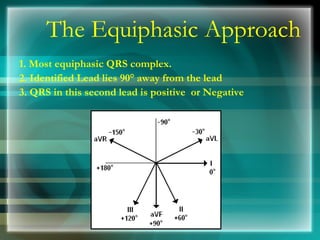
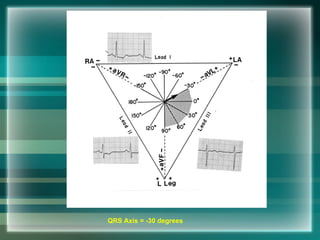
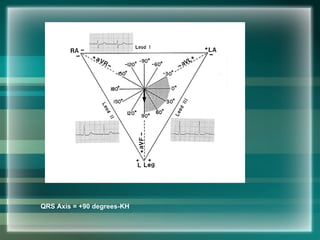
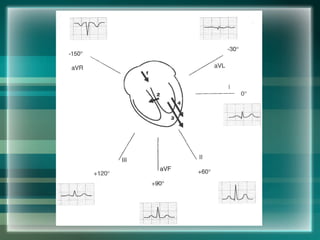
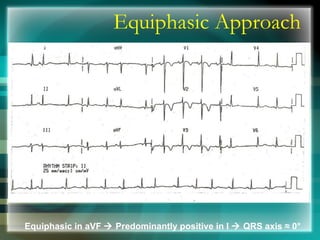
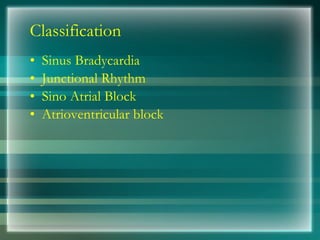
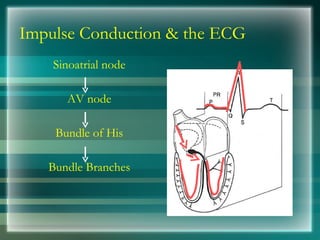
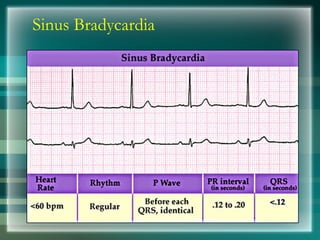
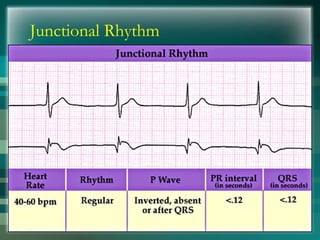
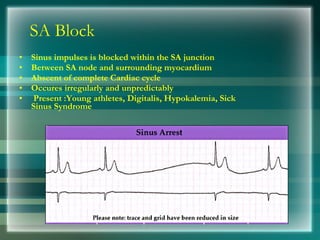
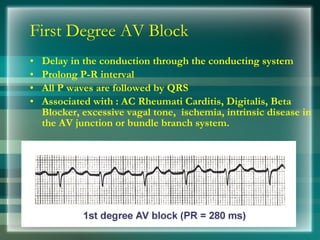
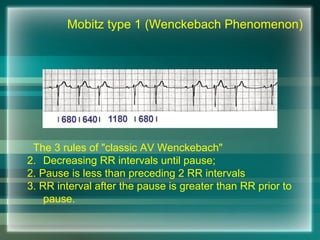
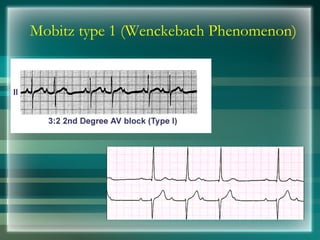
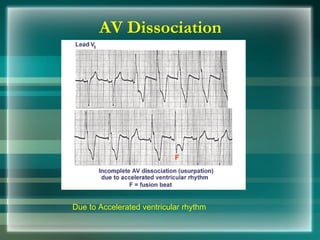
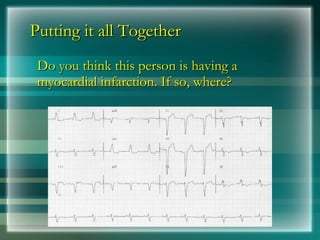
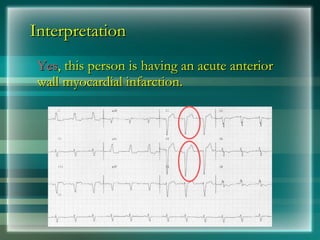
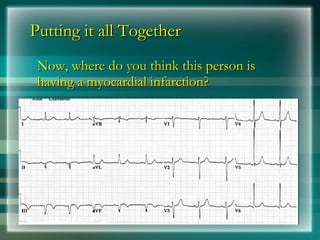
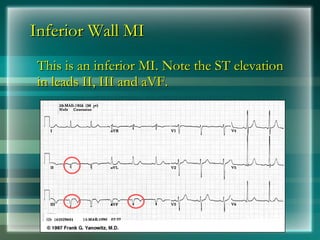
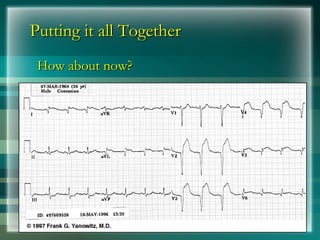
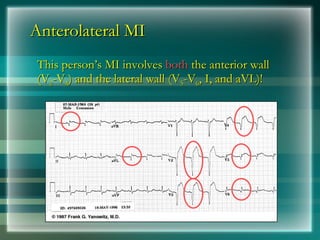
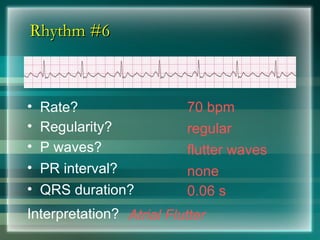
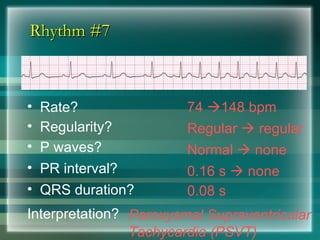
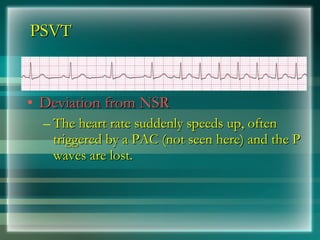
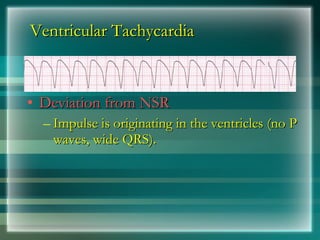
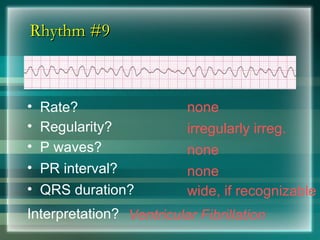
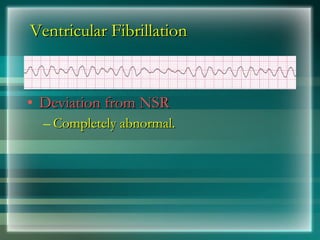
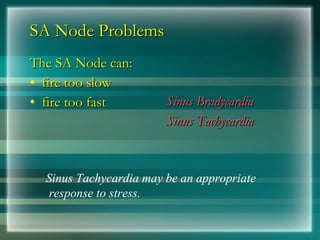
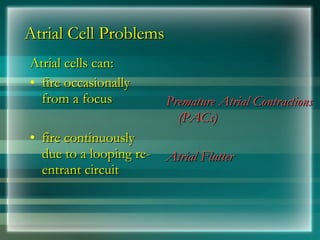
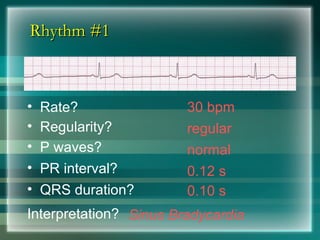
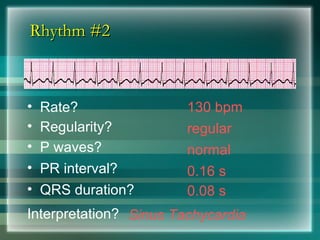
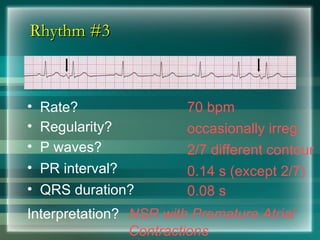
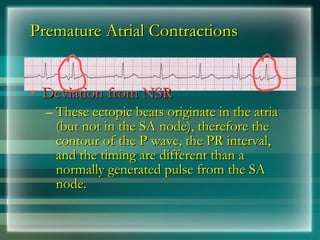
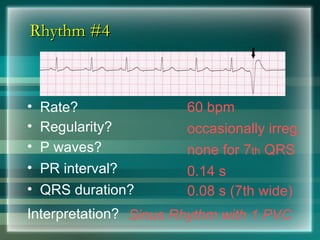
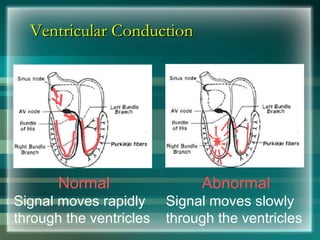
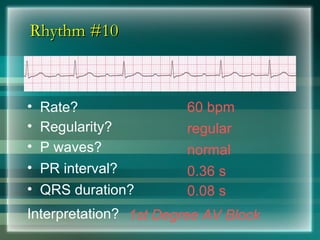
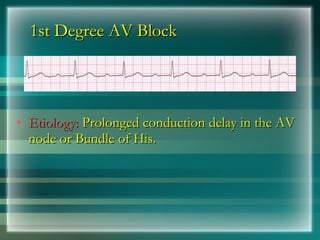
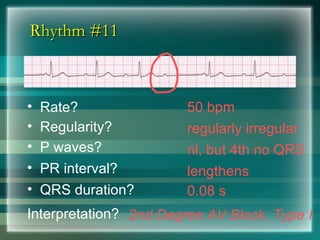
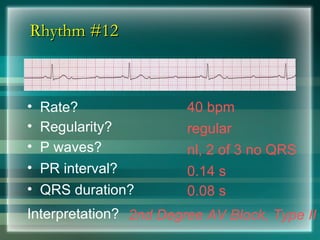
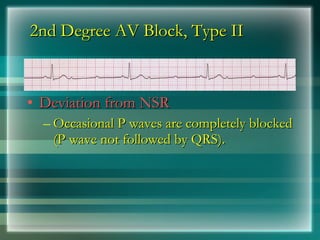
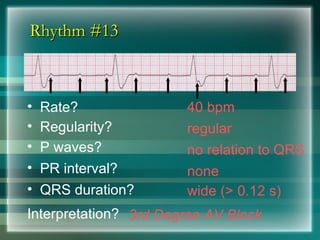
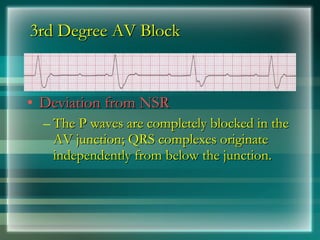
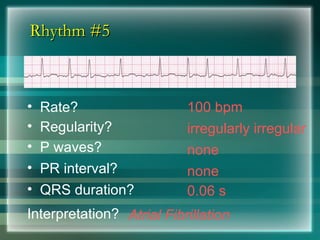
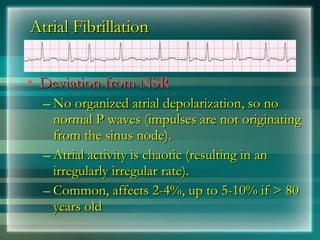
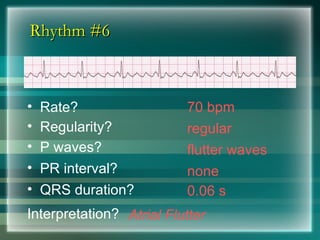
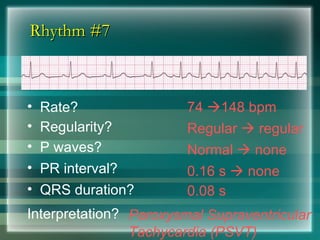
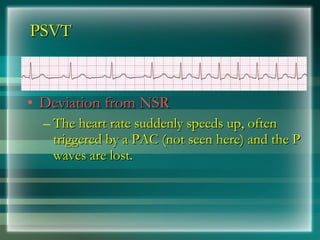
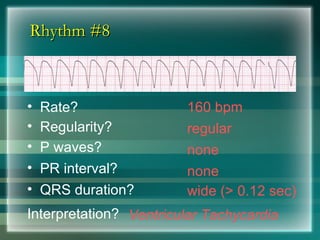
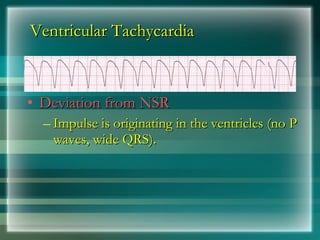
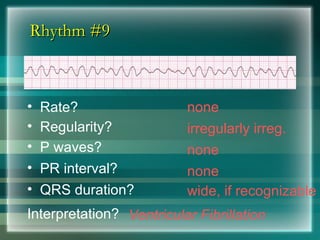
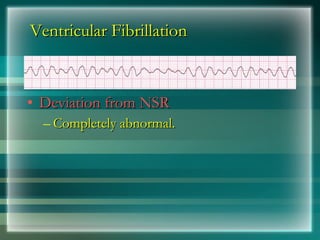
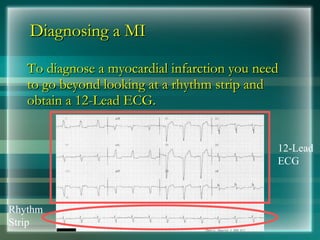
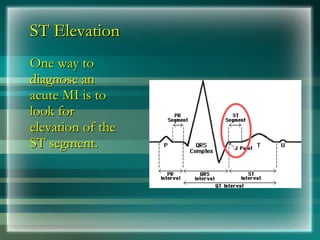
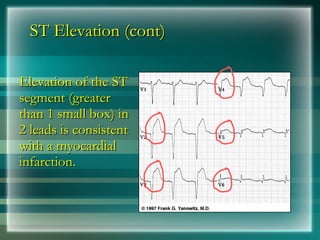
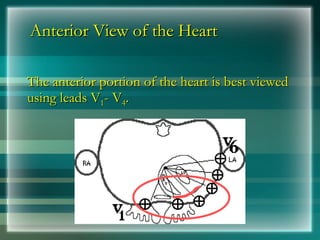
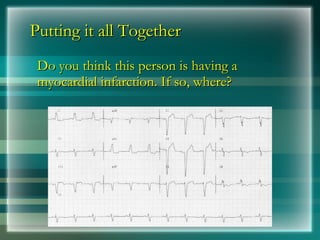
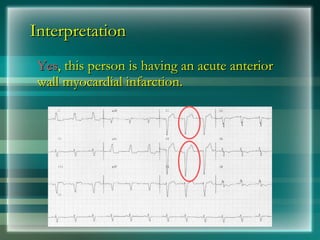
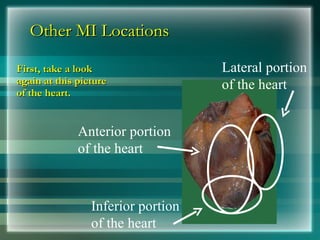
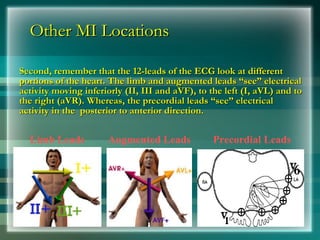
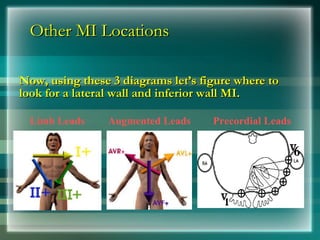
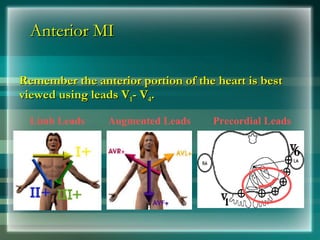
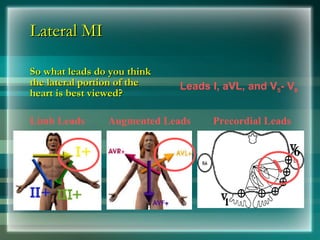
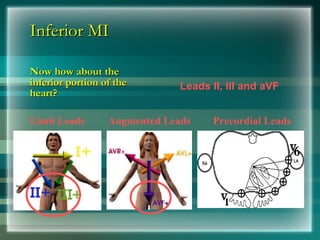
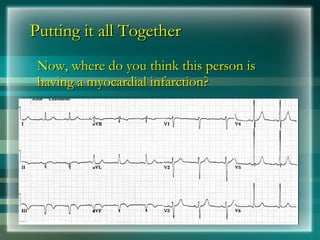
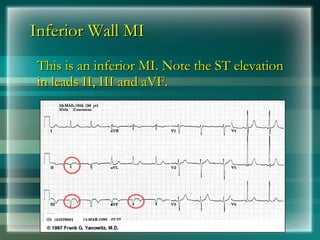
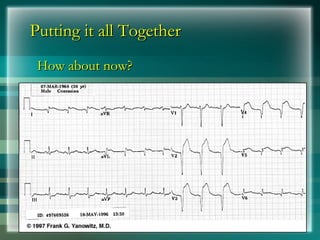
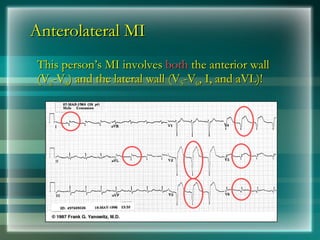
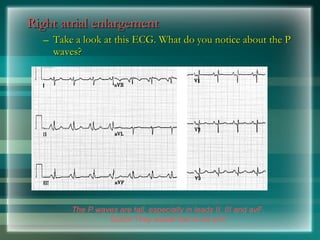
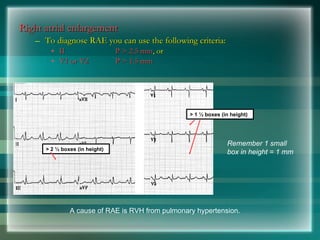
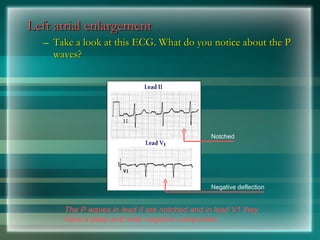
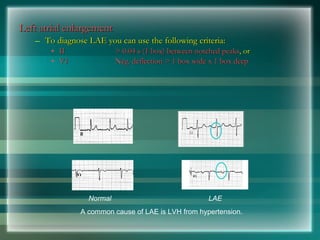
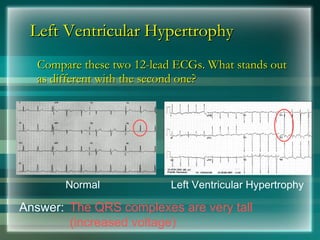
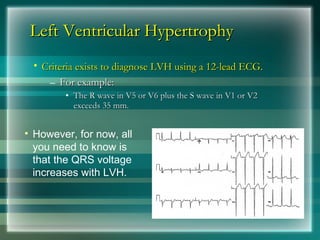
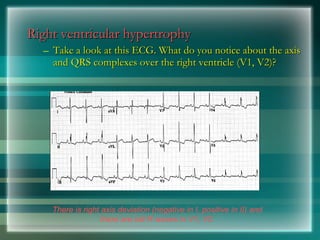
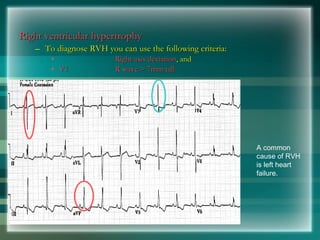
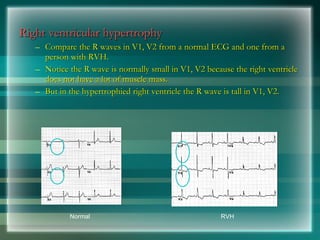
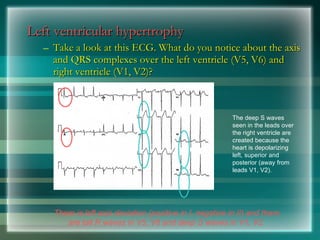
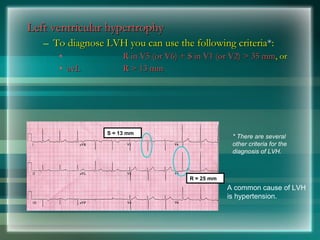
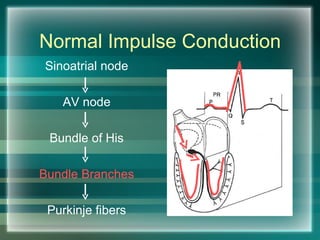
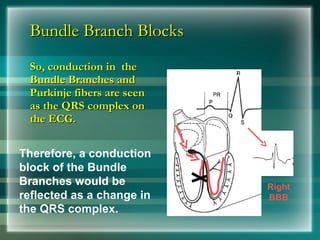
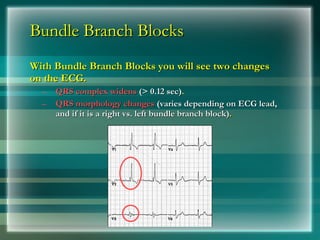
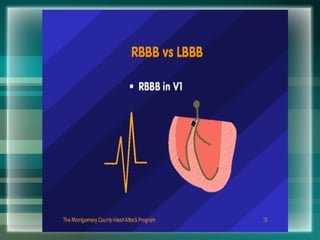
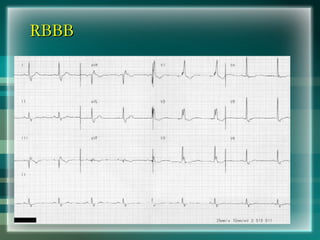
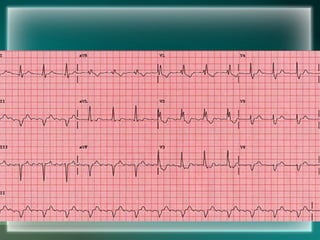
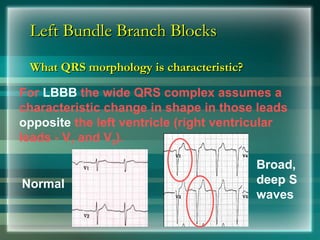
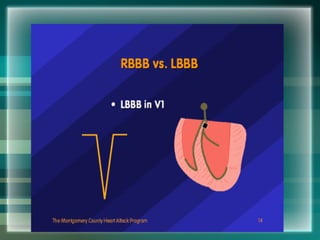
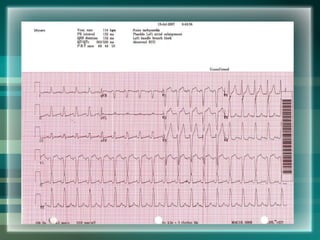
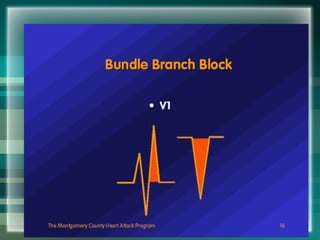
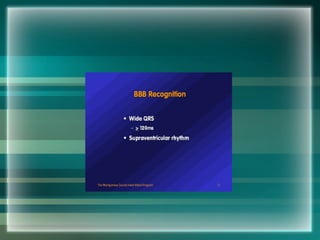
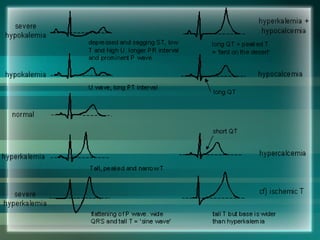
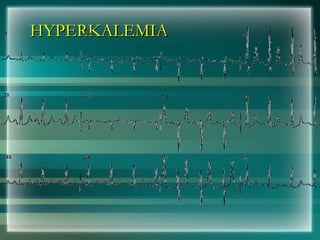
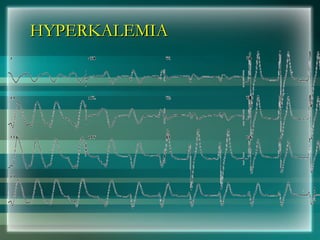
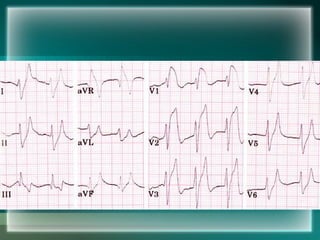
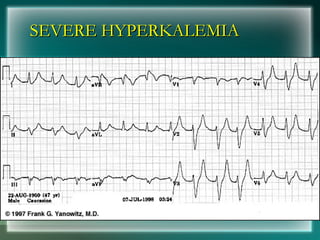
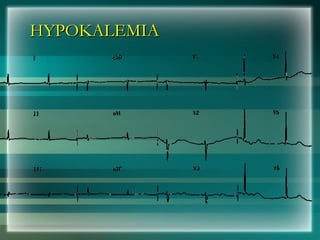
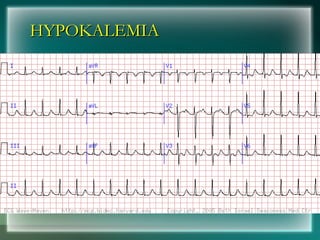
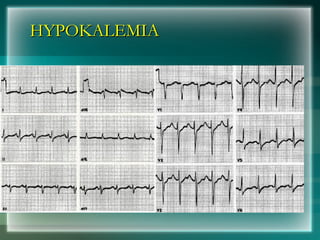
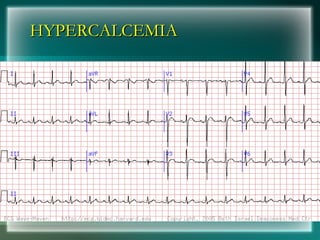
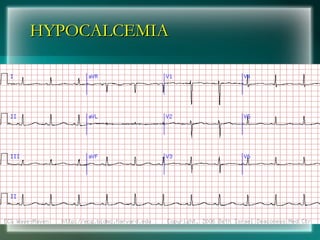
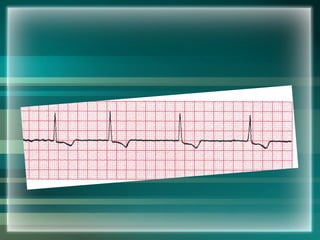
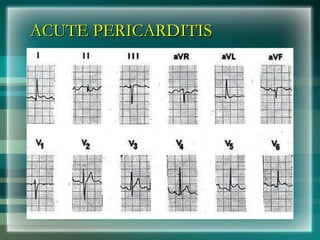
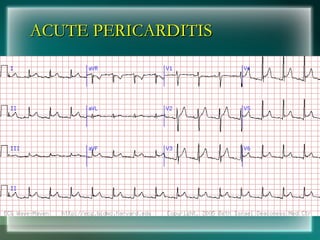
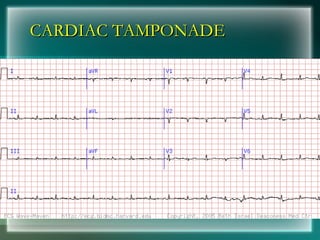
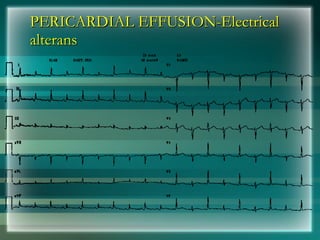
The document provides an overview of basics of electrocardiography (ECG/EKG), including a brief history, the components of a normal ECG, and how to interpret common abnormalities. It discusses the waves that make up the ECG, such as the P, QRS, and T waves, and how to determine heart rate. The document also covers arrhythmias like atrial flutter, supraventricular tachycardia, ventricular tachycardia, and myocardial infarction locations based on ECG findings.