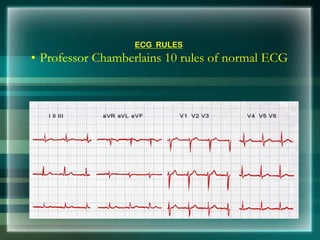
This document provides an overview of electrocardiography (ECG/EKG) including its history, components, and how to interpret common rhythms. Some key points:
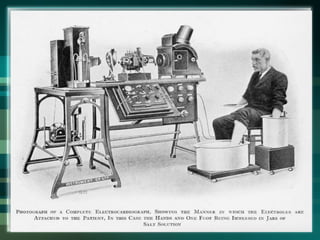
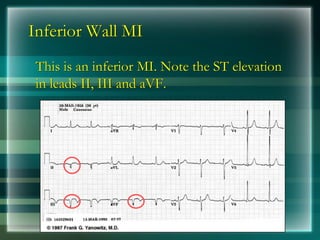
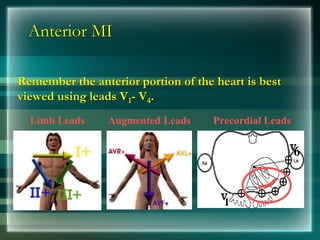
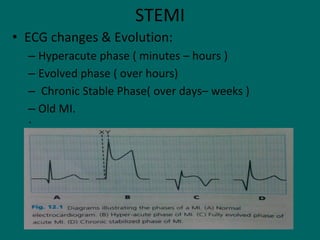
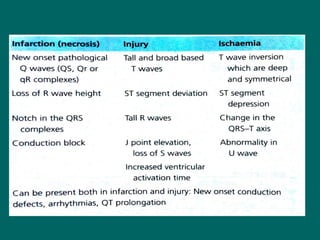
- ECG records electrical activity of the heart and was invented in the late 19th century. It helps diagnose arrhythmias, ischemia, infarction and other cardiac conditions.
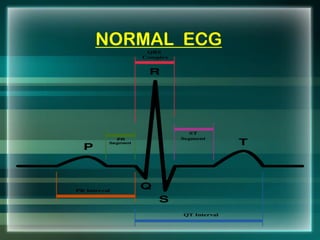
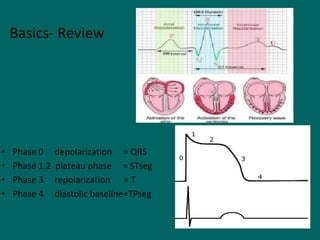
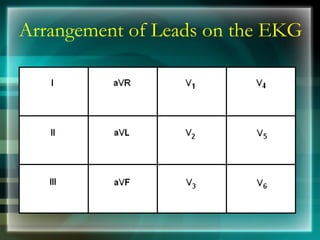
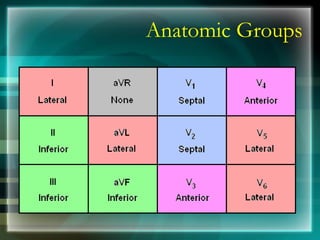
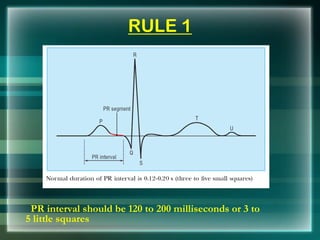
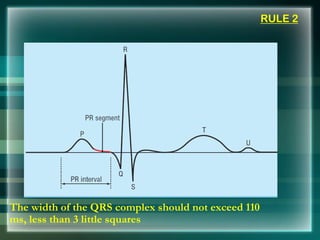
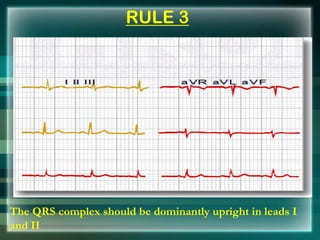
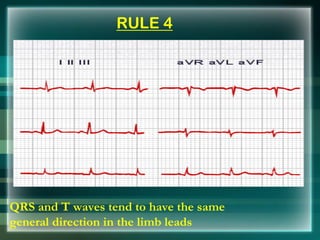
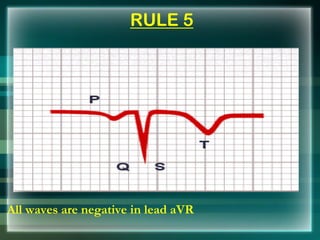
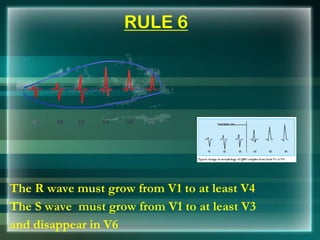
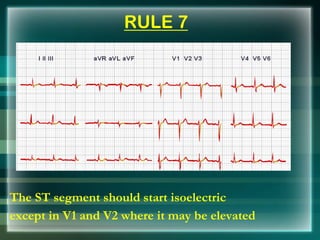
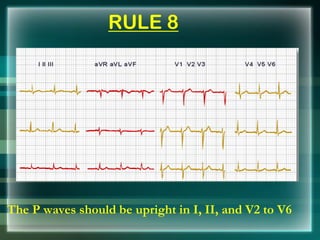
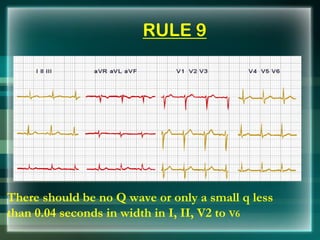
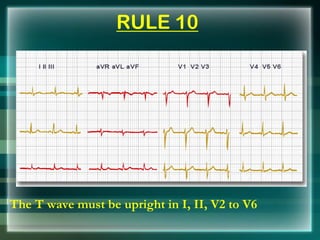
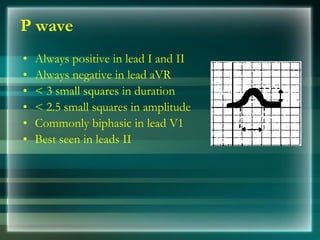
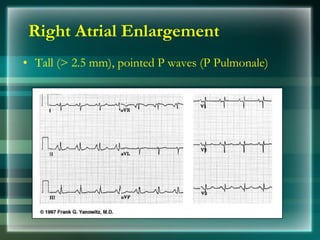
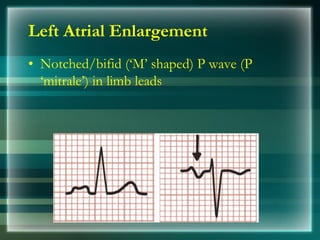
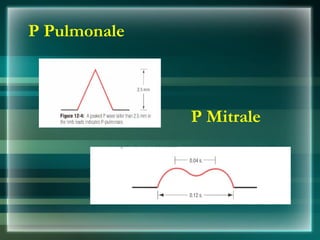
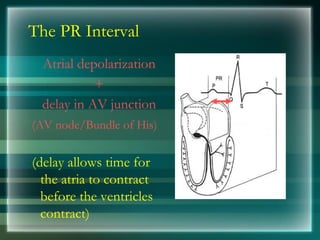
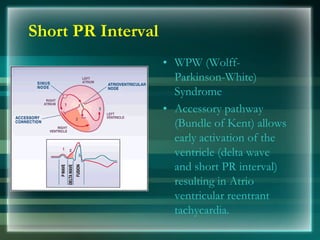
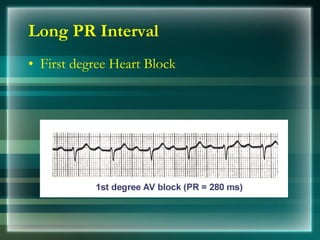
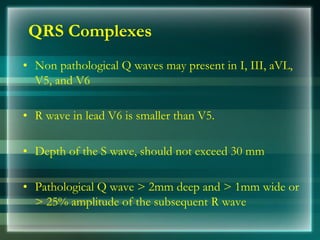
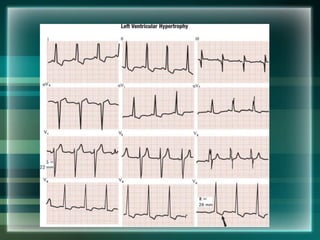
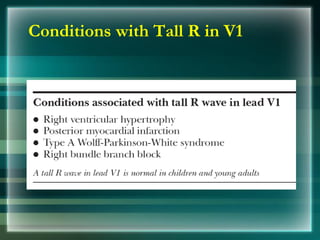
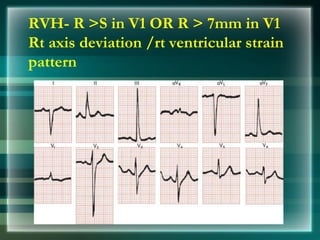
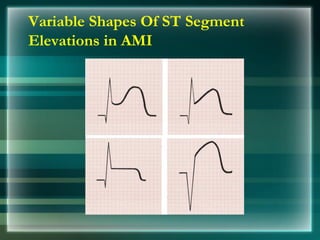
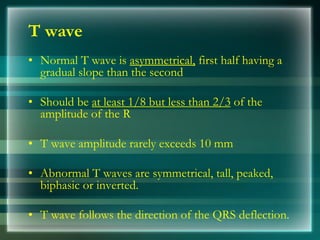
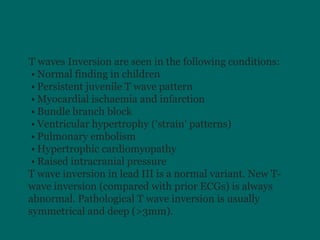
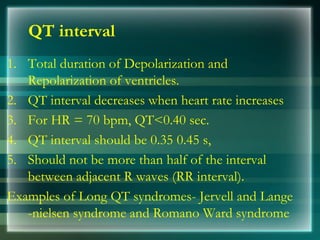
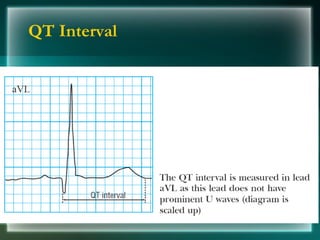
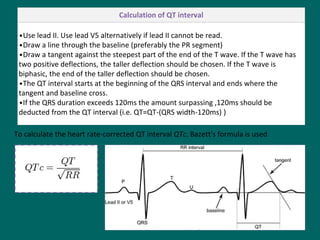
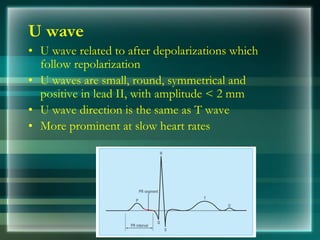
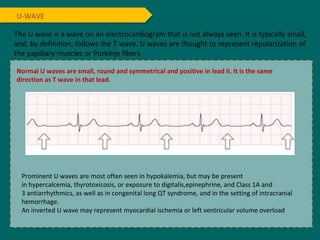
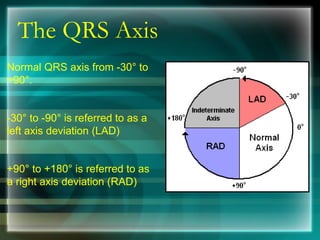
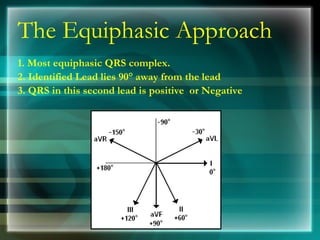
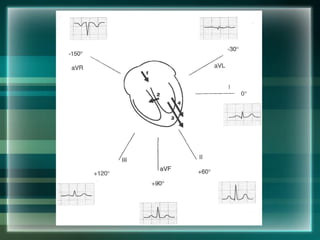
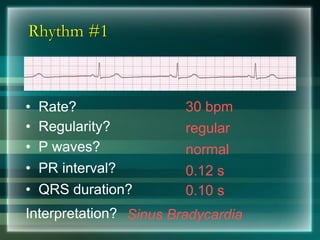
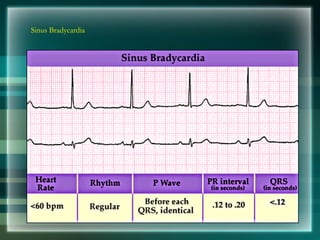
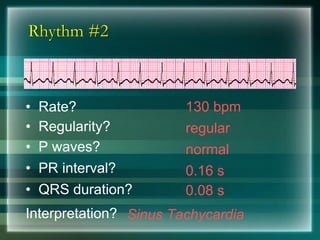
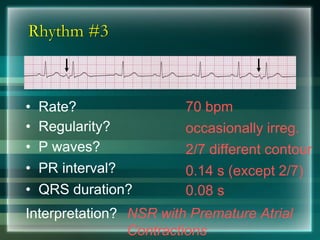
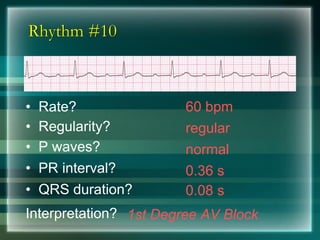
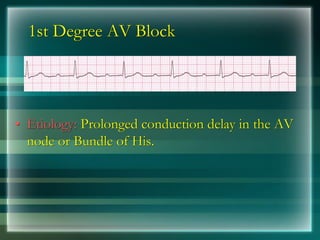
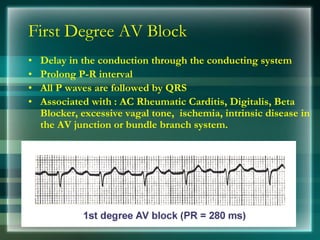
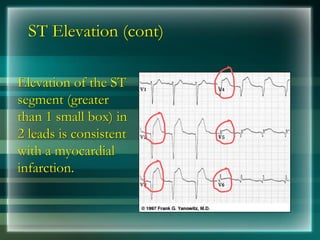
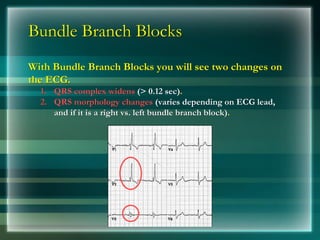
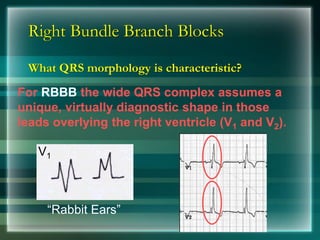
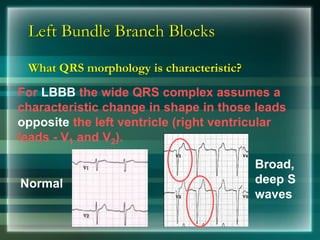
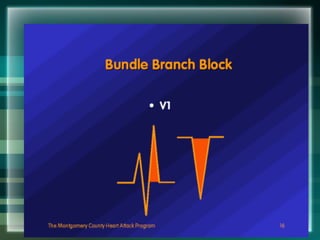
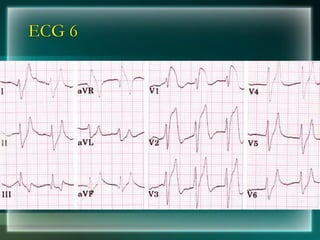
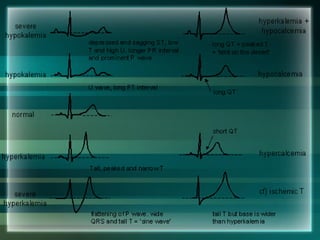
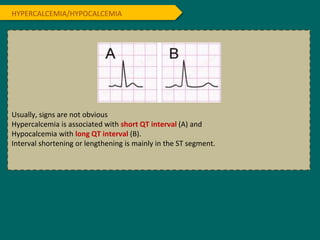
- The ECG tracing has components (P wave, PR interval, QRS complex, ST segment, T wave) that reflect different stages of the cardiac cycle.
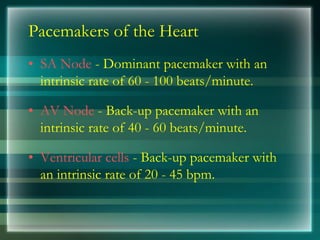
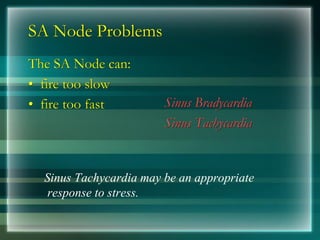
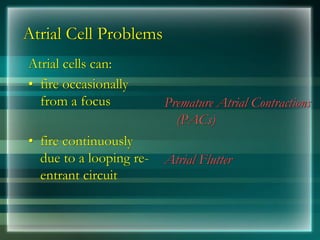
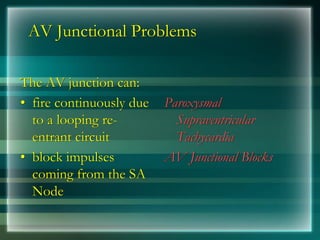
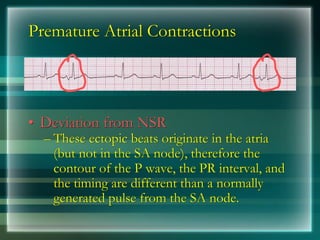
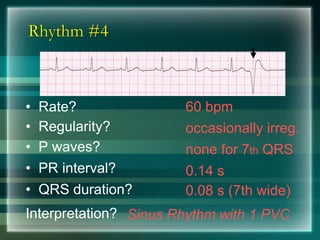
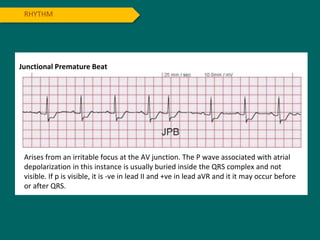
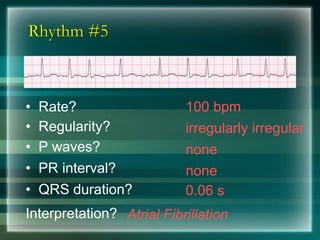
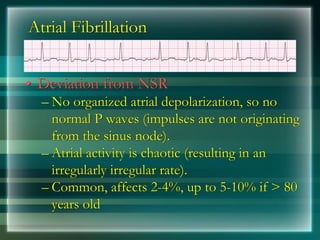
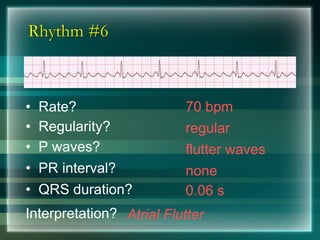
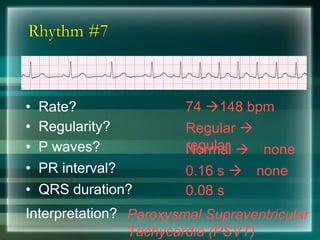
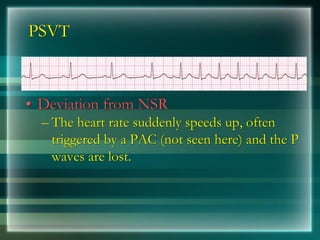
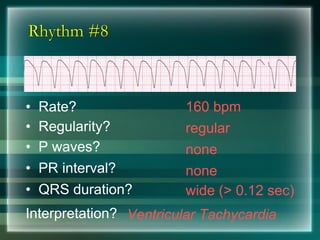
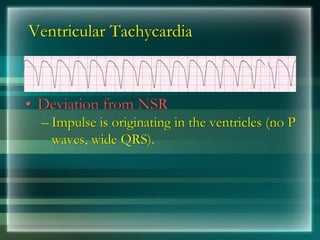
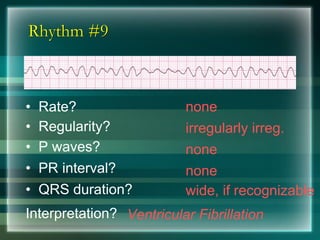
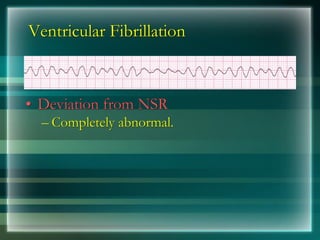
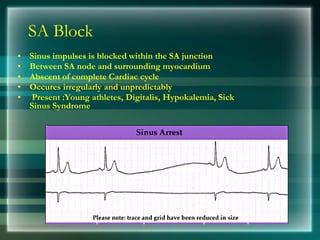
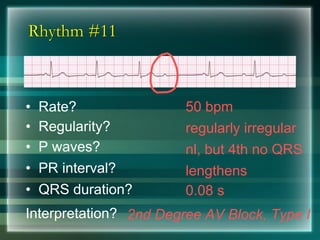
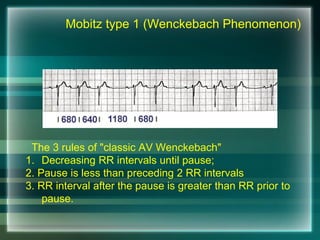
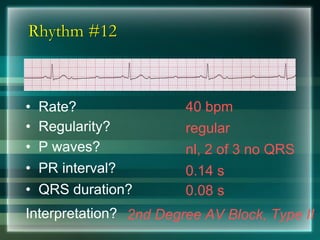
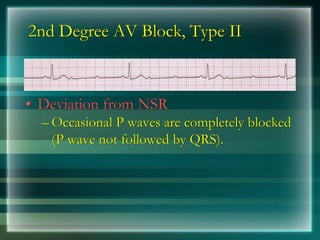
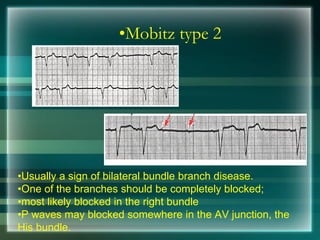
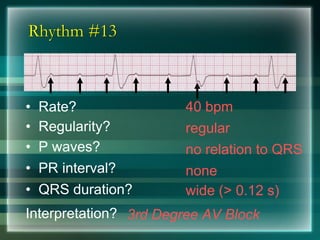
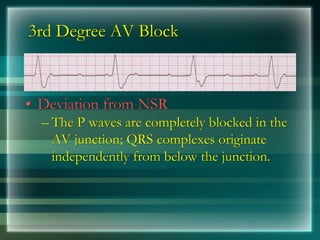
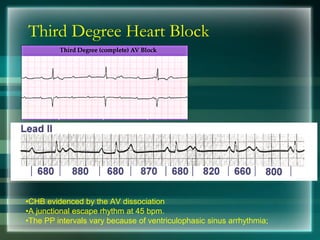
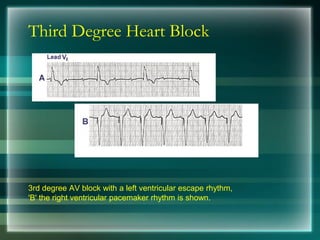
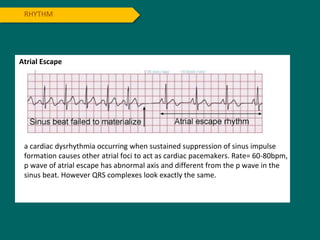
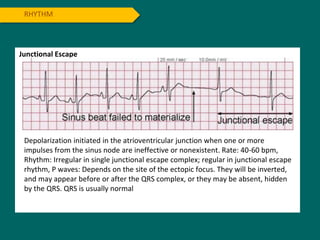
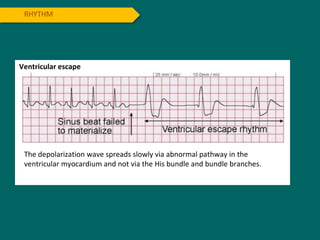
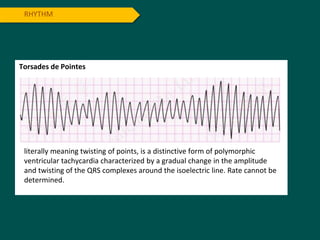
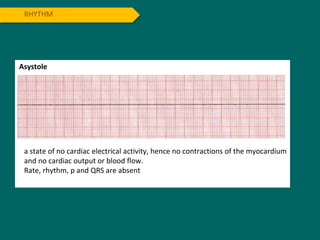
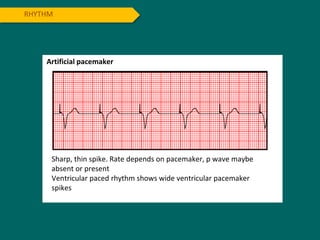
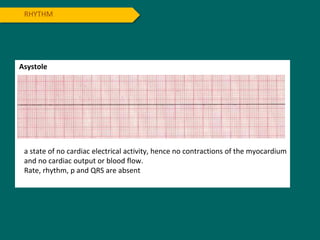
- Common arrhythmias arise from problems in the sinus node, atria, AV node or ventricles. These include sinus bradycardia, sinus tachycardia, premature