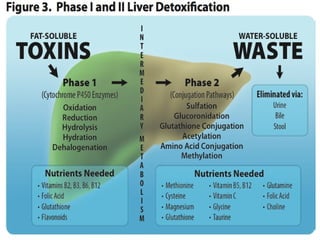
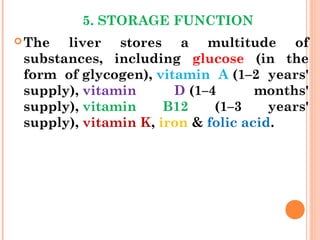
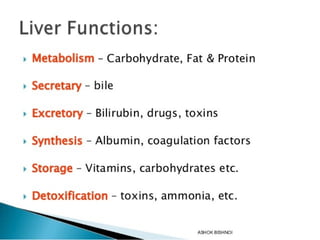
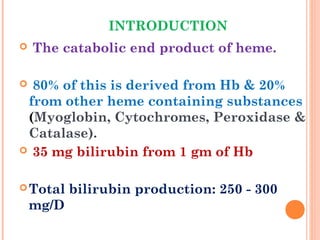
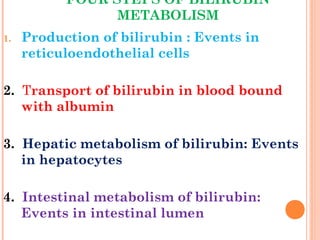
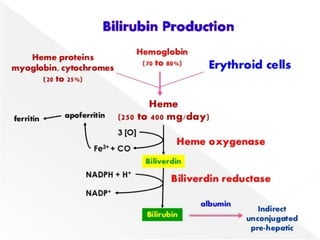
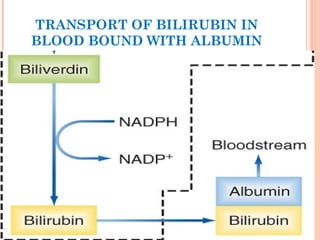
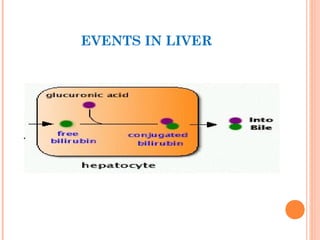
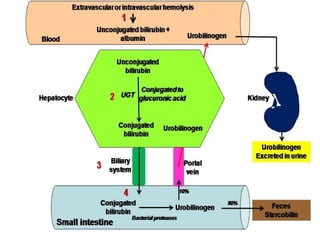
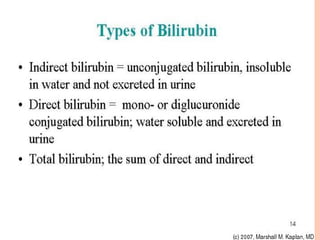
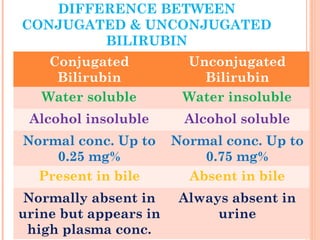
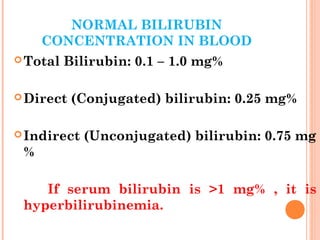
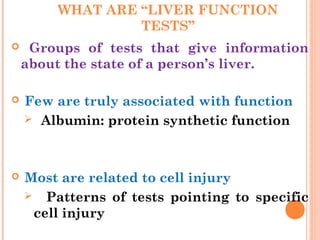
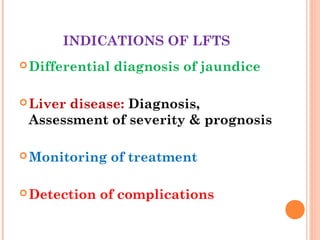
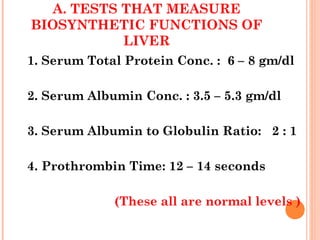
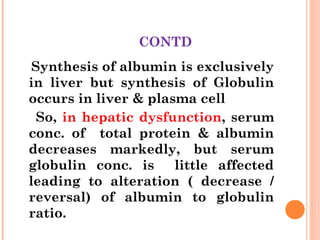
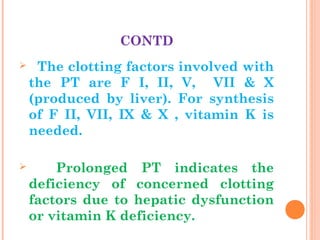
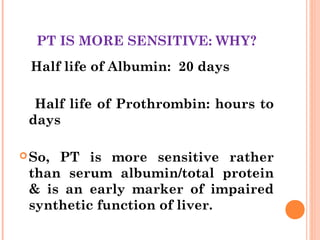
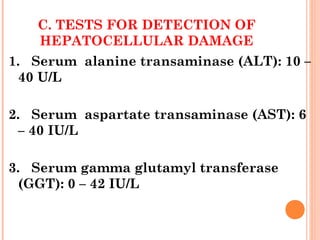
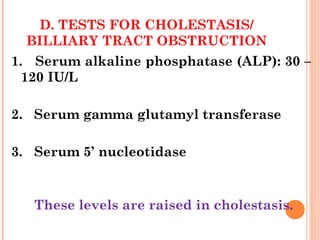
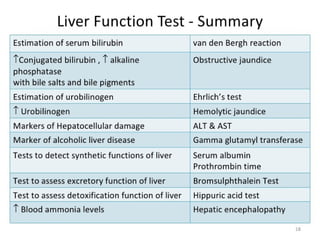
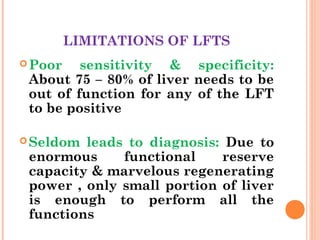
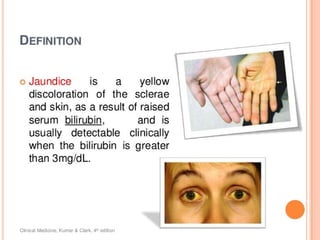
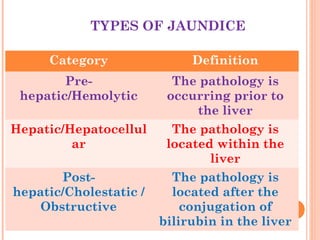
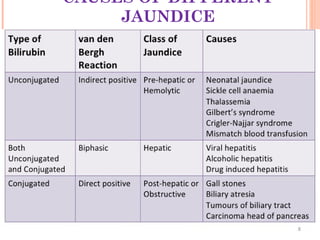
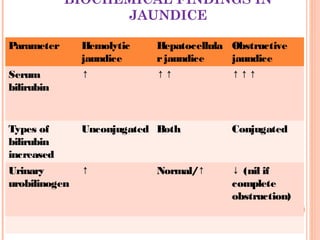
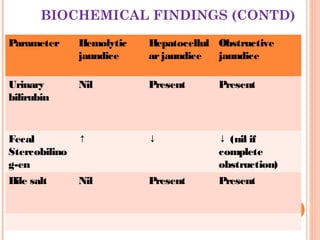
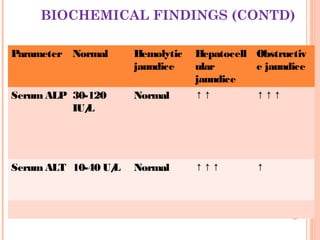
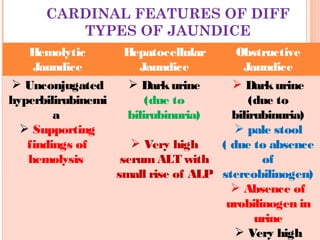
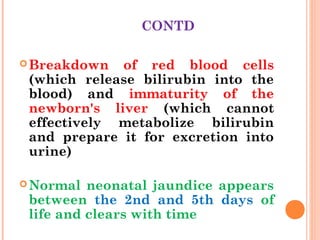
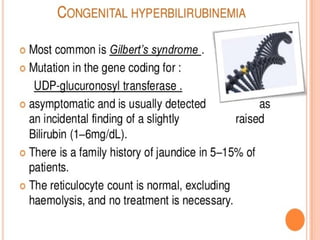
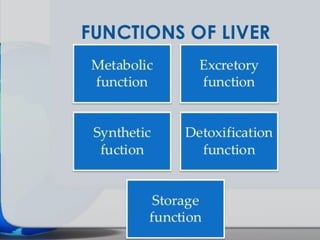
This document provides an overview of commonly performed liver function tests and jaundice. It discusses the structure and functions of the liver, including metabolic, excretory, synthetic and detoxification roles. Key liver function tests are described that evaluate biosynthetic (e.g. albumin, PT), excretory (bilirubin), hepatocellular damage (ALT, AST, GGT), and cholestasis/obstruction (ALP) functions. Bilirubin metabolism and the differences between conjugated and unconjugated bilirubin are explained. The document also covers the types, causes and distinguishing biochemical findings of pre-hepatic, hepatic and post-hepatic jaund
![CONTD
Two major types of cells:
Parenchymal cells (hepatocytes): 80%
of liver volume.
Non-parenchymal cells: constitute
40% of total number of liver cells but
only 6.5% of its volume.
[Sinusoidal hepatic endothelial cells,
kupffer cells & hepatic stellate cells are
some of the non-parenchymal cells]](https://image.slidesharecdn.com/commonlydoneliverfunctiontestslft-150121000429-conversion-gate02/85/Commonly-done-liver-function-tests-4-320.jpg)
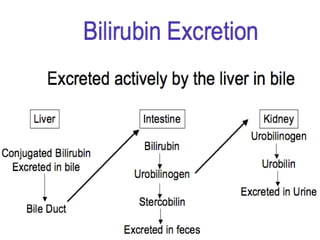
![2. EXCRETORY FUNCTION
Bile pigments, bile salts, drugs,
steroids (cholesterol), heavy metals
etc are excreted in bile into
intestine.
[Secretory function of liver
includes secretion of bile into the
intestine]](https://image.slidesharecdn.com/commonlydoneliverfunctiontestslft-150121000429-conversion-gate02/85/Commonly-done-liver-function-tests-10-320.jpg)