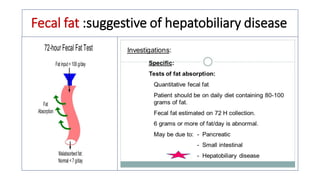
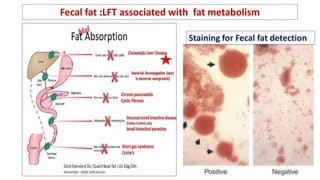
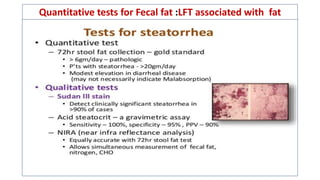
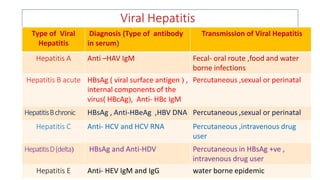
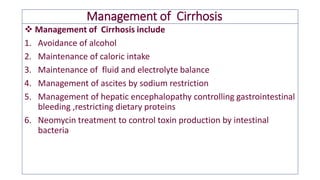
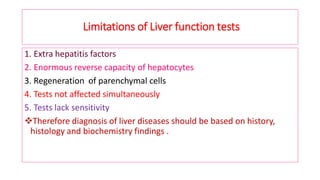
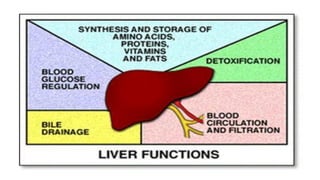
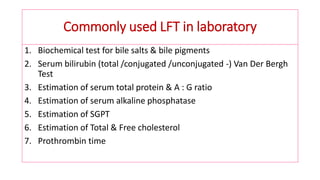
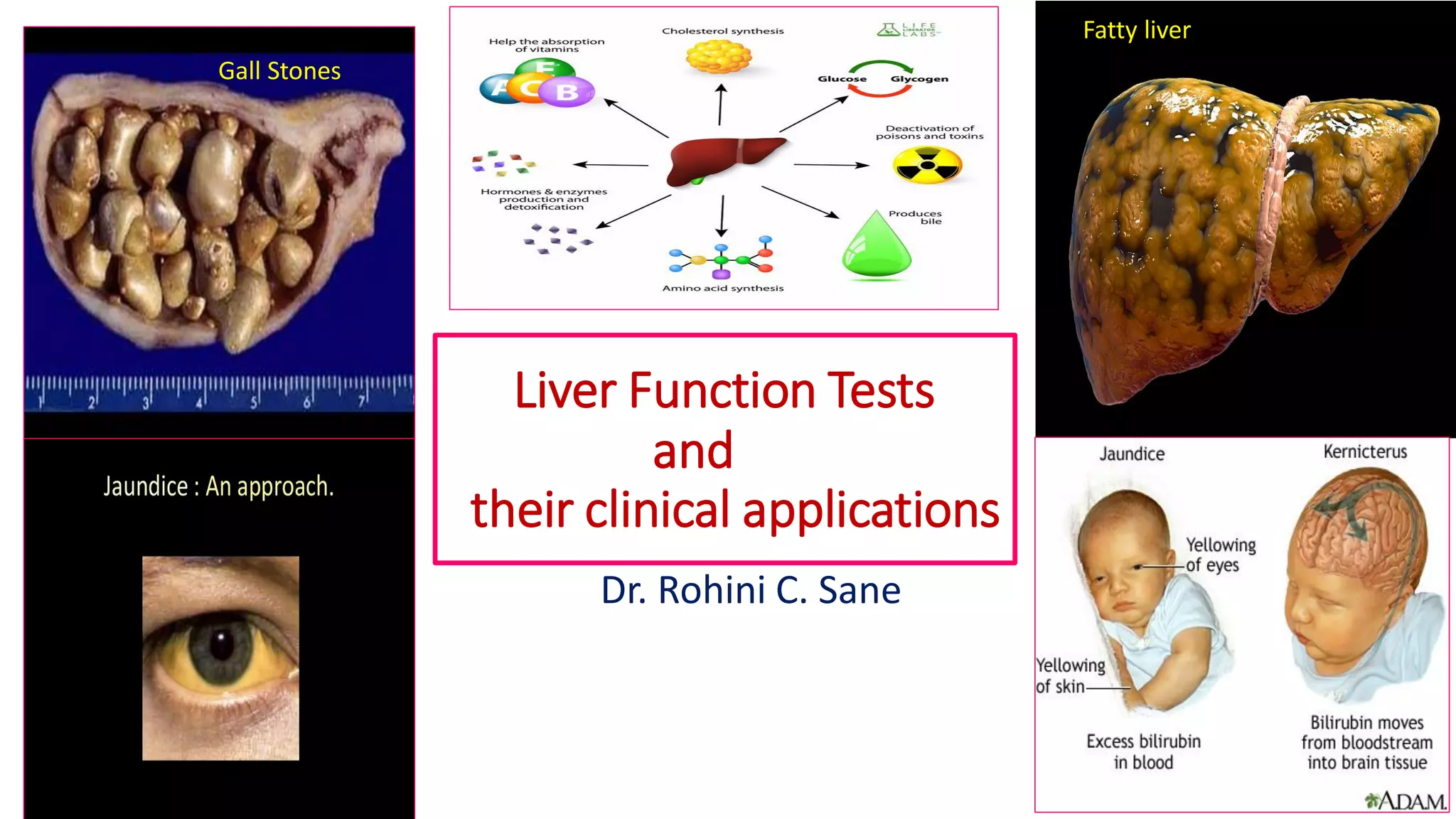
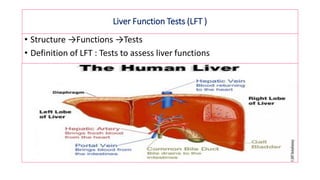
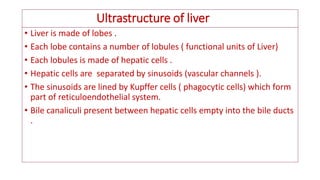
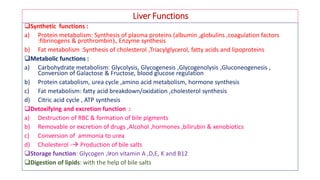
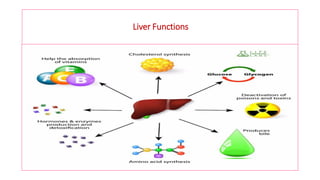
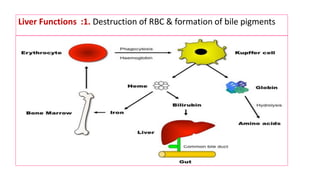
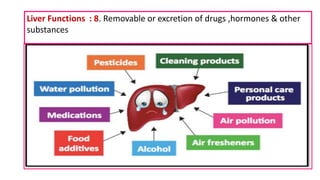
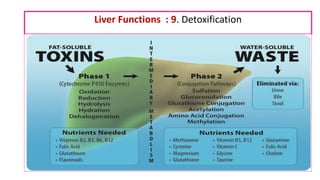
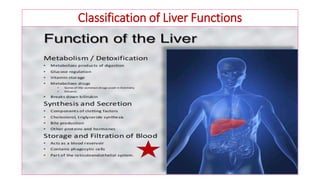
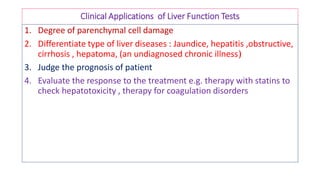
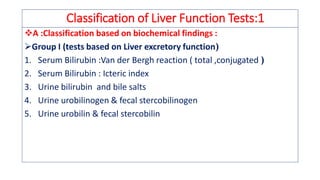
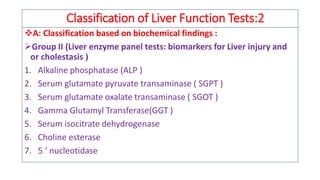
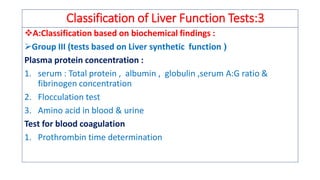
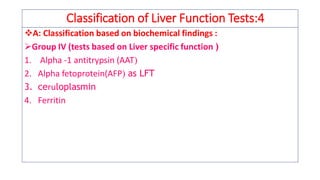
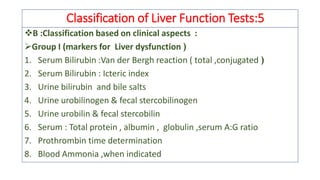
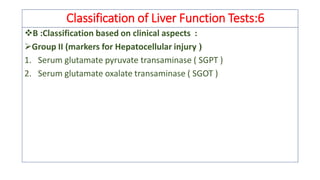
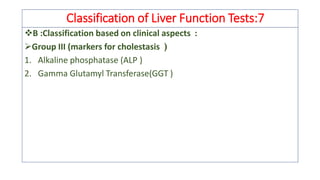
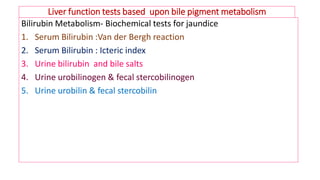
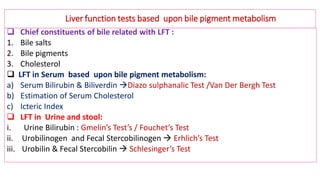
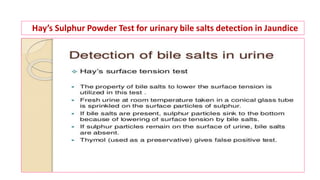
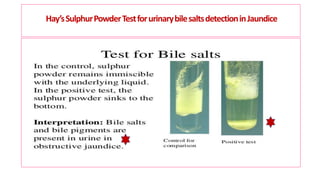
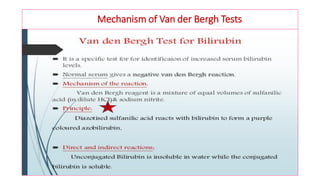
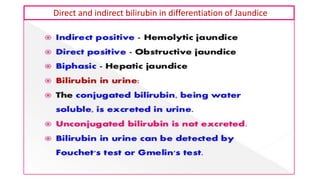
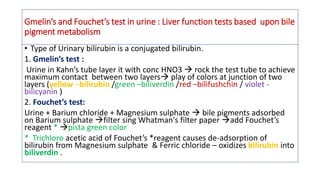
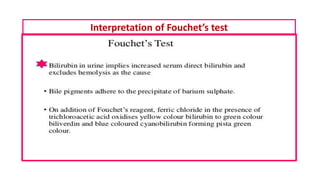
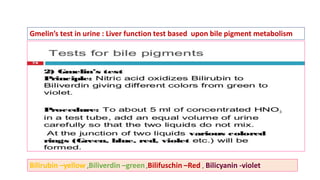
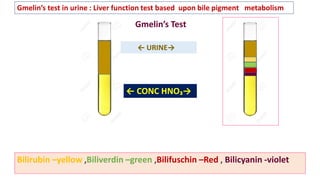
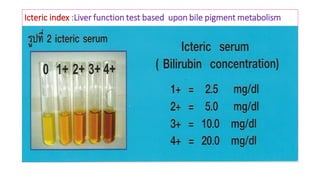
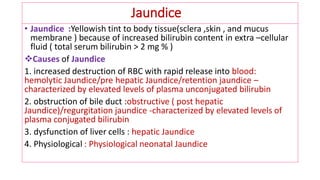
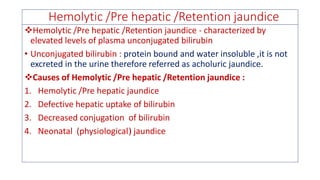
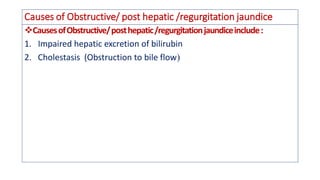
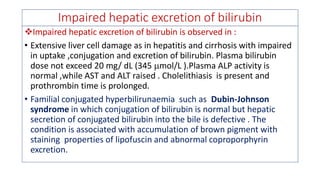
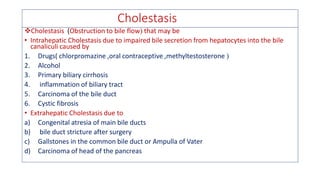
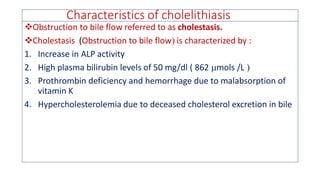
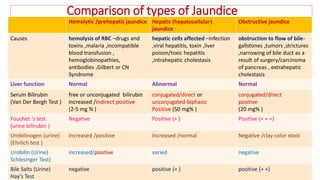
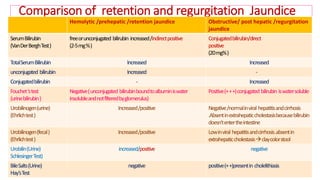
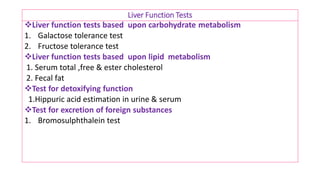
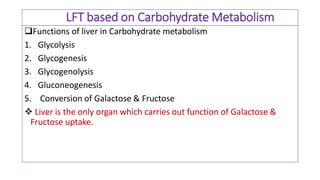
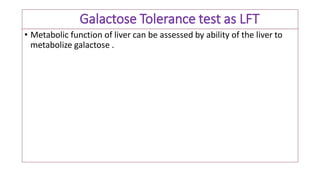
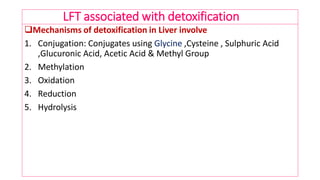
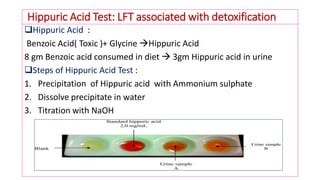
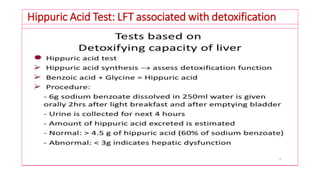
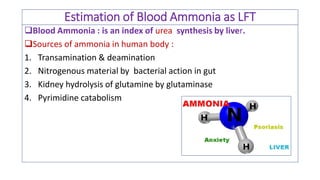
The document provides an overview of liver function tests (LFT) and their clinical applications, detailing the liver's structure and functions including metabolism, detoxification, and excretion. It categorizes LFTs based on biochemical findings and clinical aspects, which aid in diagnosing liver diseases, assessing cell damage, and monitoring treatment responses. Additionally, it discusses the importance of bile pigment metabolism and tests related to jaundice, emphasizing the relationship between bilirubin levels and various types of jaundice.
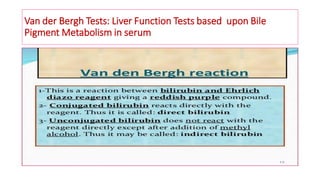
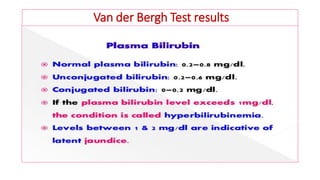
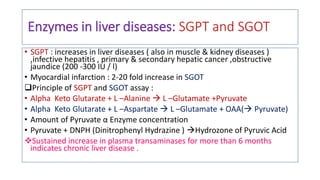
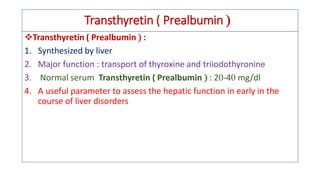
![Van der Bergh Test : Liver Function Tests based upon Bile Pigment Metabolism
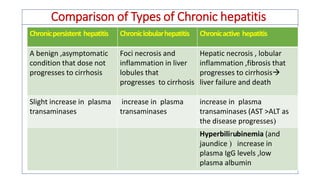
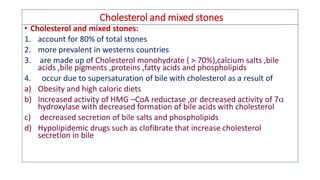
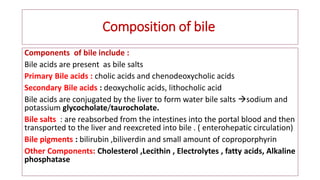
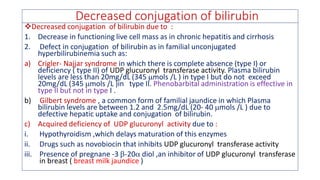
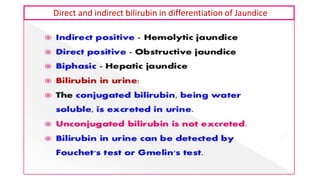
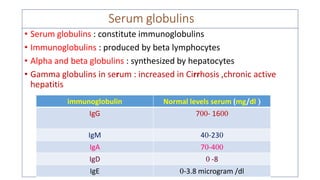
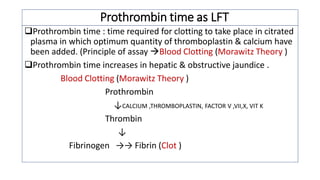
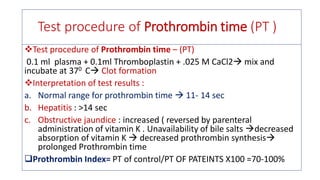
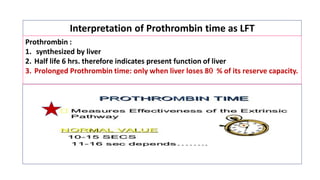
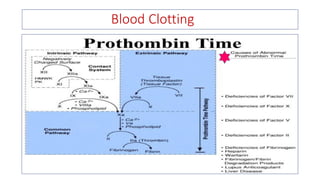
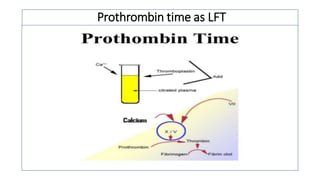
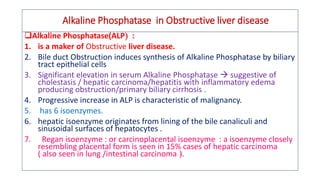
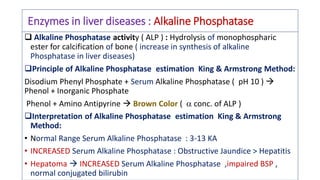
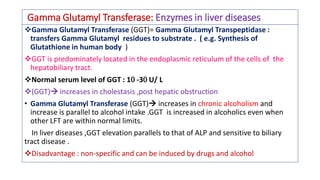
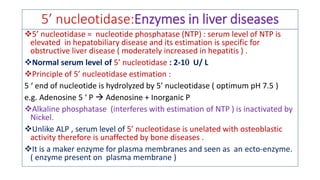
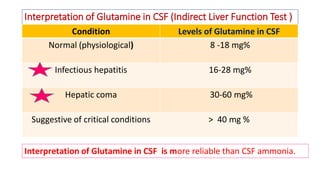
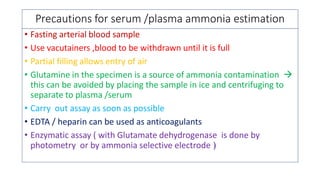
• Serum + Van der Bergh reagent violet complex Direct bilirubin / Conjugated
bilirubin =[ A]
• Serum + Alcohol *+ Van der Bergh reagent violet complex Direct + Indirect
bilirubin = Total bilirubin= [B]
• *Alcohol solubilizes proteins of free /indirect bilirubin
• Total bilirubin [B] - Conjugated bilirubin [A]= Indirect bilirubin](https://image.slidesharecdn.com/liverfunctiontestsandtheirclinicalapplications-180320142151/85/Liver-function-tests-and-their-clinical-applications-42-320.jpg)
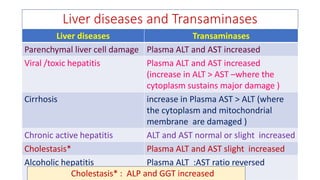
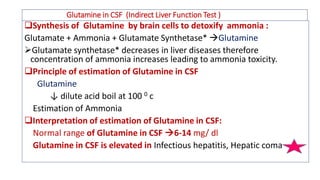
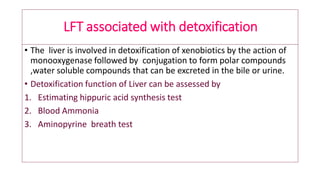
![Aminopyrine breath test
• Aminopyrine breath test: involves measurement of 14 CO2 formed
from [14 C]methyl labeled aminopyrine in liver by N-demethylation .
• In liver diseases such as cirrhosis and hepatitis ,the amount of 14 CO2is
decreased .](https://image.slidesharecdn.com/liverfunctiontestsandtheirclinicalapplications-180320142151/85/Liver-function-tests-and-their-clinical-applications-148-320.jpg)