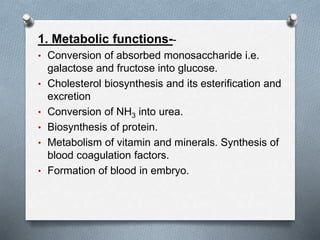
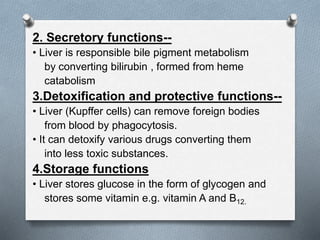
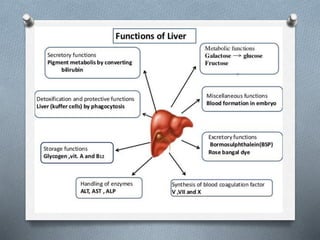
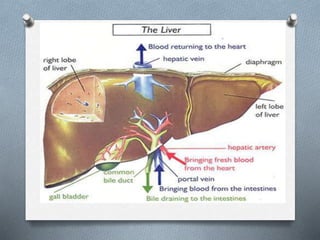
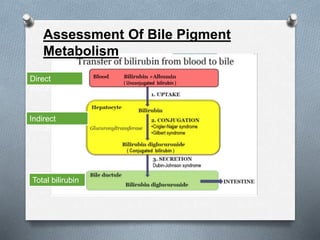
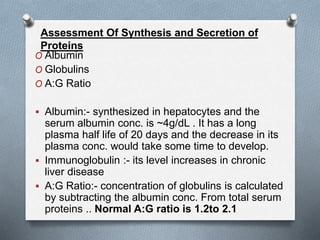
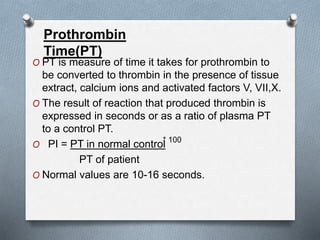
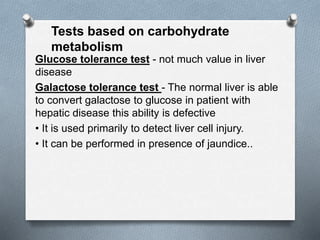
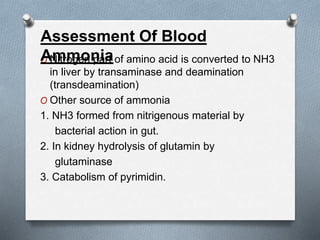
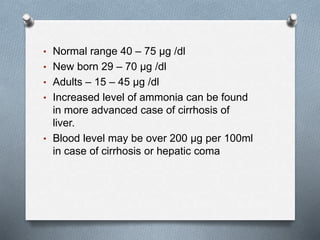
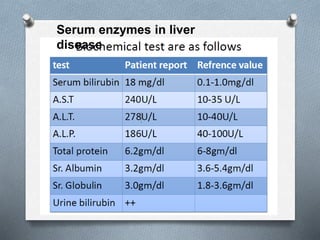
The liver performs many essential metabolic functions and is susceptible to various diseases. Liver function tests assess the status of the liver through biomarkers related to bile pigment metabolism, protein synthesis, clotting factor production, carbohydrate processing, and blood ammonia levels. Elevations in enzymes like bilirubin, AST, ALT, and prolongation of prothrombin time can indicate liver injury or disease states like viral hepatitis, cirrhosis, and alcoholic liver disease. A variety of other tests are also used to identify underlying etiologies or complications of liver disease.