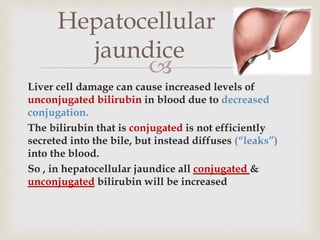
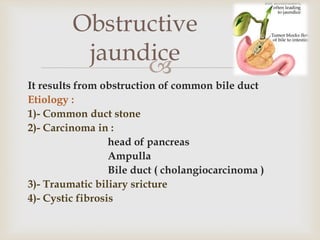
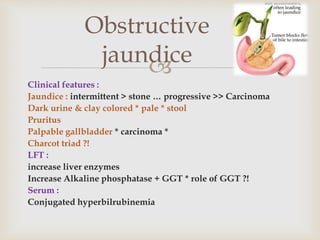
This patient, an 80-year-old African American female, presented with persistent jaundice for 2 months following a laparoscopic cholecystectomy for gallstones. Her jaundice initially decreased after surgery but returned, and she now has itching and tea-colored urine. Her weight has decreased 30 pounds over the past year despite good appetite. Physical exam showed jaundice but no signs of chronic liver disease. CT scan found nondilated bile ducts. The persistent jaundice following cholecystectomy suggests an underlying cause needs to be identified.