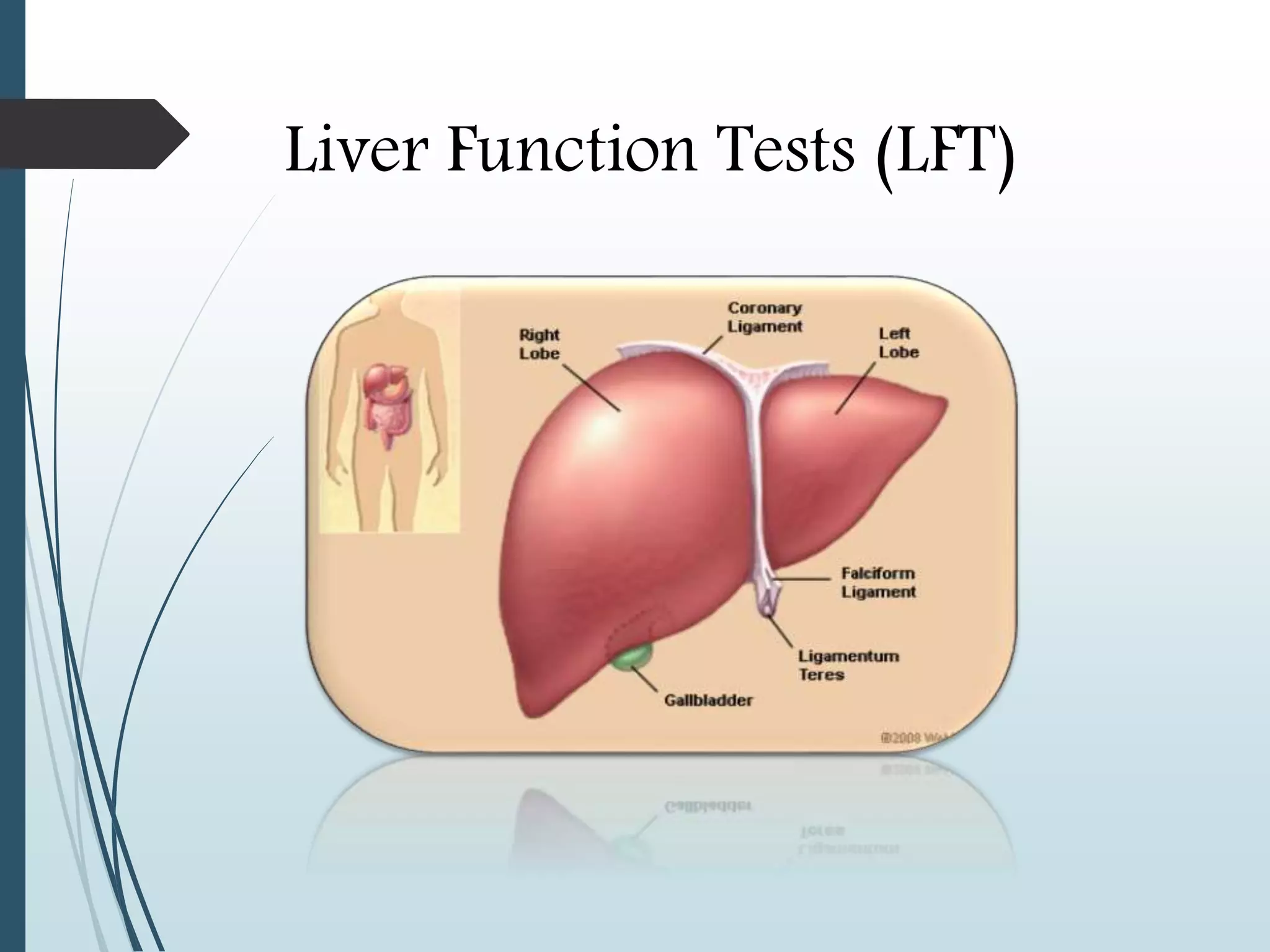
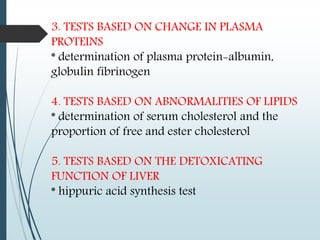
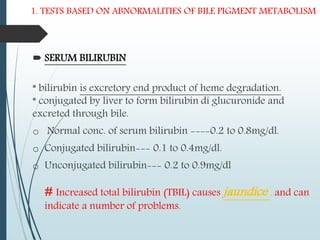
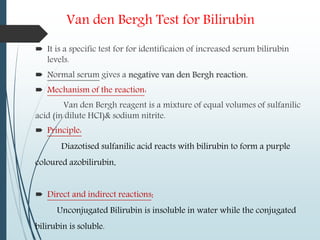
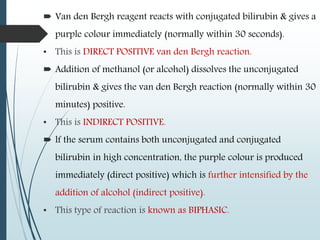
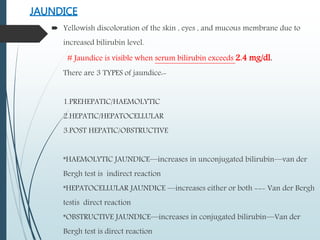
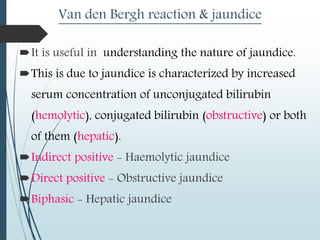
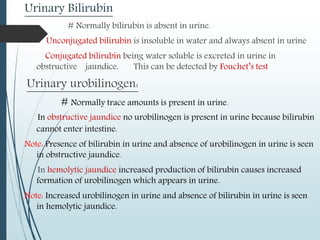
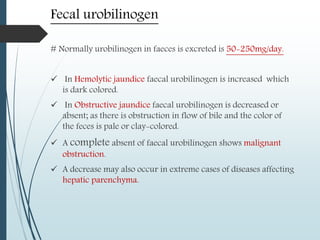
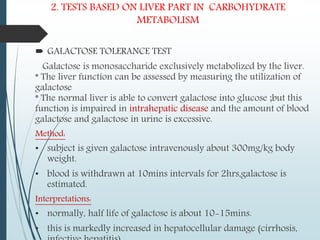
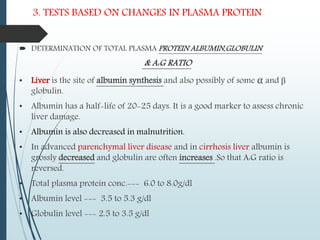
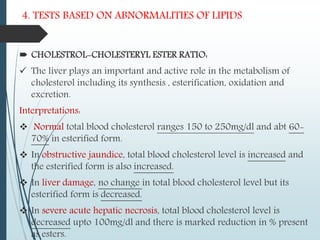
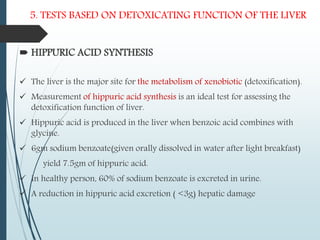
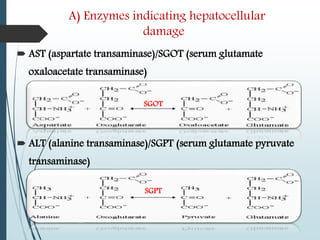
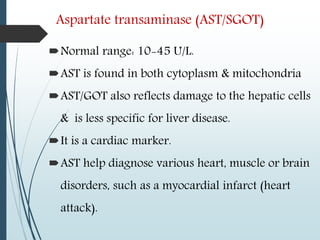
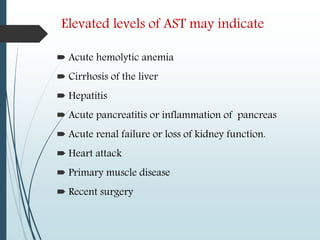
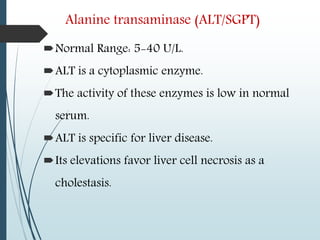
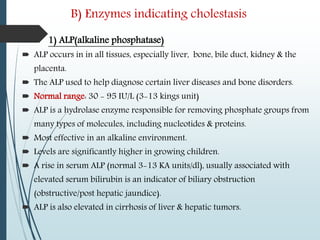
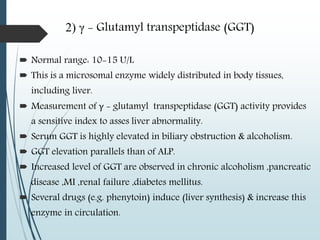
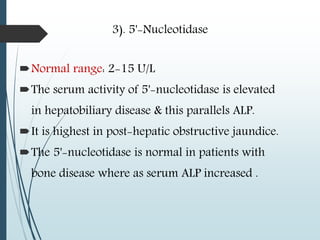
The document discusses liver function tests (LFTs). It begins by providing an overview of liver anatomy and functions. Key points include that the liver is the largest organ and performs many metabolic and excretory roles. LFTs evaluate the liver's functioning in these roles. The document then examines specific LFTs in detail, grouping them into those related to pigment metabolism, carbohydrate metabolism, plasma proteins, lipids, detoxification, excretion, blood clotting factors, blood ammonia, and serum enzymes. Elevations in different enzymes and analytes provide clues to conditions like hepatitis, cirrhosis, or obstruction. The tests discussed provide insights into liver health and disease.