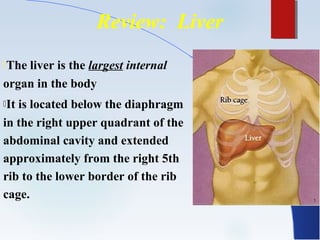
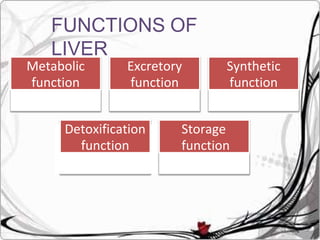
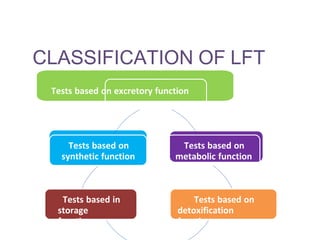
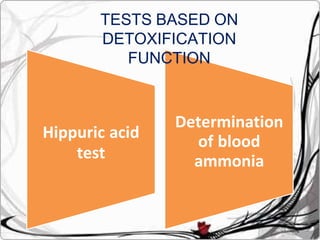
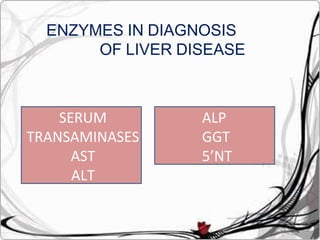
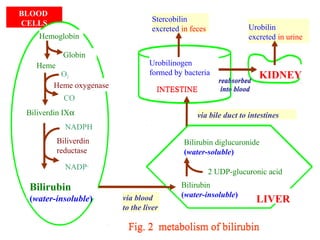
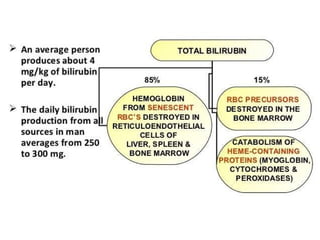
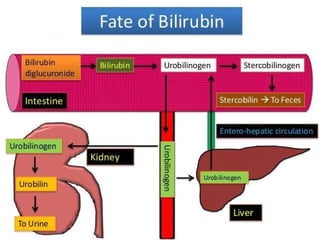
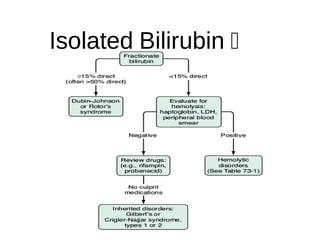
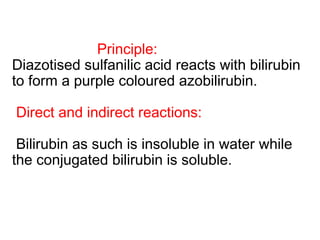
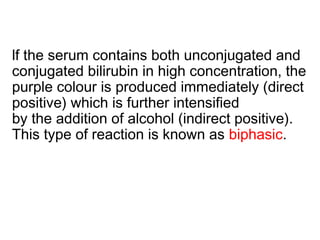
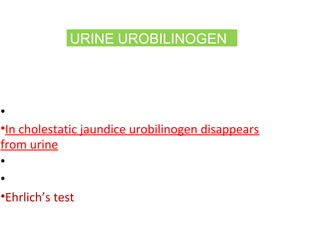
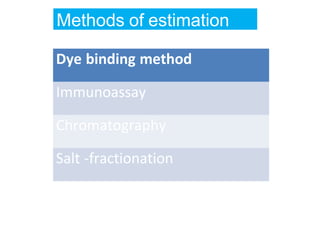
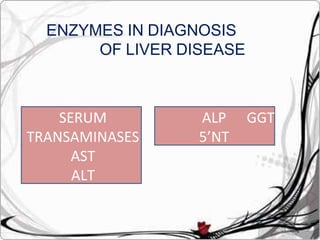
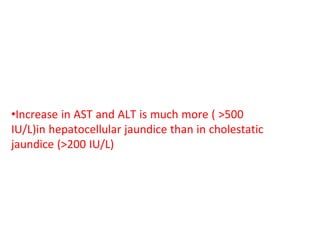
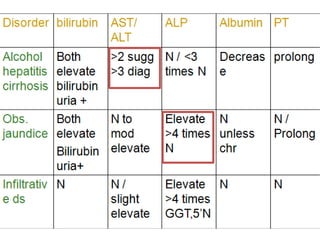
The document discusses various functions and tests of the liver. It begins by describing the liver's location and role in metabolism, storage, detoxification and other functions. It then discusses different types of liver function tests that evaluate the liver's excretory, metabolic, detoxification and other functions. Specific tests discussed include those measuring bilirubin, bile salts, enzymes and dye excretion. Causes and significance of abnormal results are also covered.