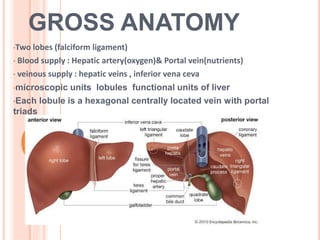
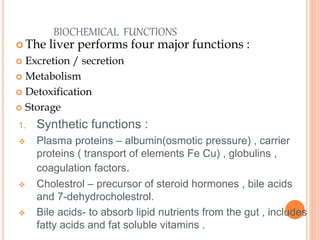
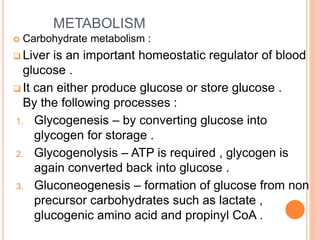
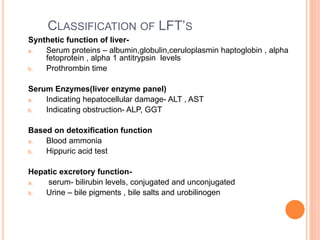
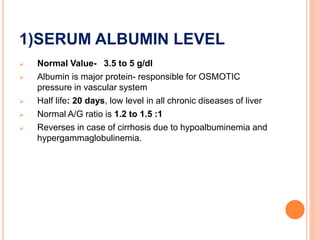
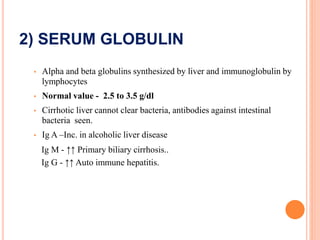
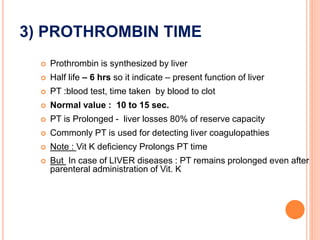
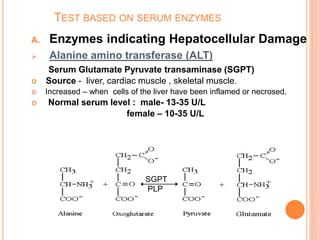
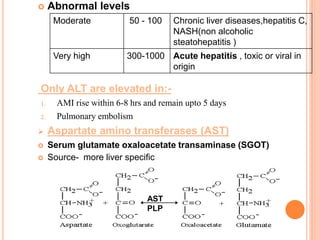
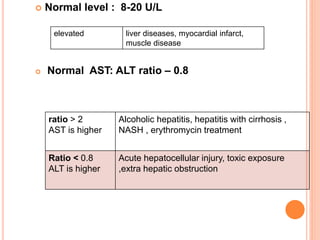
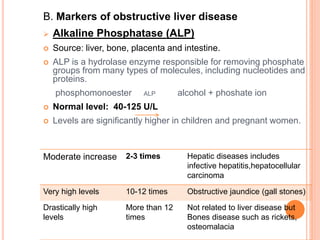
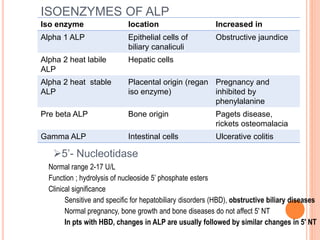
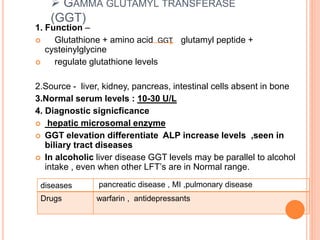
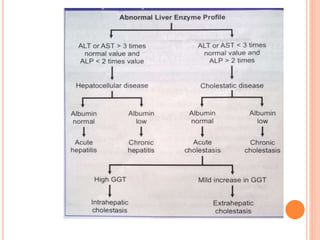
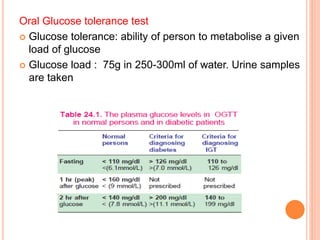
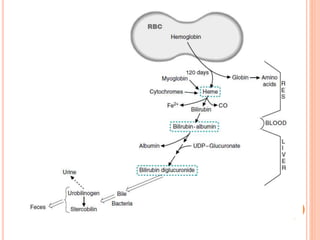
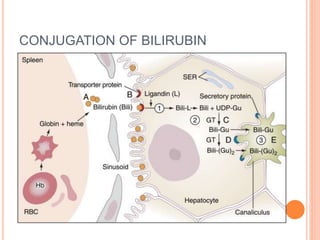
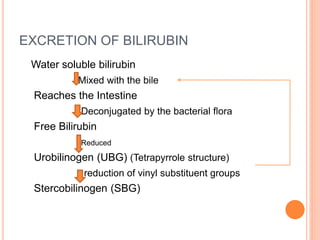
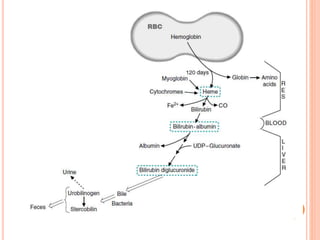
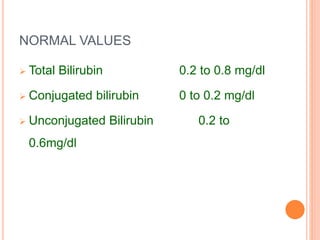
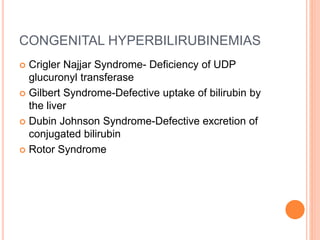
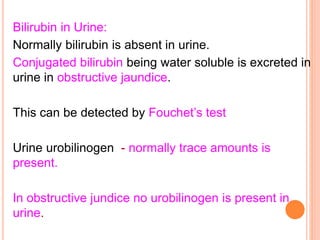
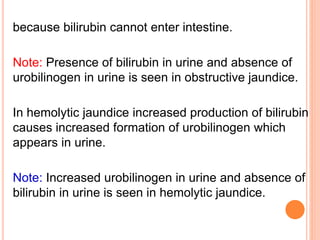
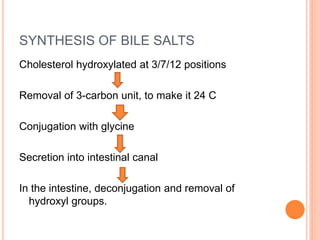
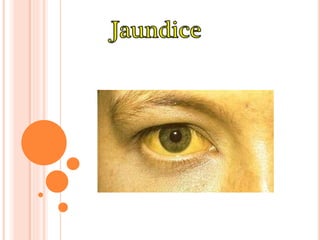
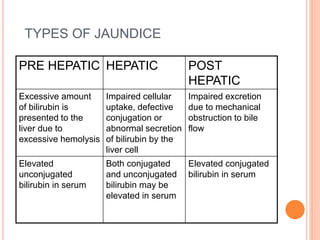
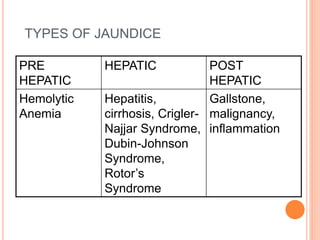
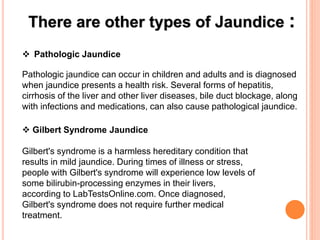
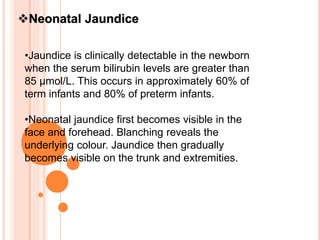
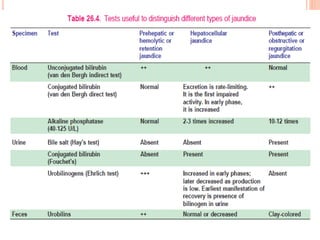
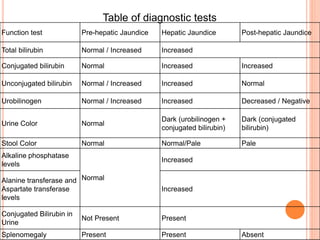
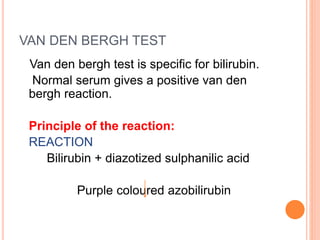
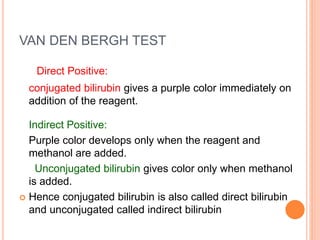
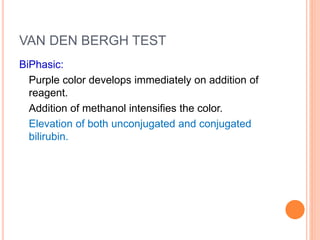
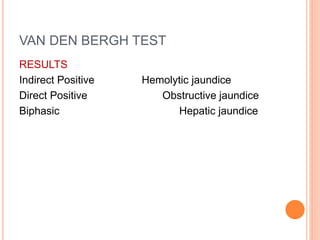
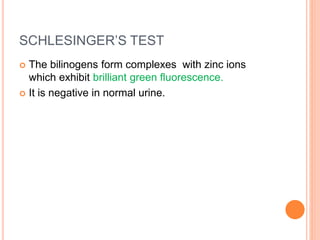
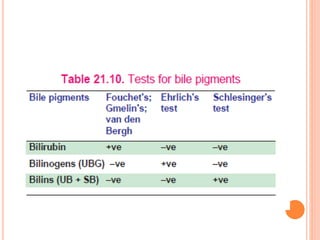
The document outlines the anatomy and functions of the liver, detailing its lobular structure, blood supply, and various metabolic processes including detoxification, storage, and synthesis of plasma proteins. It explains the significance of liver function tests (LFTs) in diagnosing liver disorders, highlighting specific tests for assessing liver damage, synthetic function, and excretory abilities. Additionally, the document describes jaundice types, bilirubin metabolism, and related diagnostic tests.