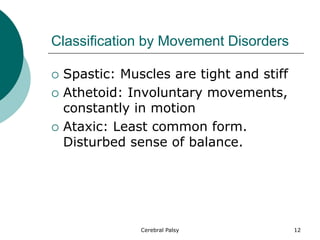
Cerebral palsy is a disorder of muscle movement and coordination caused by injury to the brain before or during infancy. It affects the part of the brain controlling body movement. Symptoms vary from mild awkwardness to virtually no muscle control and can include muscle tightness, involuntary movements, and difficulties with gross and fine motor skills. While there is no cure, early treatment including physical, occupational and speech therapy can help build strength and function. The goal is to help those with CP live as independently as possible.