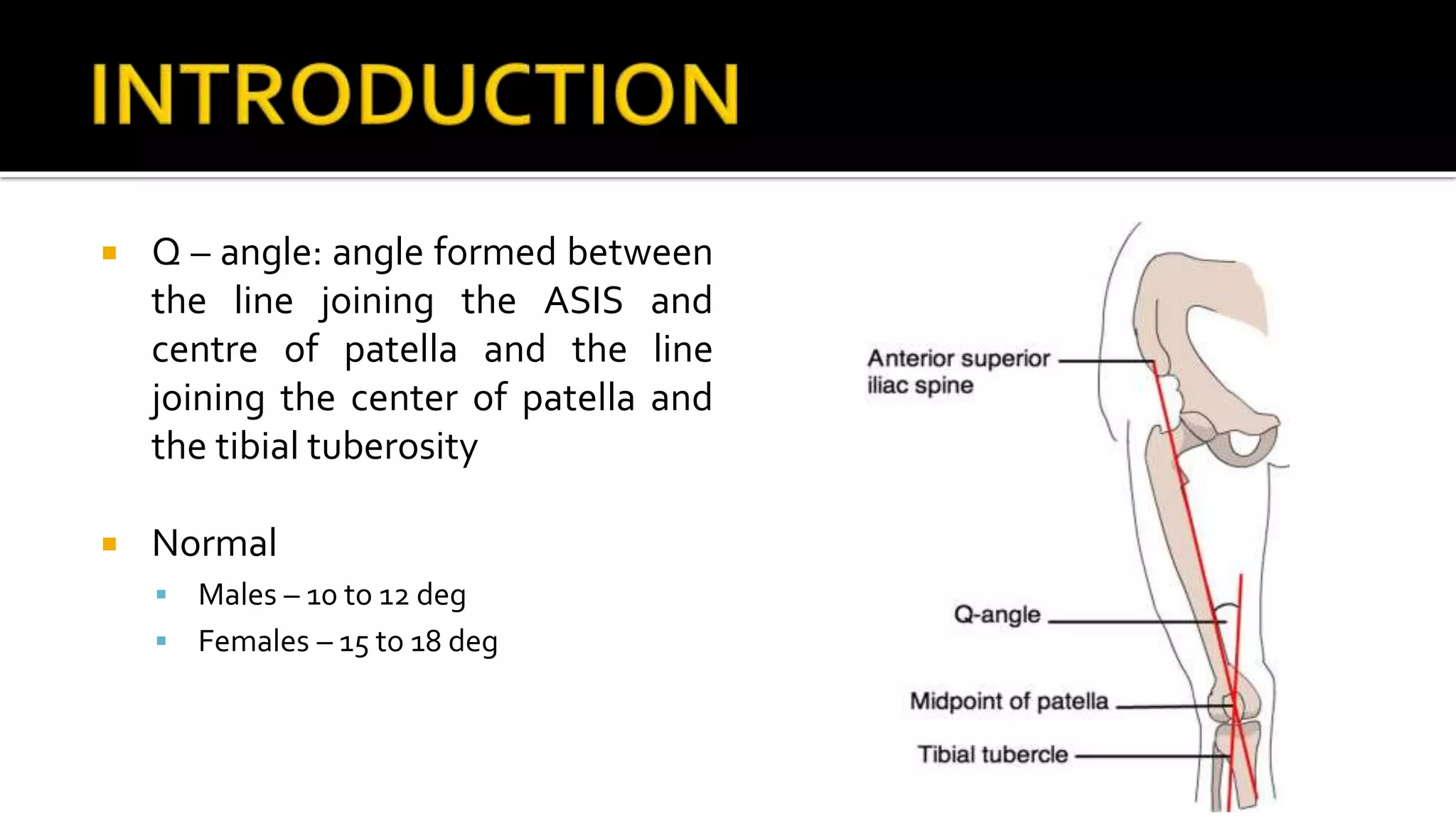
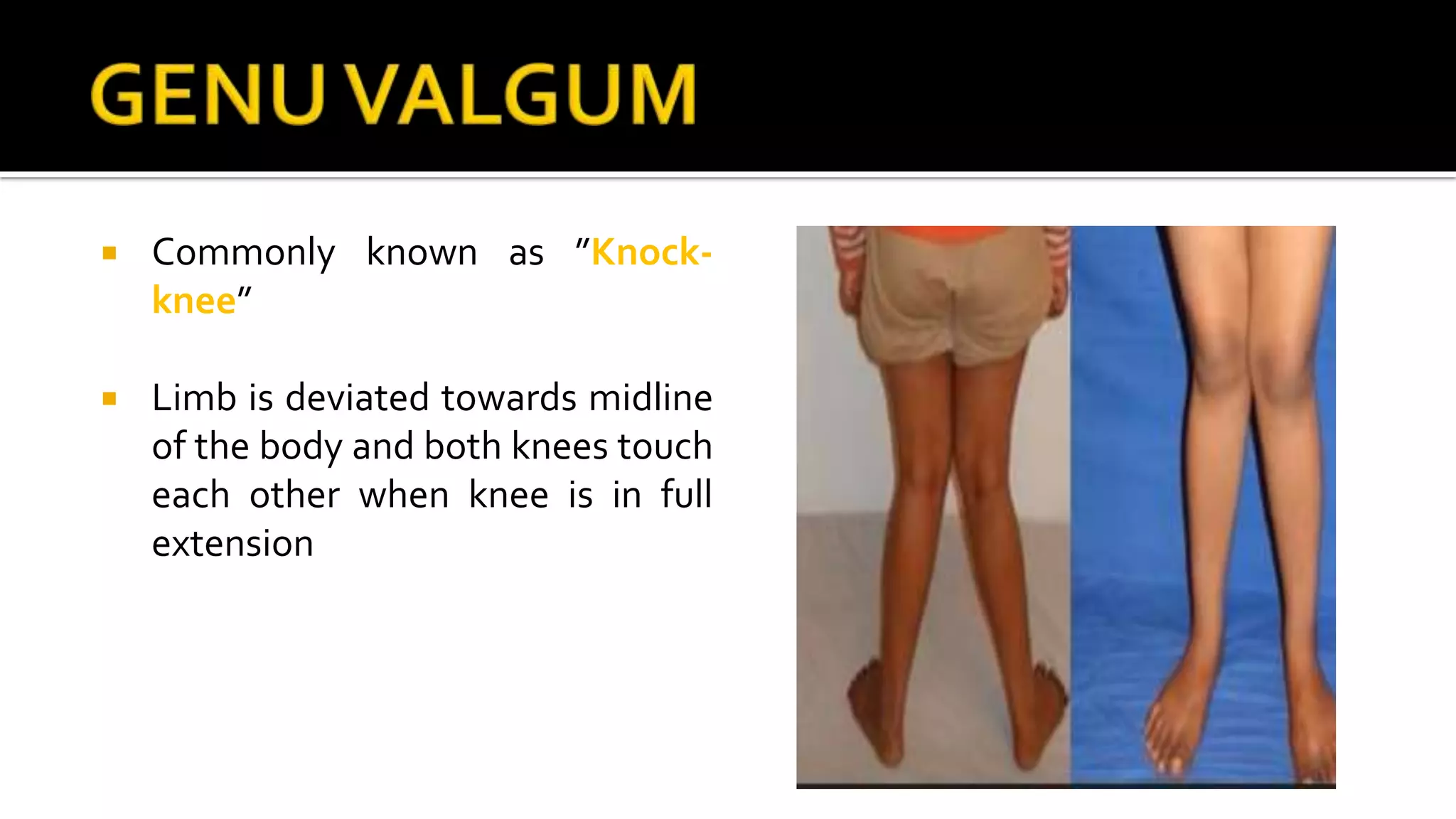
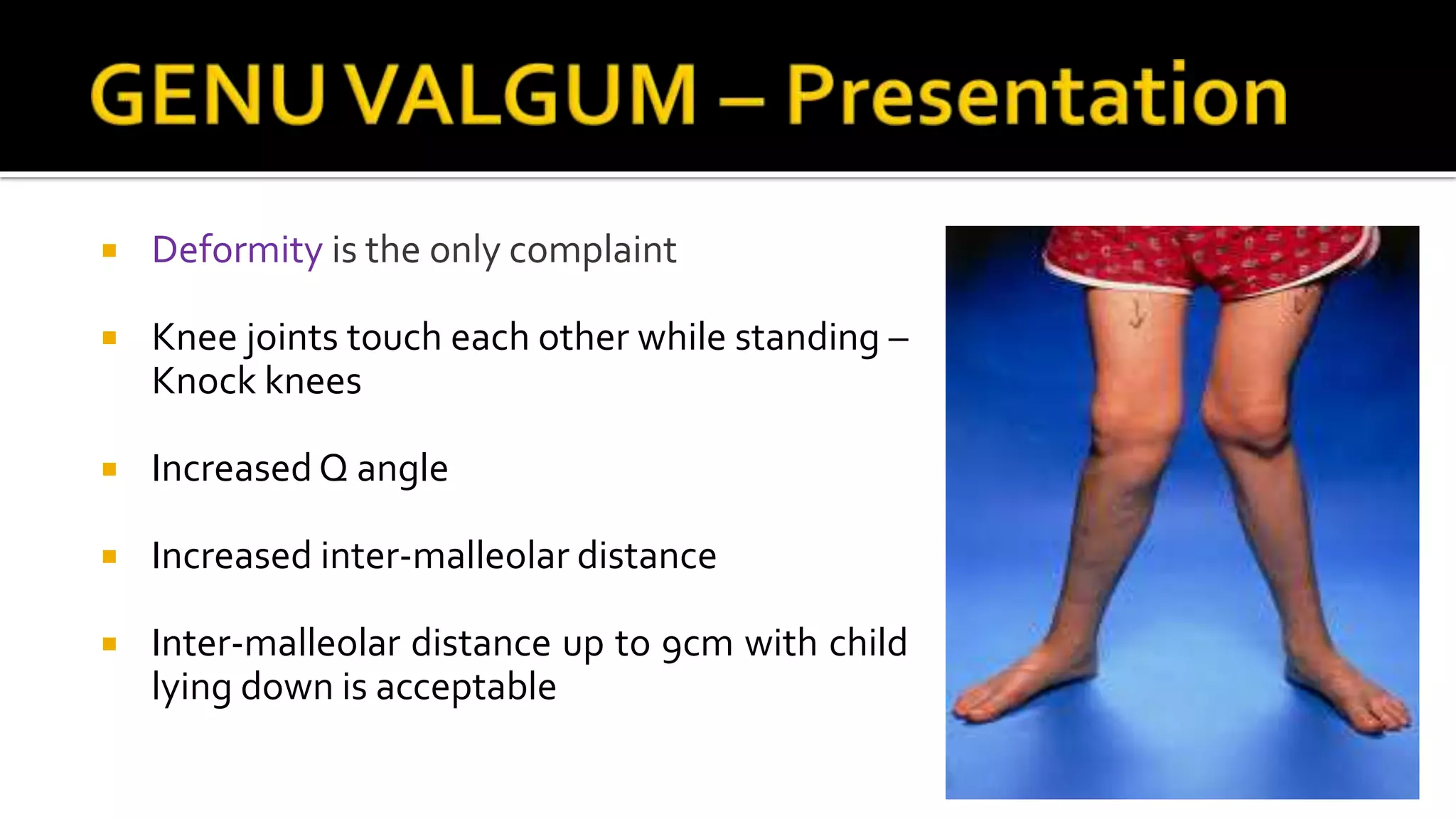
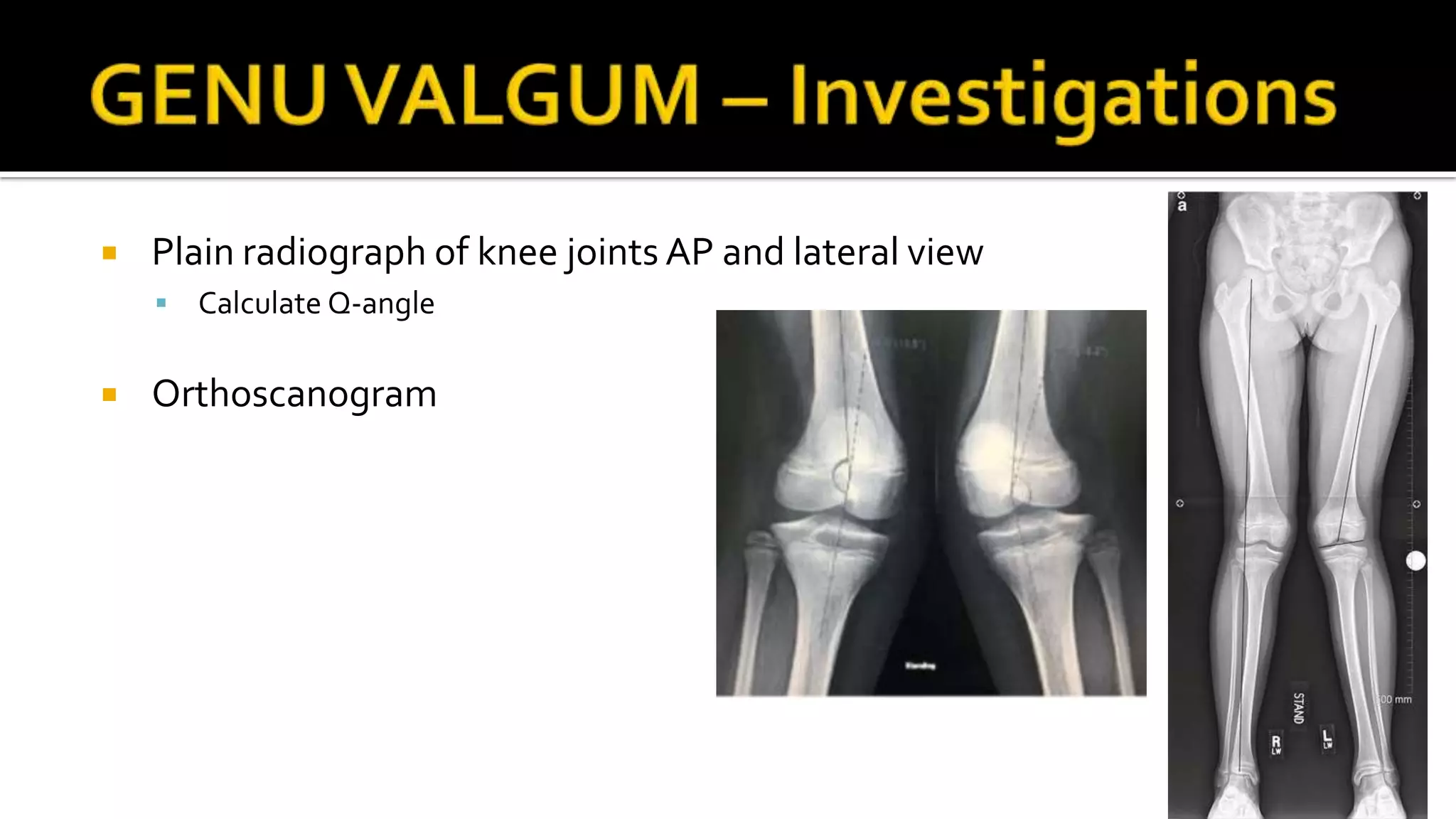
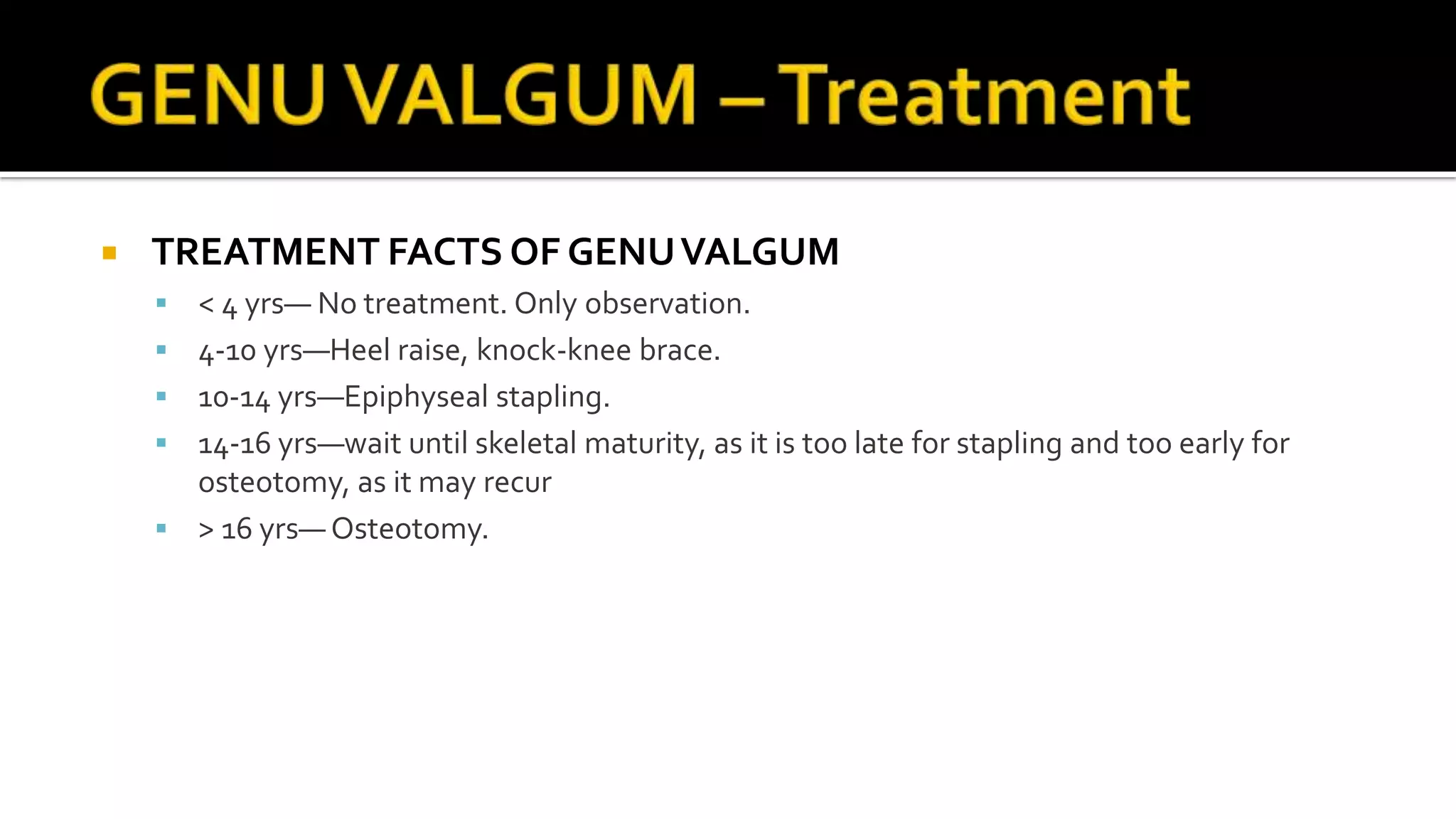
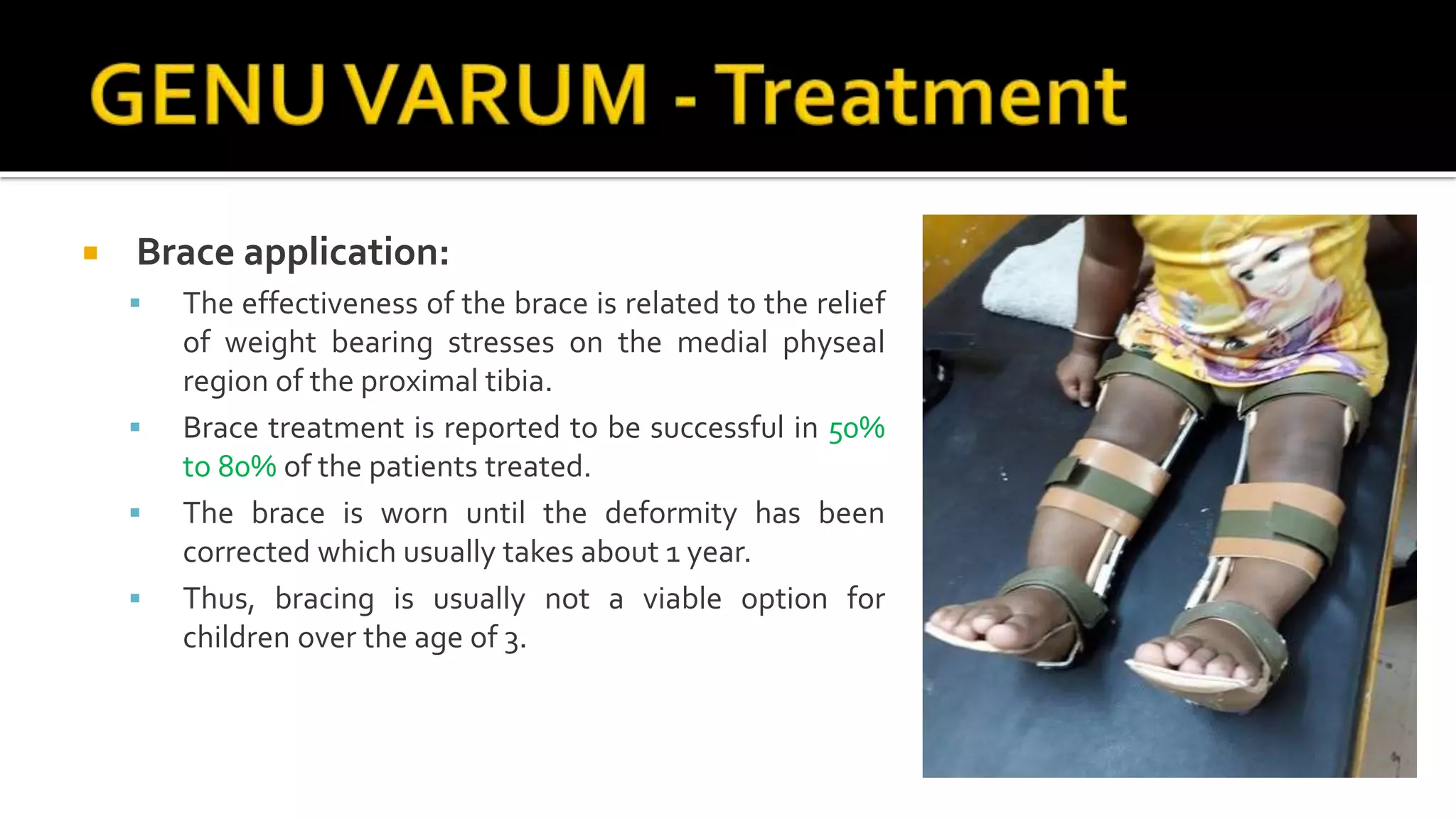
This document discusses genu valgum (knock knees) and genu varum (bowlegs). It defines the Q angle and normal ranges. Genu valgum can be physiological in children under 4 years old or pathological. Bilateral cases may be due to various conditions while unilateral cases are often due to trauma or injury. Evaluation involves physical exam and x-rays. Treatment depends on age but may include observation, bracing, hemiepiphysiodesis, or osteotomy. Genu varum is also normally physiological initially but becomes pathological after age 2. Causes in children and adults are discussed. Evaluation and treatment methods including bracing and surgery are outlined.