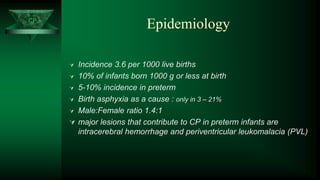
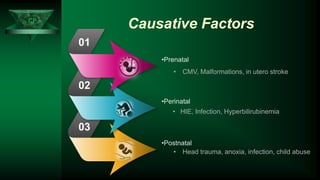
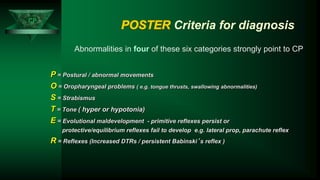
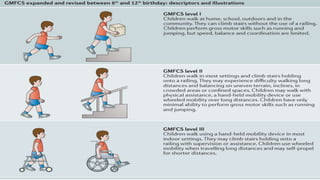
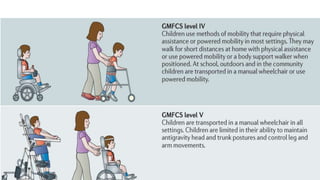
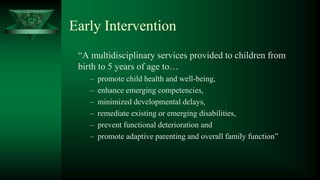
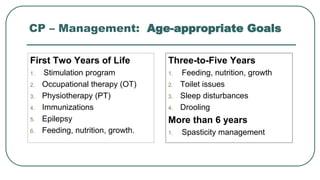
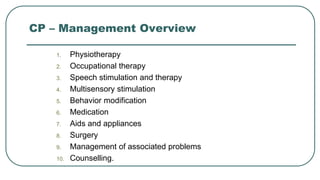
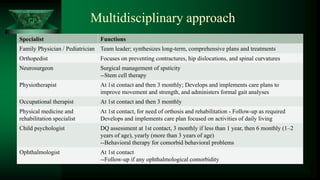
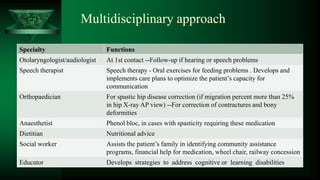
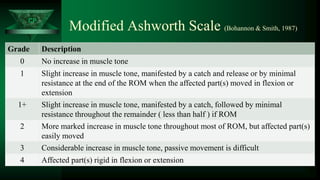
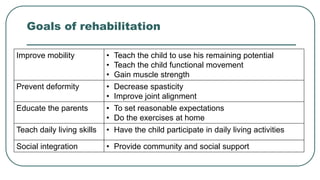
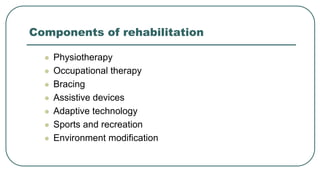
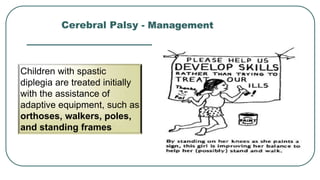
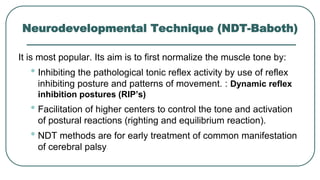
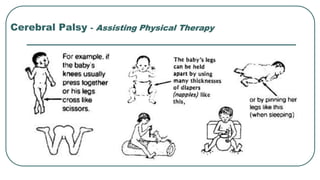
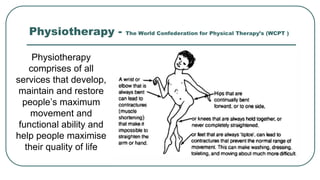
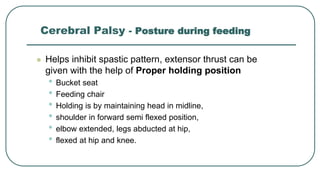
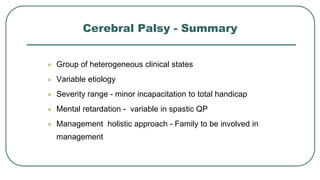
Cerebral palsy (CP) is the most common motor disability in childhood. It is caused by a non-progressive brain injury early in development. CP is characterized by disorders of movement and posture that limit activity. The document discusses the definition, epidemiology, classification, diagnosis, treatment, and management of CP. A multidisciplinary approach is needed to address the motor and associated disabilities of CP.