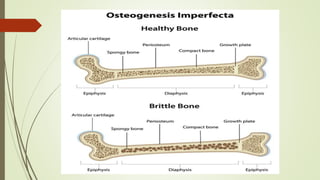
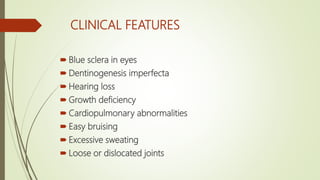
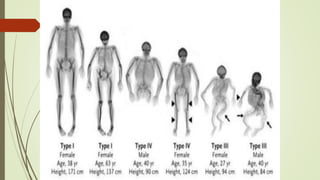
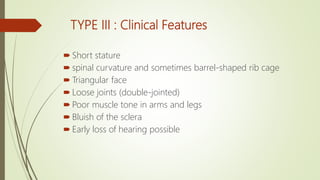
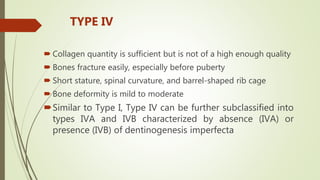
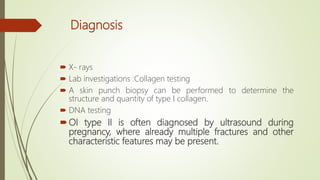
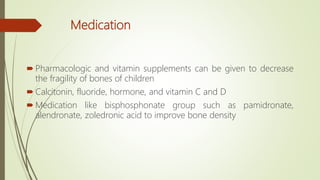
Osteogenesis imperfecta (OI) is a genetic disorder affecting type I collagen synthesis, leading to brittle bones and a range of musculoskeletal issues, classified into four main types based on severity. Clinical features vary, with symptoms such as blue sclera, hearing loss, and dental problems, and treatment focuses on managing fractures, improving bone strength, and facilitating mobility through therapy and surgical interventions. Although there is no cure, a healthy lifestyle and appropriate medical care can help manage symptoms and improve quality of life for those affected.