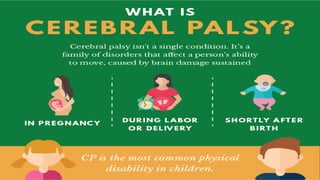
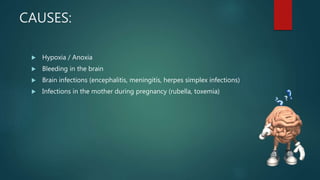
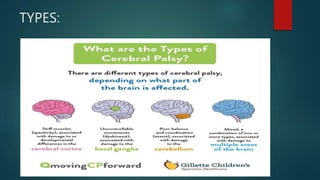
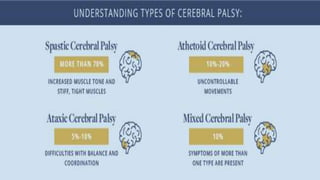
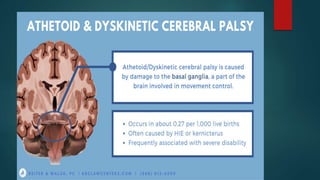
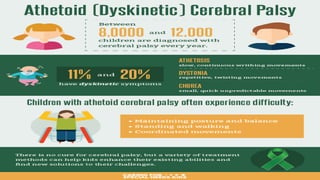
This document provides an overview of cerebral palsy, including its definition, causes, types, signs and symptoms, diagnosis, treatment, nursing considerations, complications, and educational options. Cerebral palsy is a group of disorders caused by damage to the developing brain that affects movement and posture. The main types are spastic, dyskinetic, and mixed. Treatment involves rehabilitation, physical/occupational therapy, medications, and assistive devices to improve function and independence. Nursing focuses on meeting physical, educational and psychosocial needs.