Poliomyelitis is an infectious viral disease primarily affecting children under five, characterized by flaccid paralysis due to the destruction of motor neurons. The disease progresses through several phases, including acute, convalescent, and chronic, with varying degrees of paralysis and the potential for deformities due to muscle imbalances. Management involves a comprehensive physiotherapy program, supportive care, and, if necessary, surgical interventions to correct deformities and improve function.

![TREATMENT PROGRAMME
A. Acute phase [first 3-5 weeks]
B. Recovery phase [4-18 weeks]
C. Chronic or residual phase [ after 1
year to 18 months]](https://image.slidesharecdn.com/poliomyelitis1-200518224619/85/Poliomyelitis-29-320.jpg)


![LATE CONVALESCENCE
[6 MONTH TO 1 YEAR]
• Phase of recovery that is due to hypertrophy of
residual muscle fibers that needs adequate
Programme of graded resistance to the
concerned muscles
• Resistance become more acceptable when
given during the performance of daily activities](https://image.slidesharecdn.com/poliomyelitis1-200518224619/85/Poliomyelitis-56-320.jpg)
![CHRONIC OR RESIDUAL
PHASE [AFTER 1 YEAR TO 18
MONTHS]
• More emphasis on strengthening
• Functional exercise than specific muscle training
• Movement should be made stronger by graduated
resistances
• Any additional guidance aids or supports to
facilitate functional as well as physical work
requirements given
• Prevent posture, position and activities that put
compressive forces on the involved muscles and](https://image.slidesharecdn.com/poliomyelitis1-200518224619/85/Poliomyelitis-58-320.jpg)
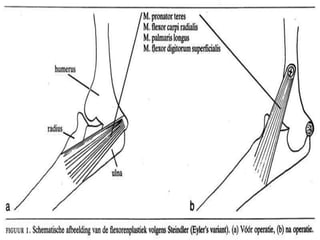
![• Paralysis of flexor of elbow results in loss of active
flexion at the elbow
• However, if the forearm and fingers are strong, the
common origin of flexor group of muscles, at the
medial epicondyle of humerus is transferred to the
front of lower end of humerus [steindler’s
flexoroplasty]](https://image.slidesharecdn.com/poliomyelitis1-200518224619/85/Poliomyelitis-72-320.jpg)
![• Function at the wrist can be improved by
tendon transfer or by fusion of wrist
• Wrist flexors are transferred to the finger
extensors to improve extension of the fingers
• In the hand, loss of opposition is a disabiling
problem and may require a tendon transfer
[opponensplasty]](https://image.slidesharecdn.com/poliomyelitis1-200518224619/85/Poliomyelitis-75-320.jpg)


![FOOT
• Contracture of planter
fascia produces a
cavus deformity of foot
• Tight planter fascia is
striped from its
attachment to the
calcaneus [Steindler's
operation]](https://image.slidesharecdn.com/poliomyelitis1-200518224619/85/Poliomyelitis-86-320.jpg)
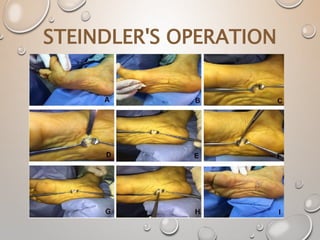
![• In younger children, the deformity is
corrected by a two-staged surgical
procedure.
• In first stage, cavus deformity is corrected
by fusion of talonavicular joint and
release of tight planter fascia [steindler’s
operation]
• A below knee plaster cast is maintained](https://image.slidesharecdn.com/poliomyelitis1-200518224619/85/Poliomyelitis-101-320.jpg)
![• The 1st metatarsal drop is corrected by an
operation [modifies jones’ operation]
consisting of transfer of extensor hallucis
longus tendon into neck of first
metatarsal and fusion of IP joint of big-
toe](https://image.slidesharecdn.com/poliomyelitis1-200518224619/85/Poliomyelitis-108-320.jpg)
![• Moderate to severe paralysis of lower
extremity result in shortening of
affected limb
• Methods:
Shortening of normal [or longer] limb
Lengthening of affected [short] limb](https://image.slidesharecdn.com/poliomyelitis1-200518224619/85/Poliomyelitis-114-320.jpg)
![SHORTENING OF NORMAL [OR
LONGER] LIMB
• Normal limb may be shortened by
arrest of the epiphyseal growth or by
resection of bone from the femur or
tibia
• Rarely performed](https://image.slidesharecdn.com/poliomyelitis1-200518224619/85/Poliomyelitis-115-320.jpg)
![LENGTHENING OF AFFECTED
[SHORT] LIMB
• Its undertaken in femur or tibia
depending on the site of shortening
• Degree of real shortening of limb is
measured both clinically and by
scanogram](https://image.slidesharecdn.com/poliomyelitis1-200518224619/85/Poliomyelitis-116-320.jpg)

![• Lengthening of femur or tibia can be
undertaken by any of the following
methods:
• Tubular fixators [wagener’s technique]
• Ring fixator [ilizarov technique]](https://image.slidesharecdn.com/poliomyelitis1-200518224619/85/Poliomyelitis-118-320.jpg)
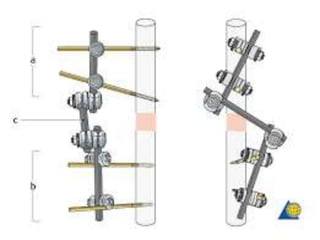
![TUBULAR FIXATORS [WAGENER’S
TECHNIQUE]
• Femur is osteotomized [cut] through the
shaft and an external fixator [with
distractor] is applied
• The femur is then gradually distracted every
day, achieving the desired amount of
lengthening over a period of time [usually
in weeks]](https://image.slidesharecdn.com/poliomyelitis1-200518224619/85/Poliomyelitis-119-320.jpg)
![RING FIXATOR [ILIZAROV
TECHNIQUE]
• In this method, thin wires are passed
into the bone under tension and
connected to half-or full circle signs
• The most commonly used ring fixator
is called ilizaov fixator, after its
innovator](https://image.slidesharecdn.com/poliomyelitis1-200518224619/85/Poliomyelitis-125-320.jpg)
![• The bone is cut [by corticotomy] in the
area of metaphysis [either the proximal
or distal] and gradual distraction is
done to increase the length of the
bone to increase the length of bone
• New bone, called regenerate forms into
the gap, thus created by distraction](https://image.slidesharecdn.com/poliomyelitis1-200518224619/85/Poliomyelitis-126-320.jpg)