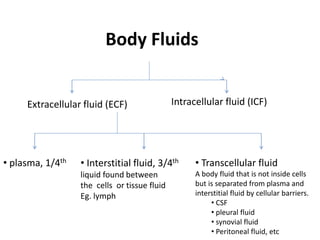
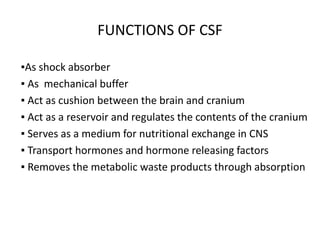
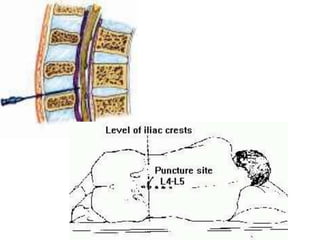
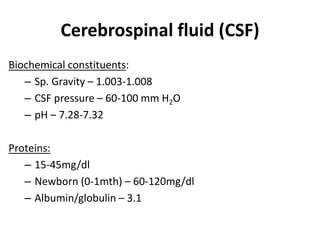
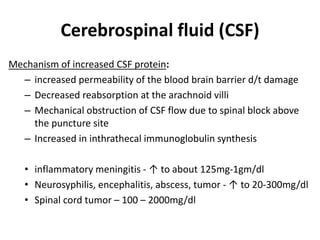
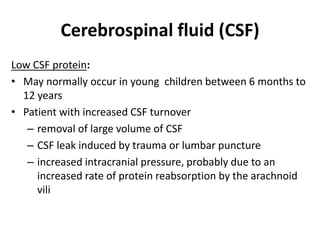
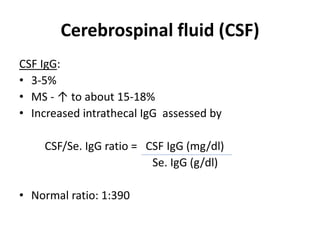
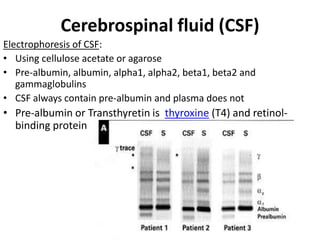
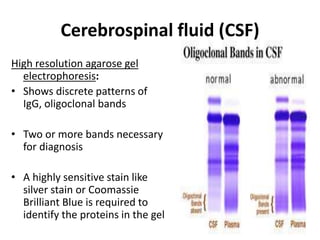
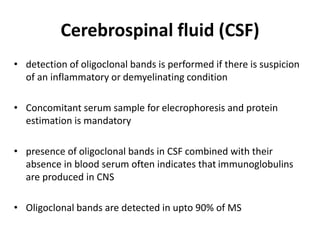
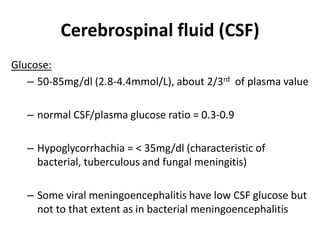
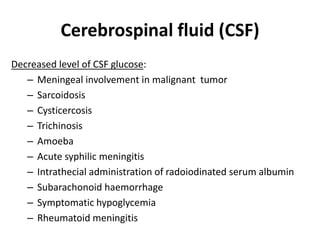
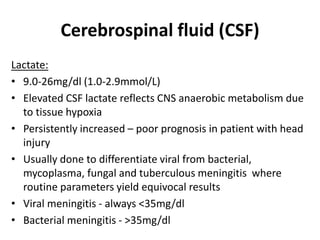
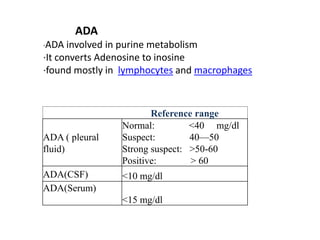
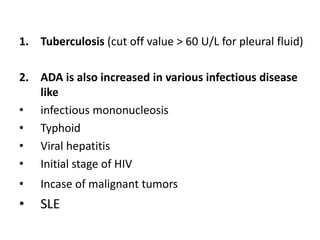
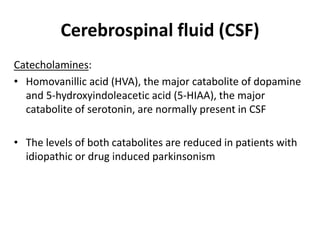
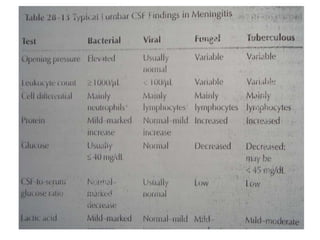
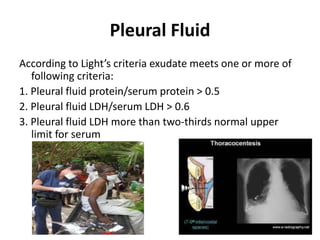
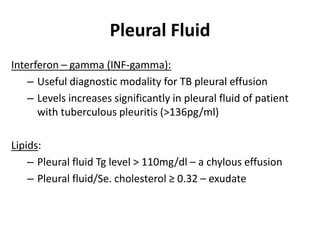
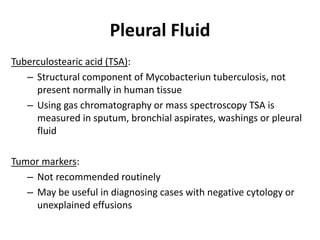
This document discusses various body fluids, including cerebrospinal fluid (CSF), pleural fluid, and peritoneal fluid. It provides details on the production, composition, and evaluation of these fluids. Key points include that CSF is produced in the brain ventricles and circulates around the brain and spinal cord, transporting nutrients and removing waste. Pleural and peritoneal fluids accumulate as exudates or transudates depending on fluid balance mechanisms. Biochemical analysis of these fluids can help diagnose conditions like meningitis, tuberculosis, and liver disease.