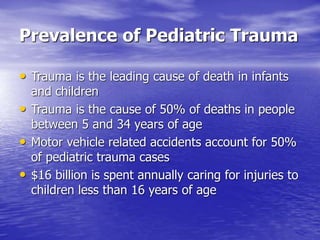
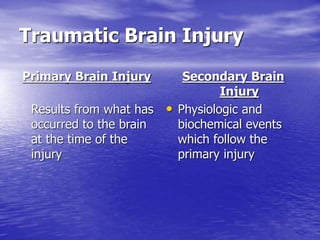
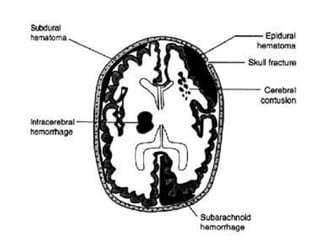
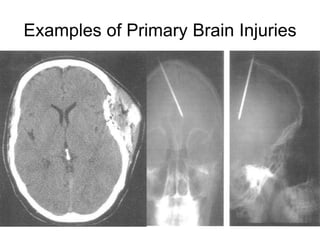
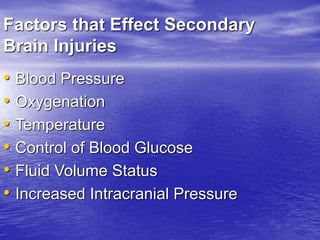
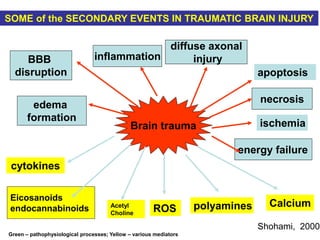
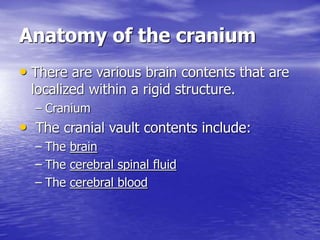
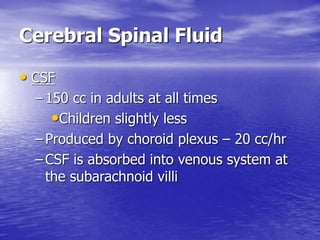
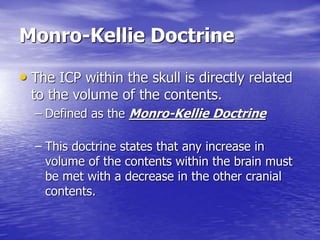
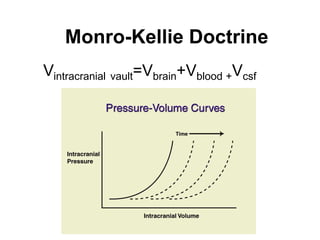
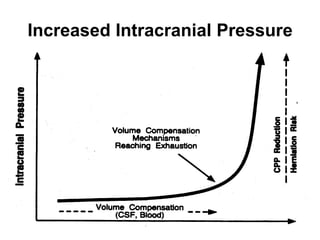
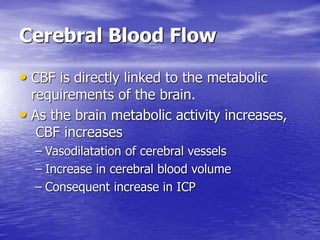
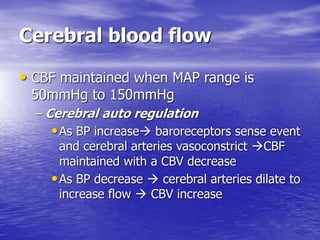
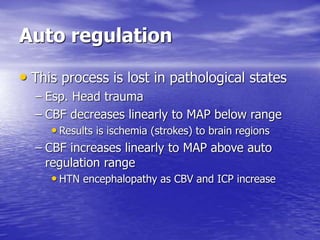
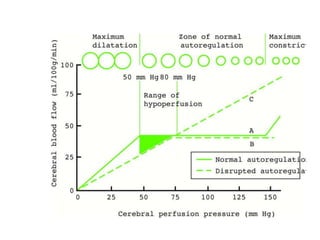
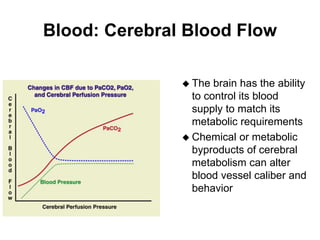
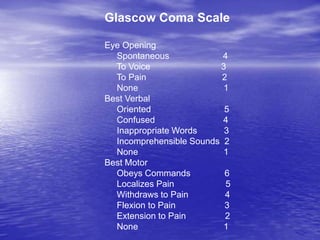
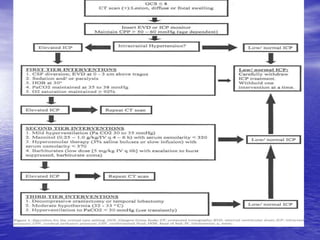
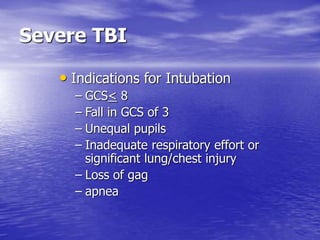
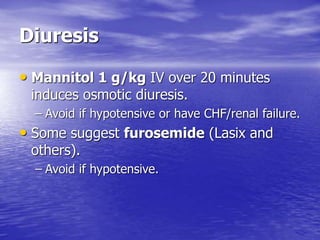
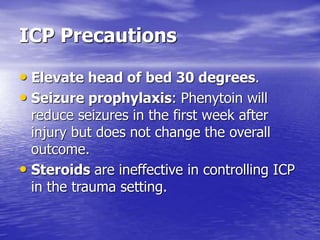
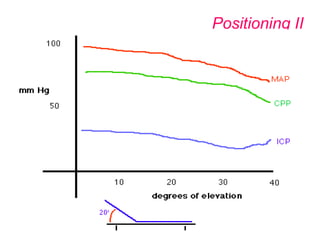
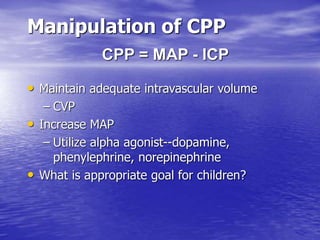
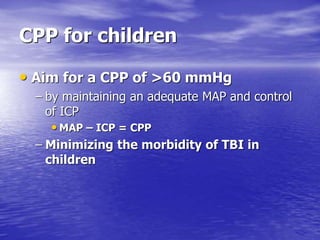
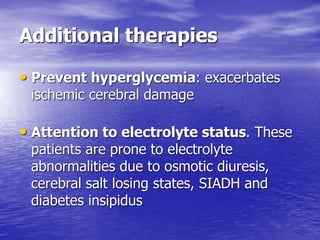
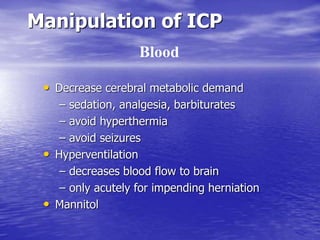
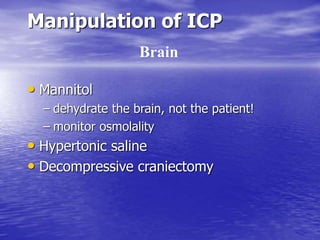
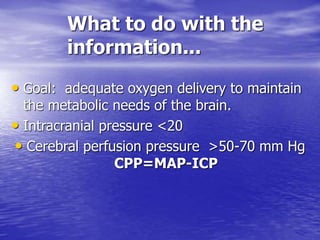
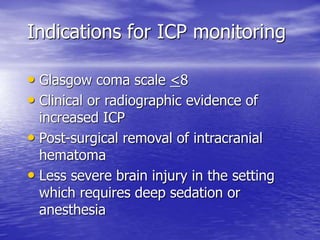
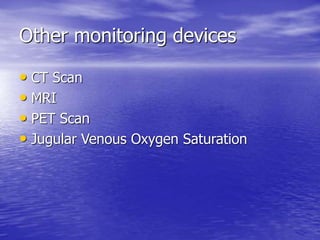
This document discusses head injuries and traumatic brain injury (TBI) in children. It notes that head injuries are a leading cause of disability and death in children. TBI can cause both primary and secondary brain injuries. Secondary injuries involve physiological and biochemical events after the initial injury that can exacerbate damage. Intracranial pressure (ICP) is an important factor, as the skull has a fixed volume, so any increase in one component (e.g. blood, brain) must be offset by a decrease in another. ICP monitoring is important for managing TBI patients. The goal is to maintain adequate cerebral perfusion pressure while controlling ICP through interventions like sedation, hyperventilation, mannitol, and hyper

![Near-infrared Spectroscopy
• Uses absorption characteristics of oxy
Hgb, deoxy Hgb, and [o] cyt aa3
• Uses the ability to penetrate the superficial
brain
• Therefore the state of oxygenation can be
determined.
• Good assessment of cerebral oxygenation](https://image.slidesharecdn.com/icpsmith-220921163146-ce7ad550/85/ICP_Smith-ppt-47-320.jpg)