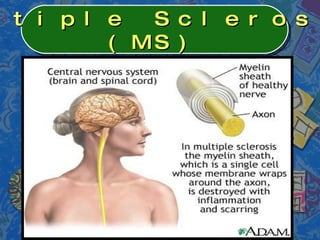
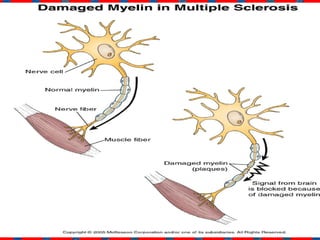
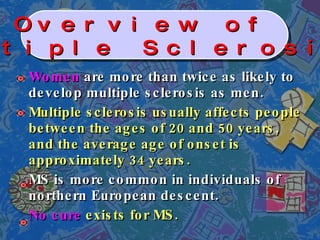
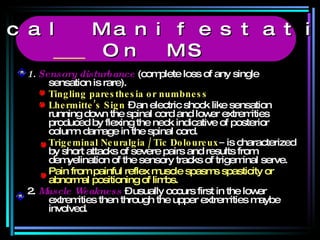
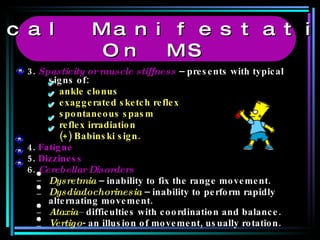
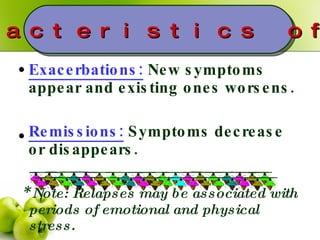
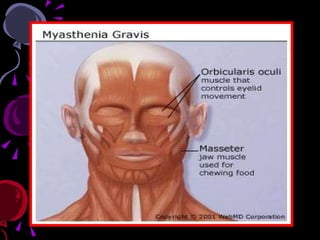
Multiple Sclerosis (MS) and Myasthenia Gravis (MG) are autoimmune disorders where the immune system attacks the body's own healthy cells. MS affects the central nervous system by damaging the protective myelin sheath surrounding nerve fibers, while MG affects the neuromuscular junction by blocking or destroying acetylcholine receptors. Common symptoms of MS include sensory issues, muscle weakness, fatigue and vision problems. MG symptoms often begin with eye weakness and drooping eyelids and may progress to generalized weakness. While there is no cure for either condition, treatments can help manage symptoms and delay disease progression.



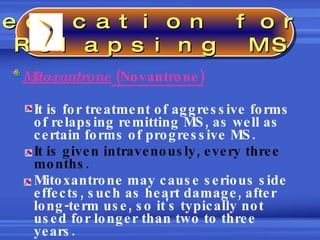
![Beta interferons Interferon beta-1b (Betaseron) ; [subcutaneously every other day] and interferon beta-1a (Avonex, Rebif) [subcutaneously three times a week] are genetically engineered copies of proteins that occur naturally in your body. They help fight viral infection and regulate your immune system. Beta interferons aren't used in combination with one another; only one of these medications is used at a time. Glatiramer (Copaxone) It works by blocking your immune system's attack on myelin. It is injected subcutaneously once daily. Side effects may include flushing and shortness of breath after injection. Natalizumab (Tysabri) This drug is administered intravenously once a month. It works by blocking the attachment of immune cells to brain blood vessels (a necessary step for immune cells to cross into the brain) thus reducing the immune cells' inflammatory action on brain nerve cells. Medication for Relapsing MS](https://image.slidesharecdn.com/autoimmunedisorders-091215033138-phpapp01/85/Autoimmune-Disorders-18-320.jpg)









![GBS typically begins with muscle weakness and diminished reflexes of the lower extremities. (Ascending from legs to arms). Weakness in their legs, manifesting as "rubbery legs" or legs that tend to buckle, with or without dysthesias (numbness or tingling). Facial diplegia (affecting like parts on both sides of the face; possibly accompanied by opthalmoplegia [ocular paralysis]) Hyporeflexia and weakness may progress to tetraplegia. Neuromuscular respiratory failure (due to demyelination of the nerves that innervate the diaphragm and intercostal muscles.) Clinical Manifestations on GBS](https://image.slidesharecdn.com/autoimmunedisorders-091215033138-phpapp01/85/Autoimmune-Disorders-46-320.jpg)