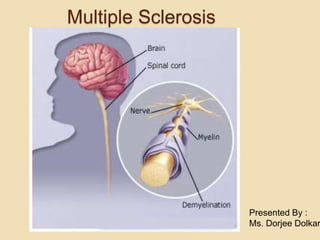
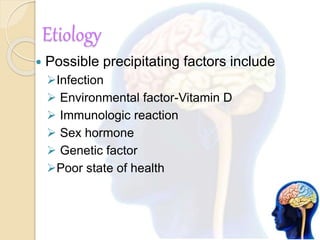
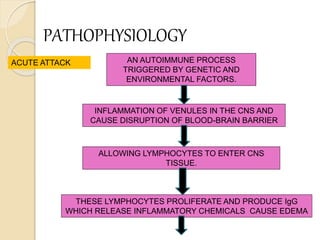
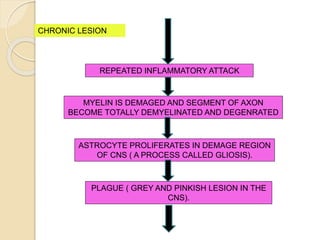
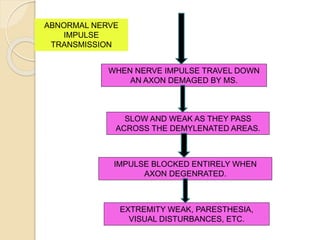
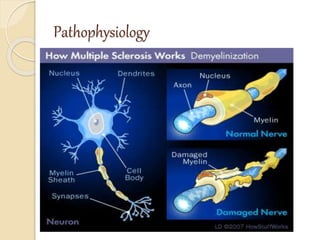
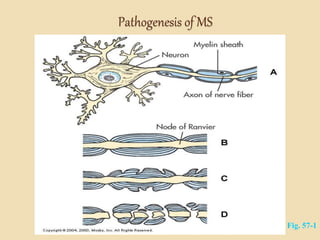
Multiple sclerosis is a chronic autoimmune disorder that affects the central nervous system through demyelination of nerve fibers. It typically presents in young to middle-aged adults and is more common in women. Symptoms can include visual disturbances, weakness, sensory changes, and impairments in coordination. Diagnosis involves MRI, spinal fluid analysis, and evoked potential tests. Treatment focuses on managing symptoms, reducing inflammation and relapses, and physical/occupational therapy. Nursing care centers around safety, mobility, self-care, and managing complications.