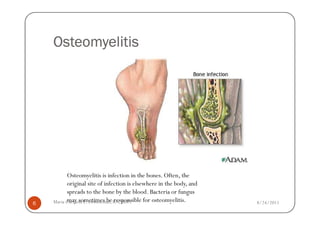
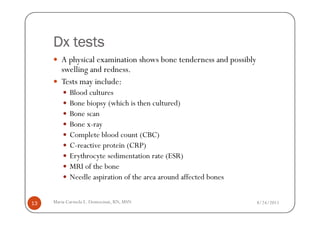
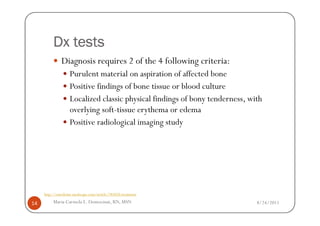
The document discusses musculoskeletal disorders, focusing on bone infections like osteomyelitis and septic arthritis. It covers their causes, risk factors, symptoms, diagnostic tests, and treatment options including antibiotics and surgery. The summary also highlights the importance of early diagnosis and intervention for better prognosis.

![Antibiotics
Linezolid (Zyvox)
Prevents formation of functional 70S initiation complex, which
is essential for bacterial translation process. Bacteriostatic
against staphylococci.
The FDA warns against the concurrent use of linezolid with
serotonergic psychiatric drugs, unless indicated for life-
threatening or urgent conditions. Linezolid may increase
serotonin CNS levels as a result of MAO-A inhibition,
increasing the risk of serotonin syndrome.[14]
30 Maria Carmela L. Domocmat, RN, MSN 8/24/2011](https://image.slidesharecdn.com/musculoskeletaldisorderspart1cld-110823222718-phpapp02/85/Musculoskeletal-disorders-part-1-30-320.jpg)
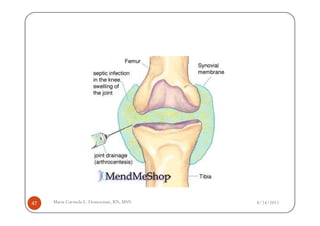
![Synovial Fluid Drainage
The choice of the type of drainage, whether percutaneous or surgical, has not
been resolved completely.[19, 25] In general, use a needle aspirate initially,
repeating joint taps frequently enough to prevent significant reaccumulation of
fluid. Aspirating the joint 2-3 times a day may be necessary during the first few
days. If frequent drainage is necessary, surgical drainage becomes more
attractive.
Gonococcal-infected joints rarely require surgical drainage.
Surgical drainage is indicated when one or more of the following occur:
The appropriate choice of antibiotic and vigorous percutaneous drainage fails to
clear the infection after 5-7 days
The infected joints are difficult to aspirate (eg, hip)
Adjacent soft tissue is infected
Routine arthroscopic lavage is rarely indicated. However, drainage through the
arthroscope is replacing open surgical drainage. With arthroscopic drainage, the
operator can visualize the interior of the joint and can drain pus, debride, and
lyse adhesions.
55 Maria Carmela L. Domocmat, RN, MSN 8/24/2011](https://image.slidesharecdn.com/musculoskeletaldisorderspart1cld-110823222718-phpapp02/85/Musculoskeletal-disorders-part-1-55-320.jpg)

![Surgical Intervention in Prosthetic Joint
Infection
In cases of prosthetic joint infection (PJI) that require surgery for cure,
successful treatment requires appropriate antibiotic therapy combined with
removal of the hardware. Despite appropriate antibiotic use, the success rate has
been only about 20% if the prosthesis is left in place. In recent years, evidence
has shown that debridement alone could yield a cure rate of 74.5% of patients
with a prosthetic joint infection and a C-reactive protein (CRP) level of 15
mg/dL or less who are treated with a fluoroquinolone.[26] For the time being, a
2-stage approach should be regarded as the most effective technique.
First, remove the prosthesis and follow with 6 weeks of antibiotic therapy.
Then, place the new joint, impregnating the methylmethacrylate cement with
an anti-infective agent (ie, gentamicin, tobramycin). Antibiotic diffusion into
the surrounding tissues is the goal. The success rate for this approach is
approximately 95% for both hip and knee joints.
An intermediate method is to exchange the new joint for the infected joint in a
1-stage surgical procedure with concomitant antibiotic therapy. This method,
with concurrent use of antibiotic cement, succeeds in 70-90% of cases.
57 Maria Carmela L. Domocmat, RN, MSN 8/24/2011](https://image.slidesharecdn.com/musculoskeletaldisorderspart1cld-110823222718-phpapp02/85/Musculoskeletal-disorders-part-1-57-320.jpg)




![Down syndrome
Down syndrome is by far the most common and best
known chromosomal disorder in humans and the most
common cause of intellectual disability.[3]
Mental retardation, dysmorphic facial features, and other
distinctive phenotypic traits characterize the syndrome
106 Maria Carmela L. Domocmat, RN, MSN 8/24/2011](https://image.slidesharecdn.com/musculoskeletaldisorderspart1cld-110823222718-phpapp02/85/Musculoskeletal-disorders-part-1-106-320.jpg)
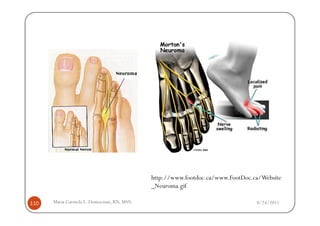
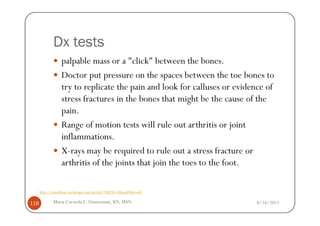
![Causes
Various factors have been implicated in the precipitation of Morton's neuroma.
Morton's neuroma is known to develop as a result of chronic nerve stress and
irritation, particularly with excessive toe dorsiflexion.
Poorly fitting and constricting shoes (ie, small toe box) or shoes with heel lifts
often contribute to Morton's neuroma. Women who wear high-heeled shoes for
a number of years or men who are required to wear constrictive shoe gear are
at risk.
A biomechanical theory of causation involves the mechanics of the foot and
ankle. For instance, individuals with tight gastrocnemius-soleus muscles or who
excessively pronate the foot may compensate by dorsiflexion of the metatarsals
subsequently irritating of the interdigital nerve.
Certain activities carry increased risk of excessive toe dorsiflexion, such as
prolonged walking, running, squatting, and demi-pointe position in ballet.[4]
http://emedicine.medscape.com/article/308284-clinical#showall
114 Maria Carmela L. Domocmat, RN, MSN 8/24/2011](https://image.slidesharecdn.com/musculoskeletaldisorderspart1cld-110823222718-phpapp02/85/Musculoskeletal-disorders-part-1-114-320.jpg)







![Causes
Dystonic reactions cause muscles to spasm, and if left
untreated can damage muscle
Cholesterol lowering medications [for example, statins
prescribed to treat high cholesterol (particularly when
combined with other cholesterol lowering medications such
as fibrates)
Antidepressant medications
[for example selective serotonin reuptake inhibitors (SSRIs)
antidepressants may cause a serotonin syndrome characterized
by agitation, fever, and muscle spasm]
http://www.emedicinehealth.com/rhabdomyolysis/page3_em.htm
222 Maria Carmela L. Domocmat, RN, MSN 8/24/2011](https://image.slidesharecdn.com/musculoskeletaldisorderspart1cld-110823222718-phpapp02/85/Musculoskeletal-disorders-part-1-222-320.jpg)
![Causes
Some anesthetics can cause malignant hyperthermia syndrome
with high fever and muscle rigidity
A variety of drugs of abuse [for example, cocaine, heroin,
phencyclidine (PCP), and amphetamines]
Hyperthermia and hypothermia (high and low body temperature,
respectively)
Complications from a variety of infections caused by bacteria,
viruses, and fungi
Association with other diseases such as sickle cell
disease, polymyositis, and dermatomyositis
Complications from the venom from snake bites and black widow
spider bites
http://www.emedicinehealth.com/rhabdomyolysis/page3_em.htm
223 Maria Carmela L. Domocmat, RN, MSN 8/24/2011](https://image.slidesharecdn.com/musculoskeletaldisorderspart1cld-110823222718-phpapp02/85/Musculoskeletal-disorders-part-1-223-320.jpg)