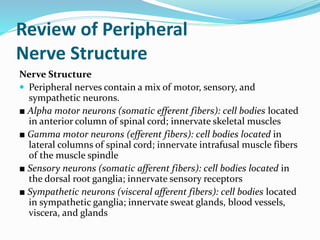
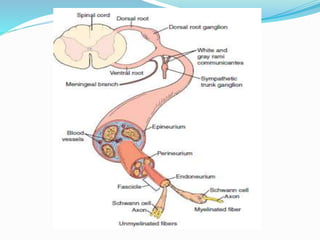
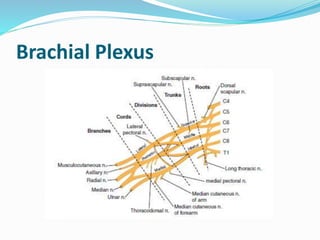
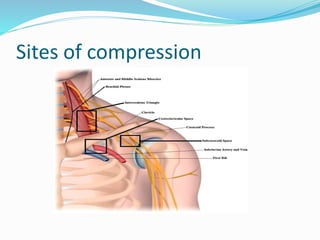
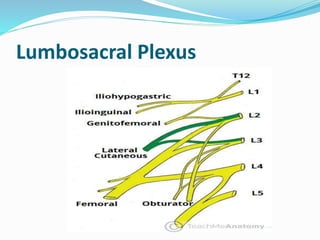
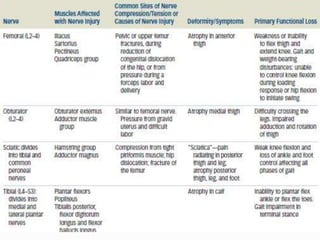
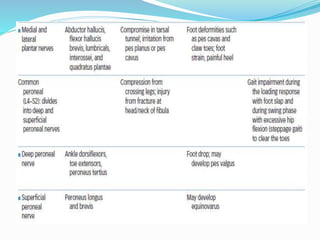
This document provides an overview of peripheral nerve structure and common sites of injury. It discusses the different types of neurons that make up peripheral nerves, including motor, sensory and sympathetic neurons. Common sites where peripheral nerves can be injured include the intervertebral foramina, brachial plexus and lumbosacral plexus. Mechanisms of nerve injury include compression, laceration, stretch and radiation. The document also outlines guidelines for managing nerve injuries in the acute, recovery and chronic phases.