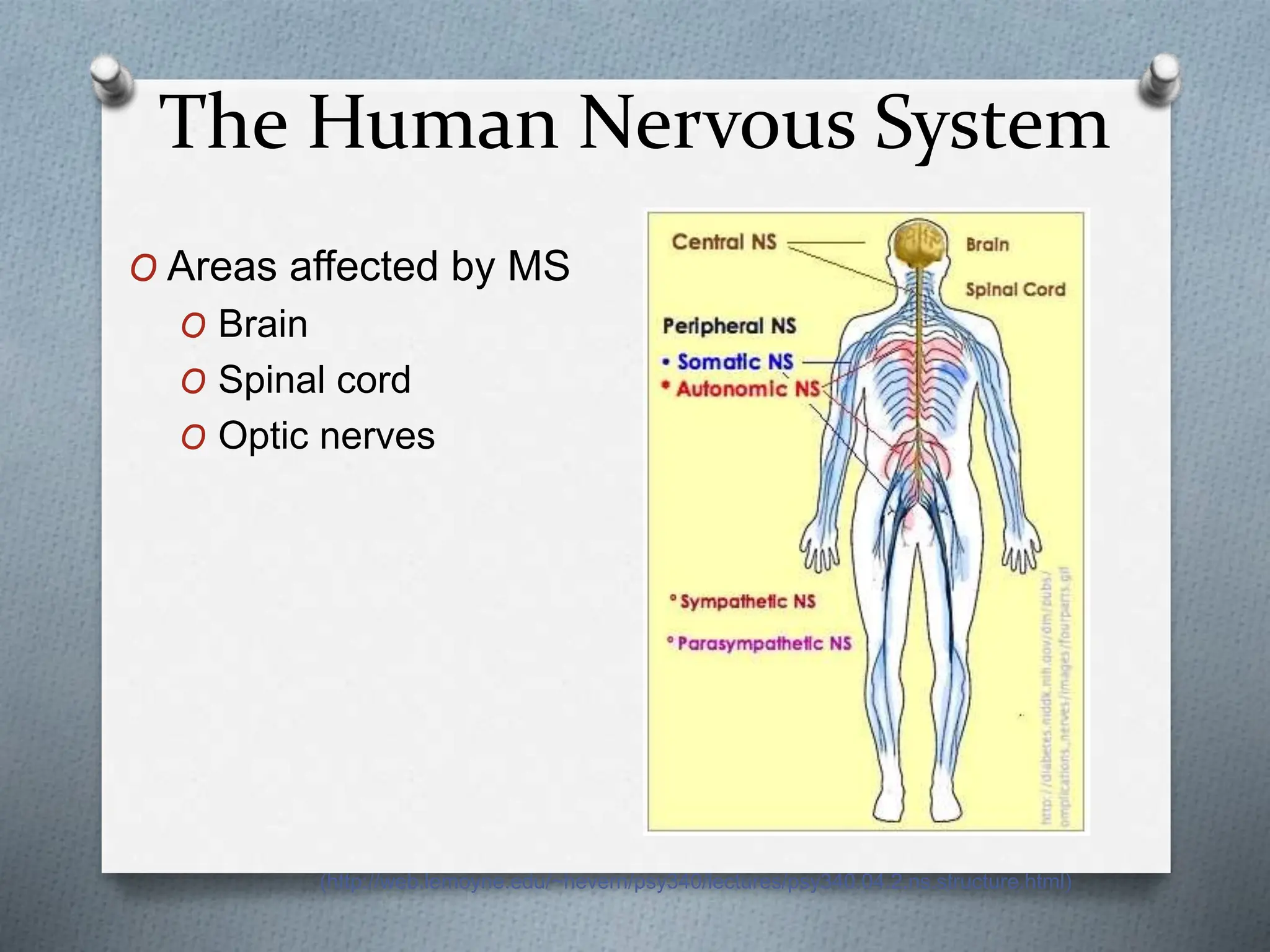
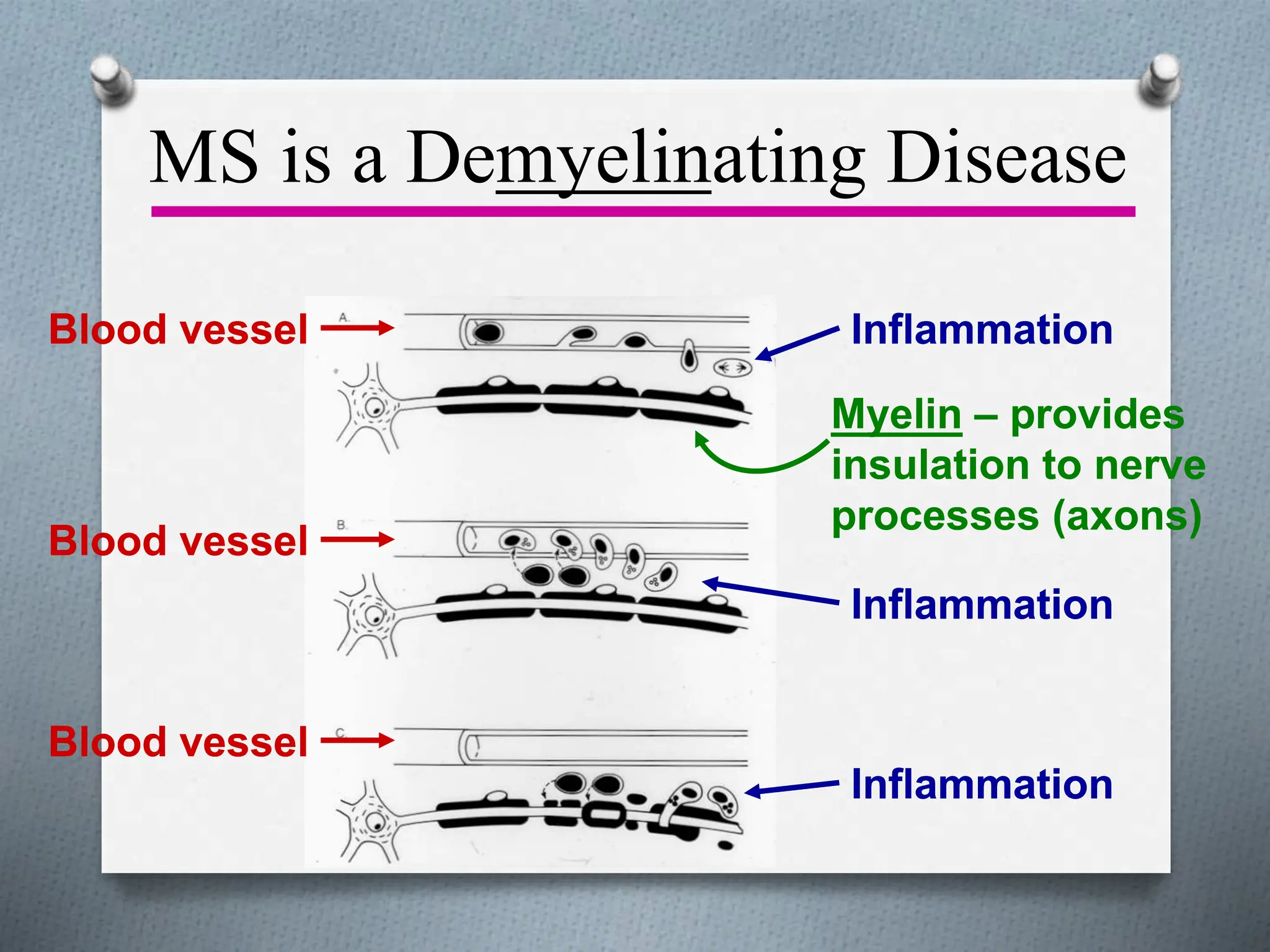
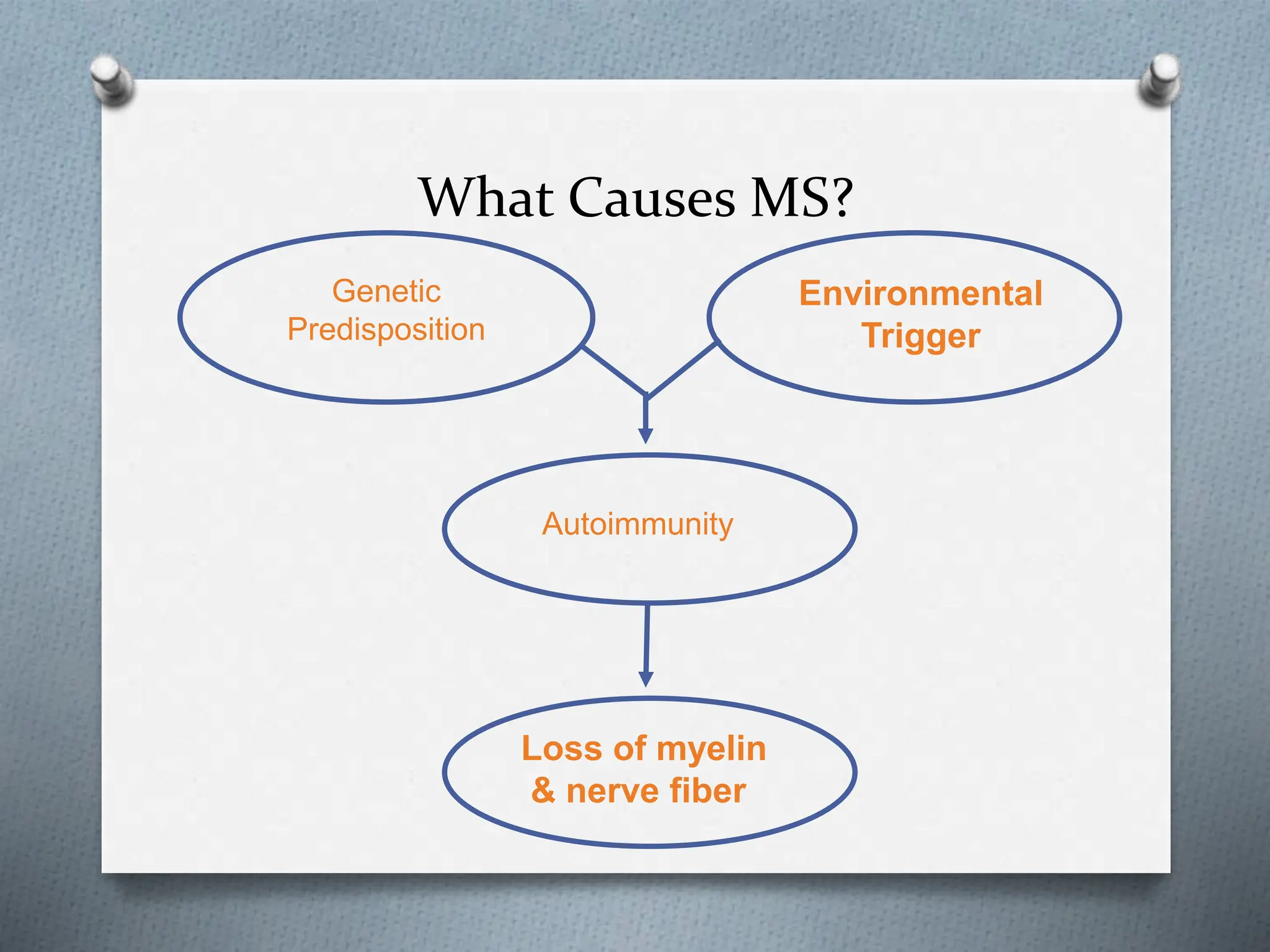
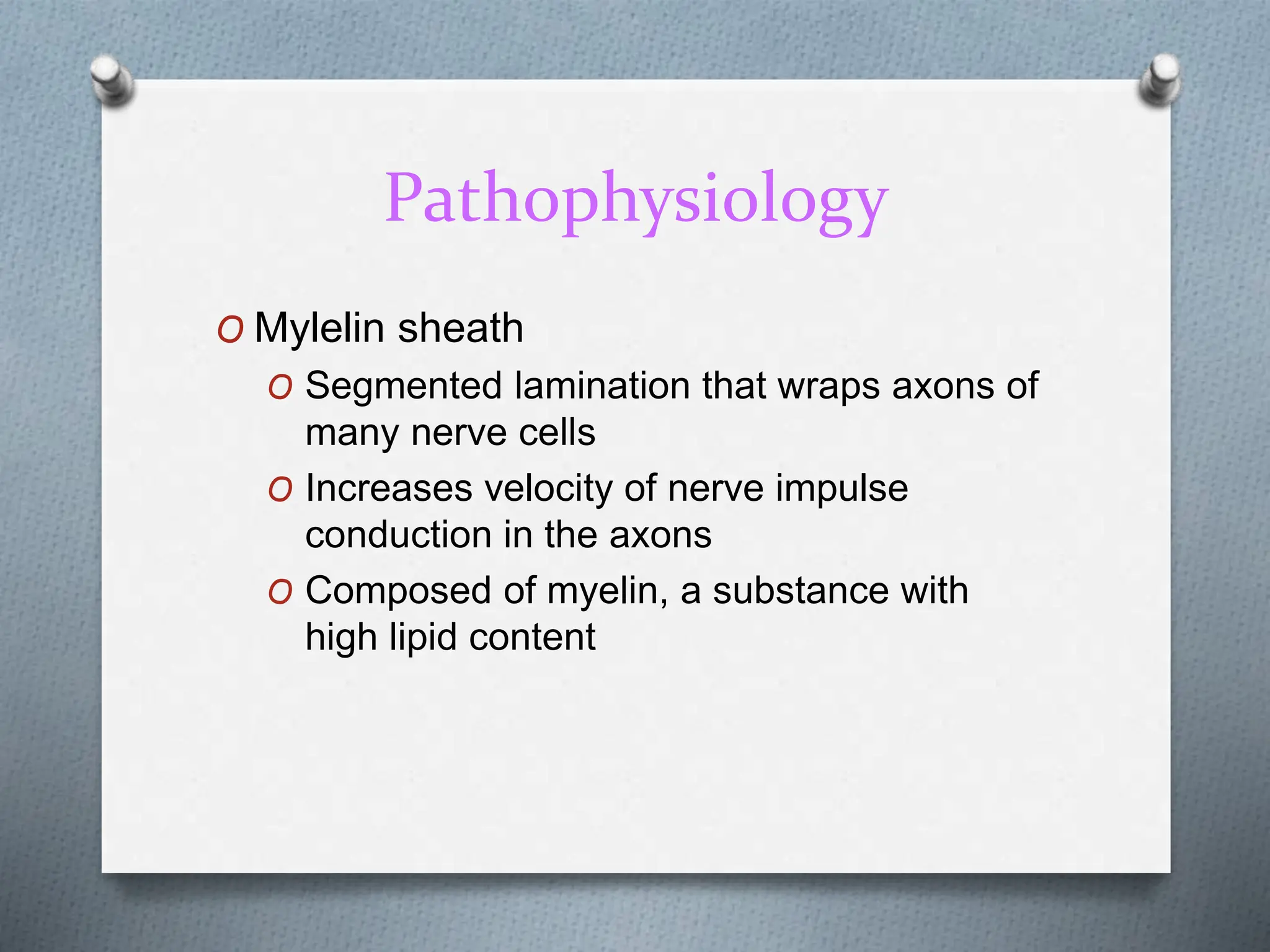
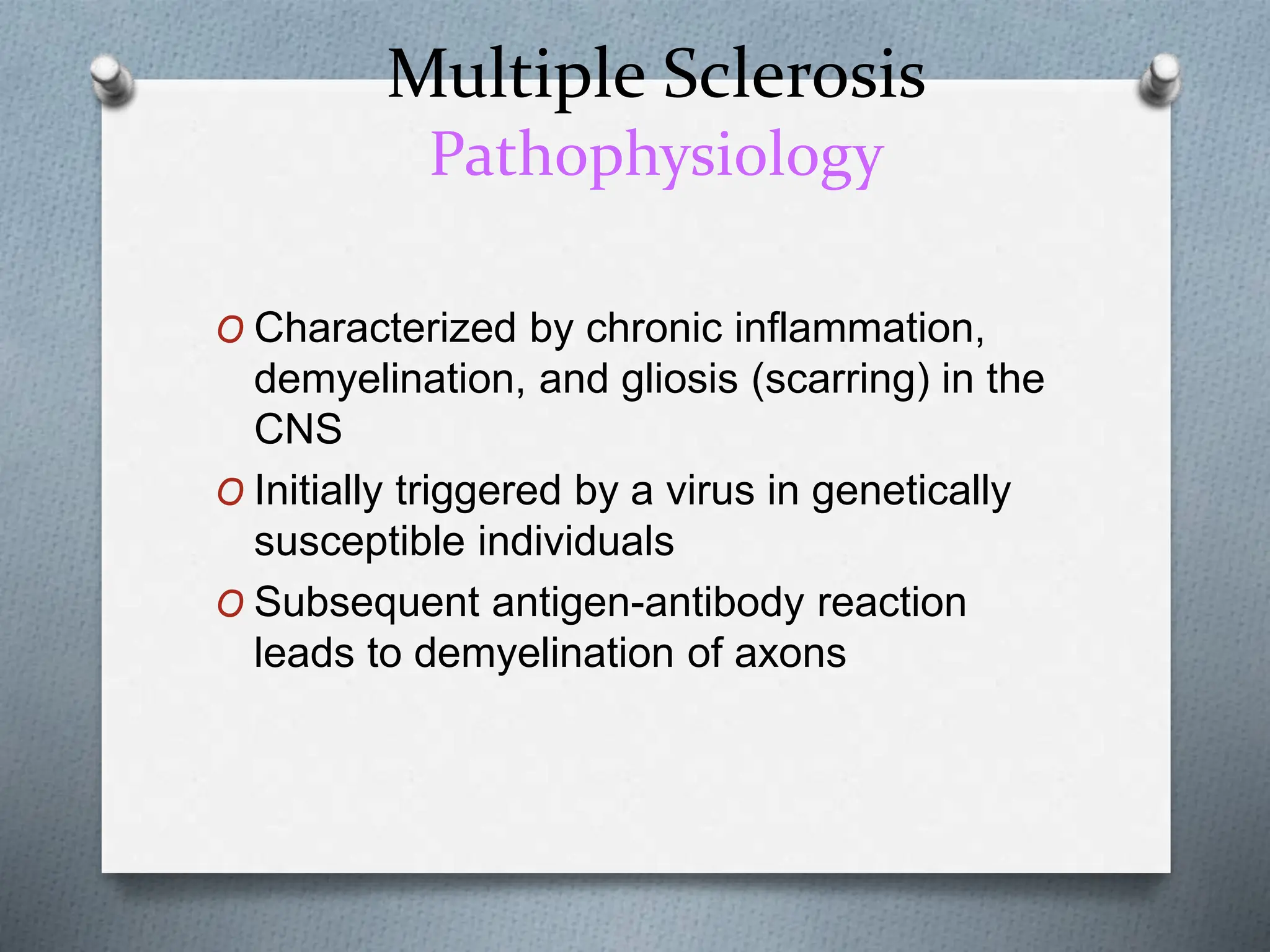
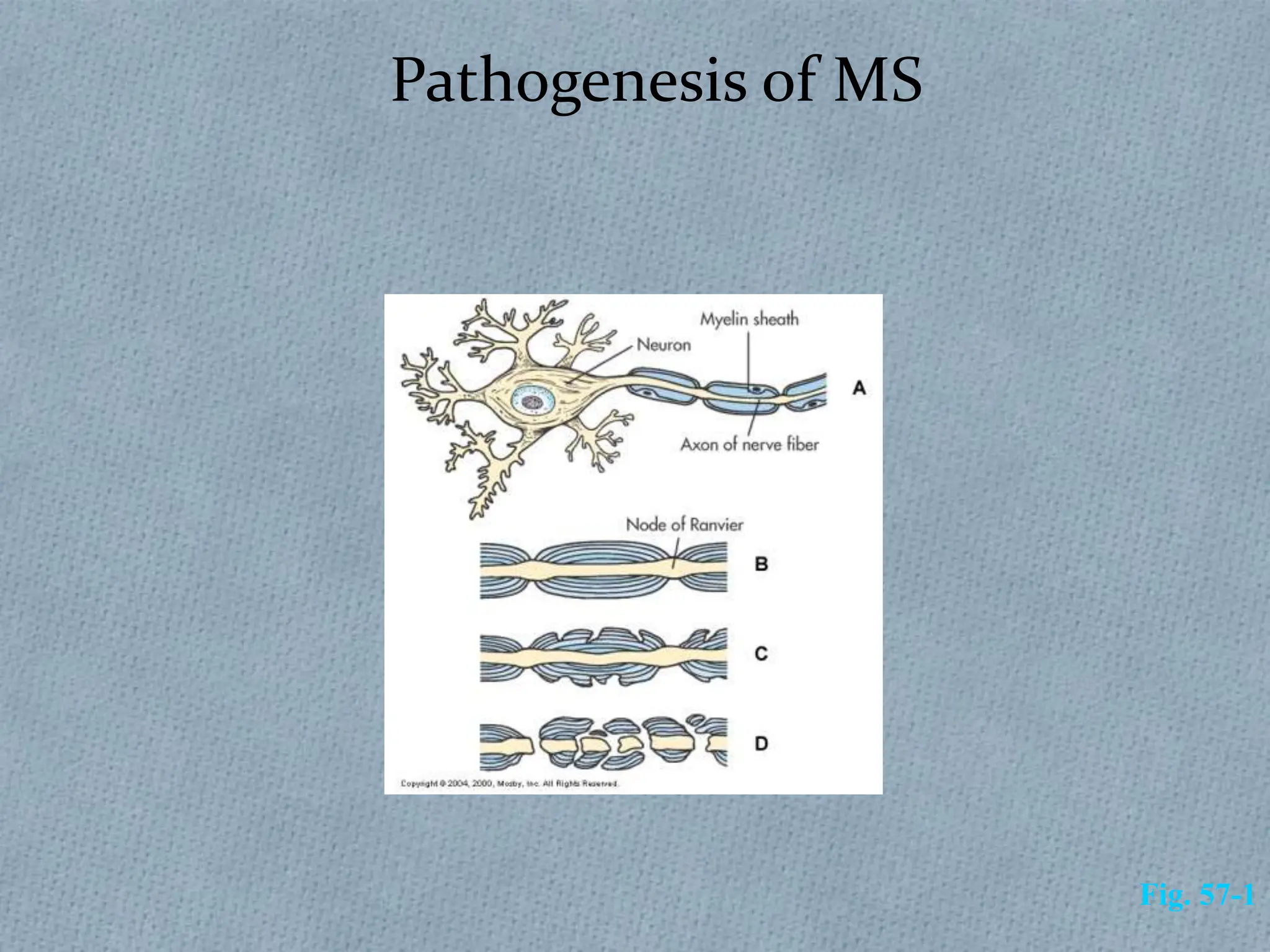
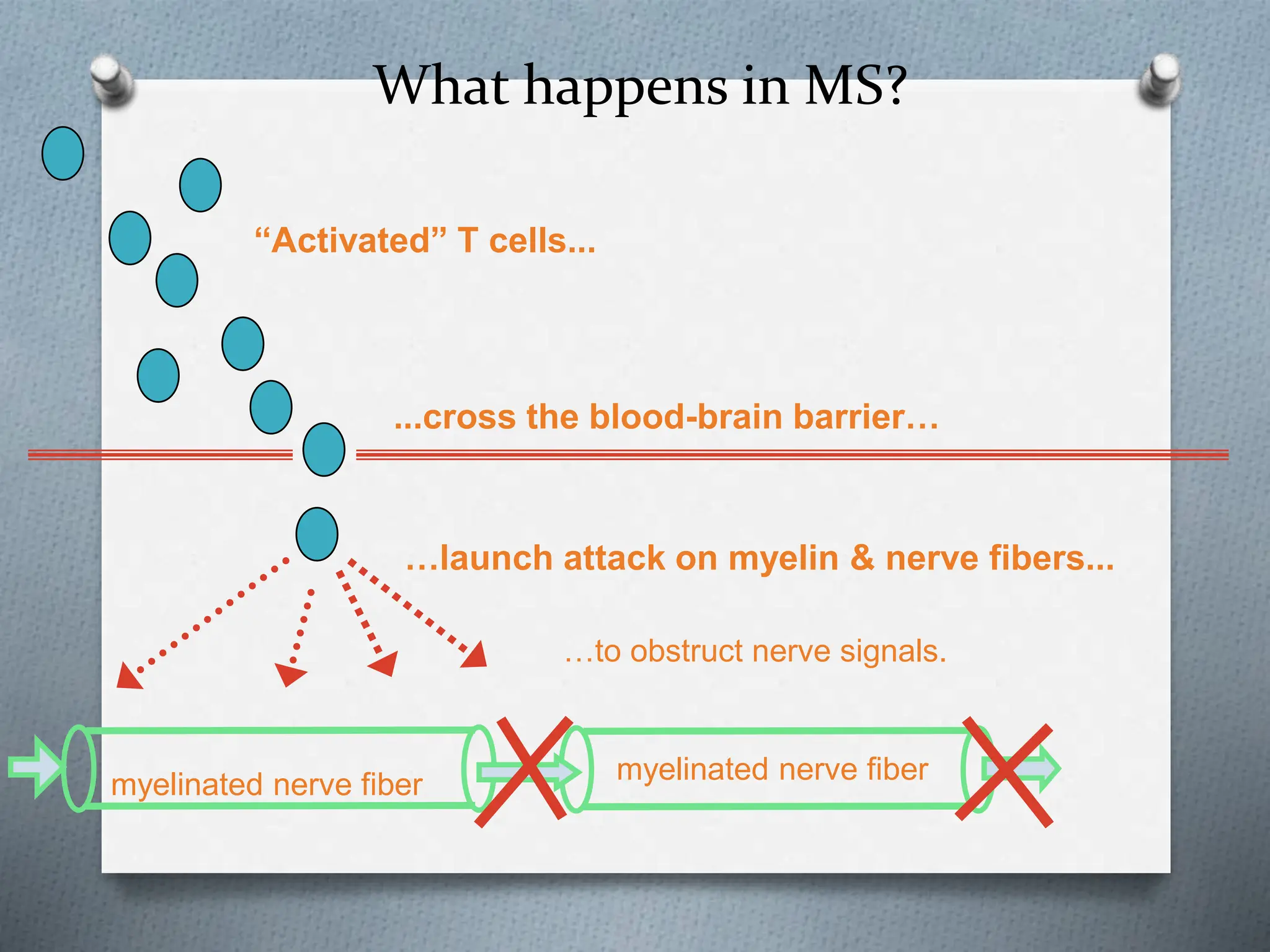
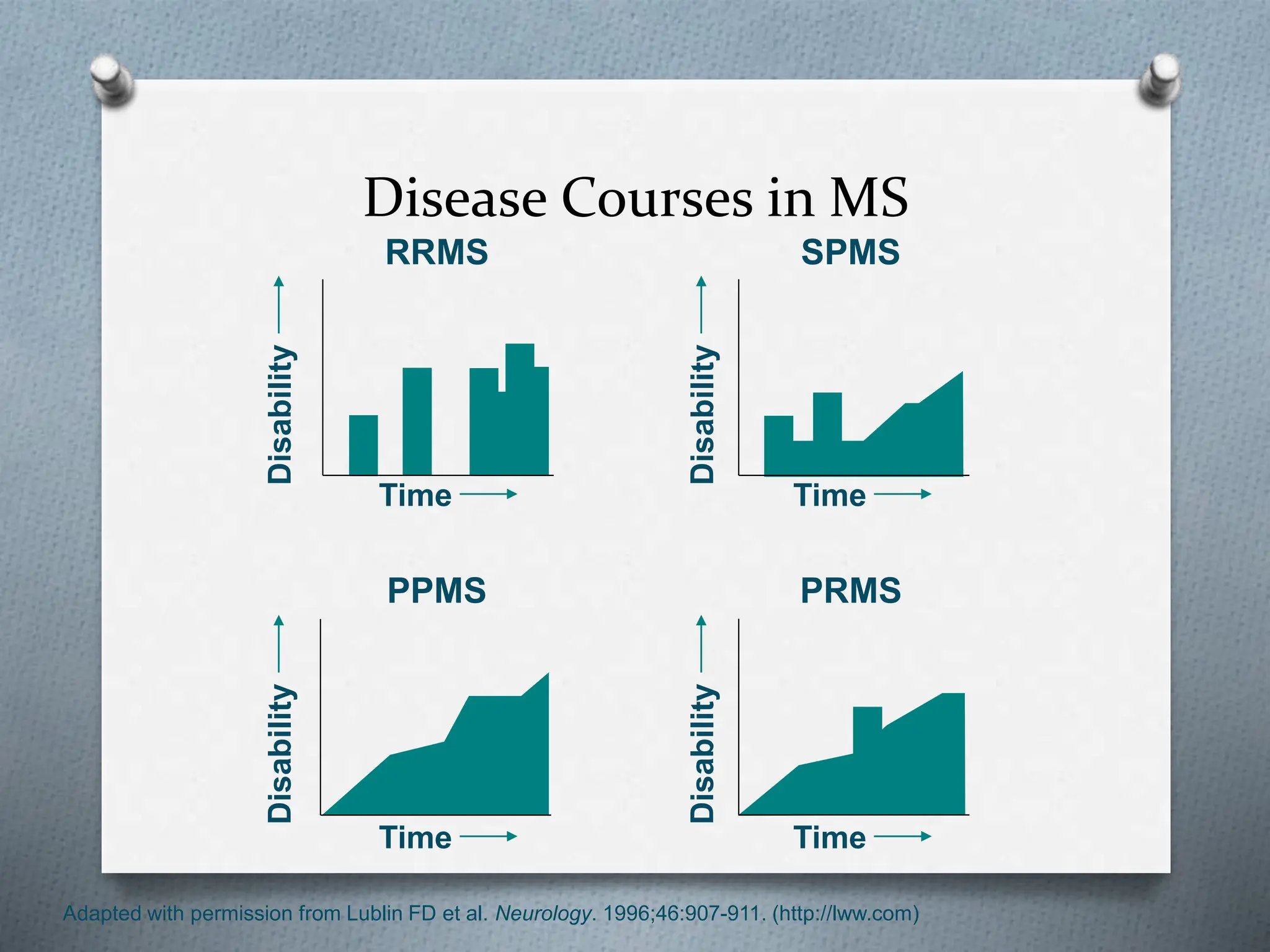
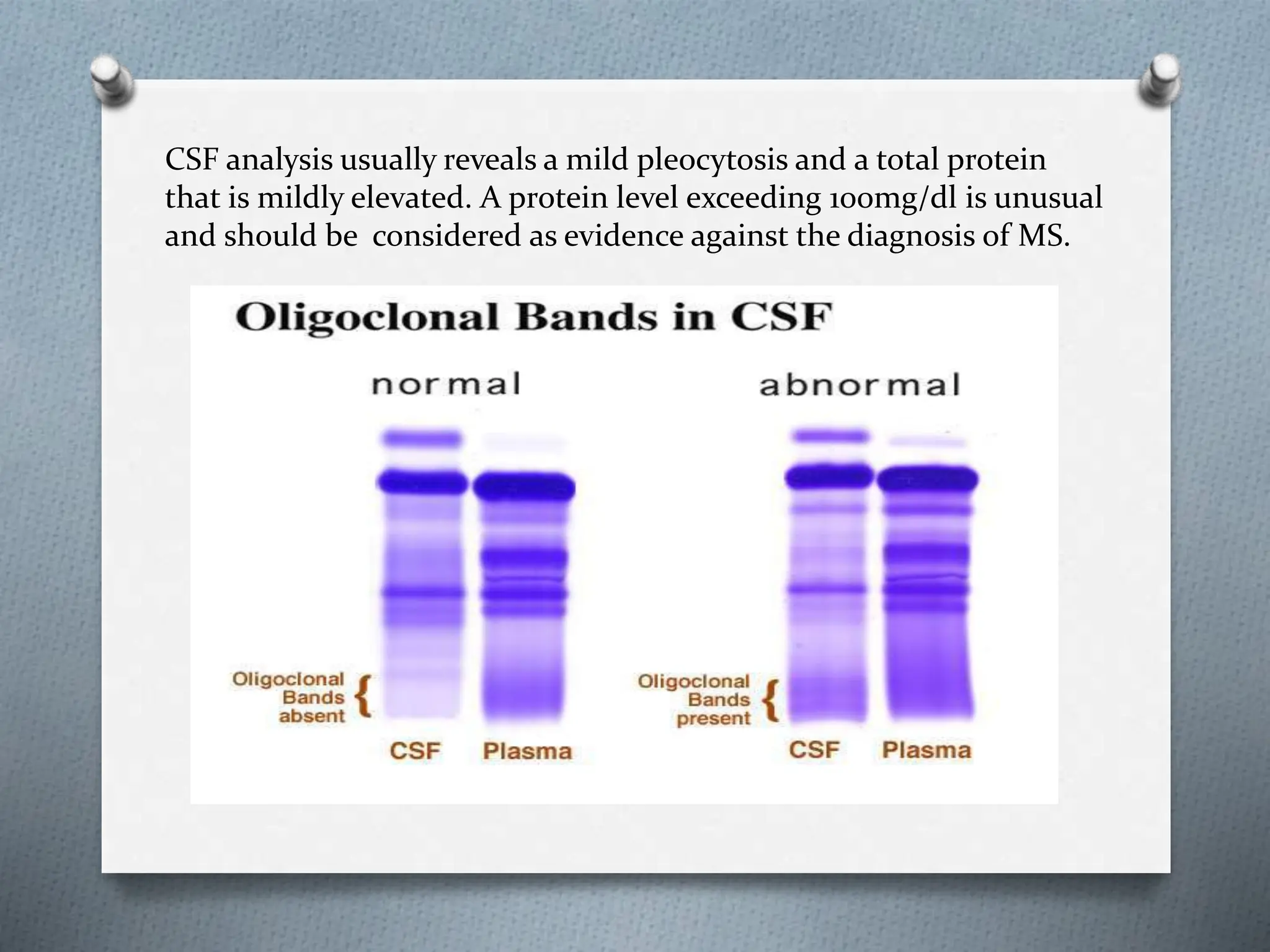
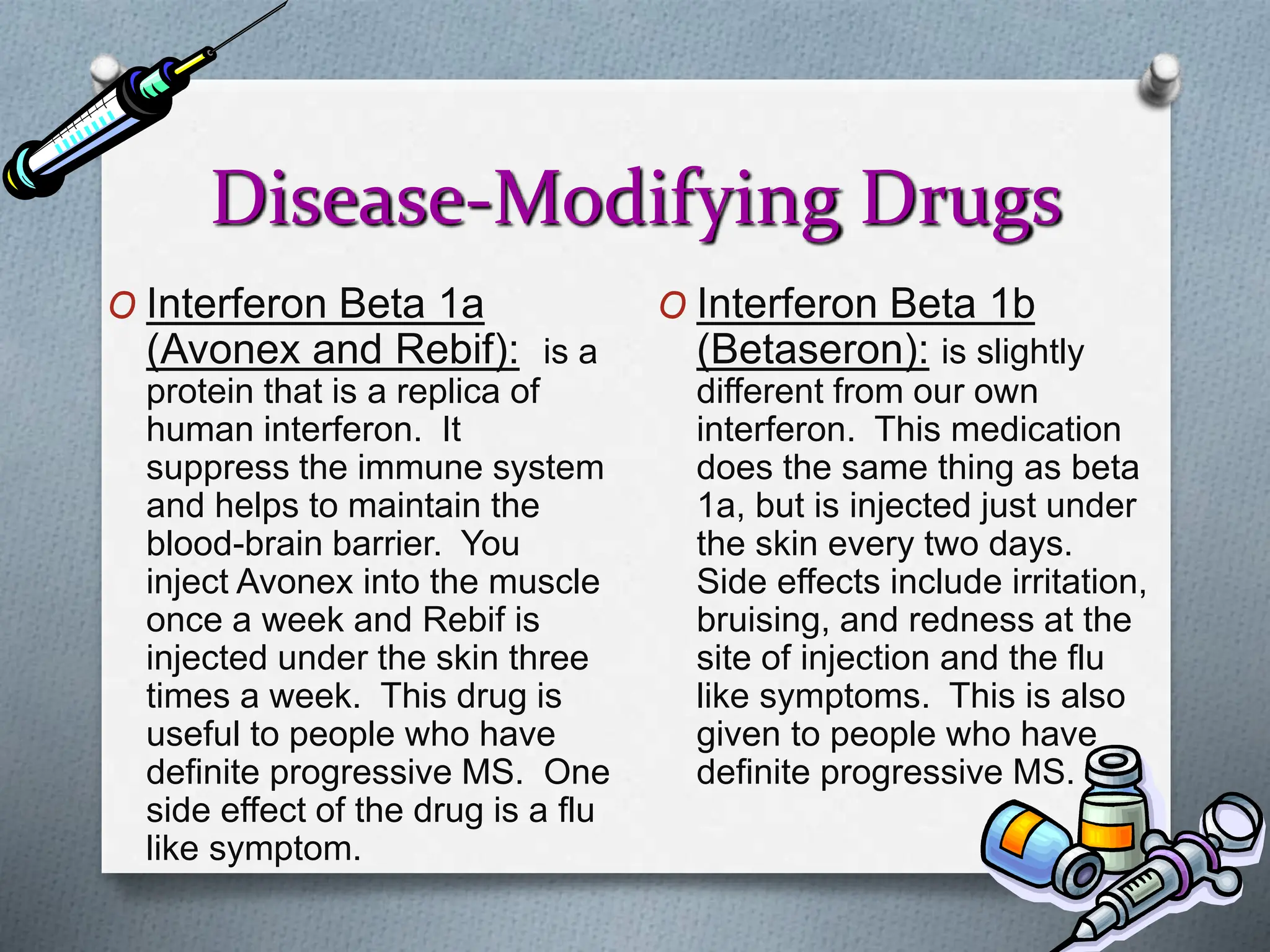
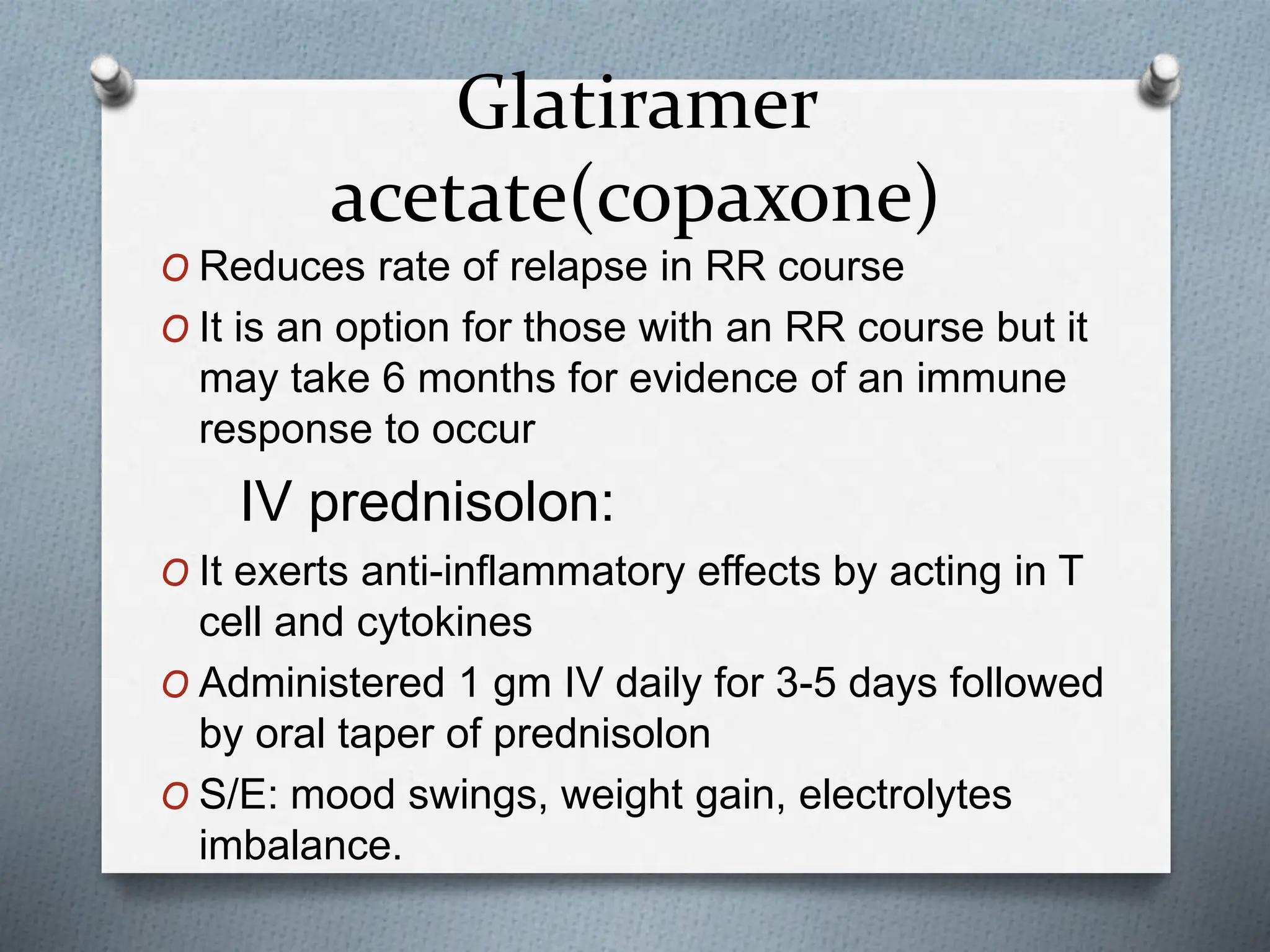
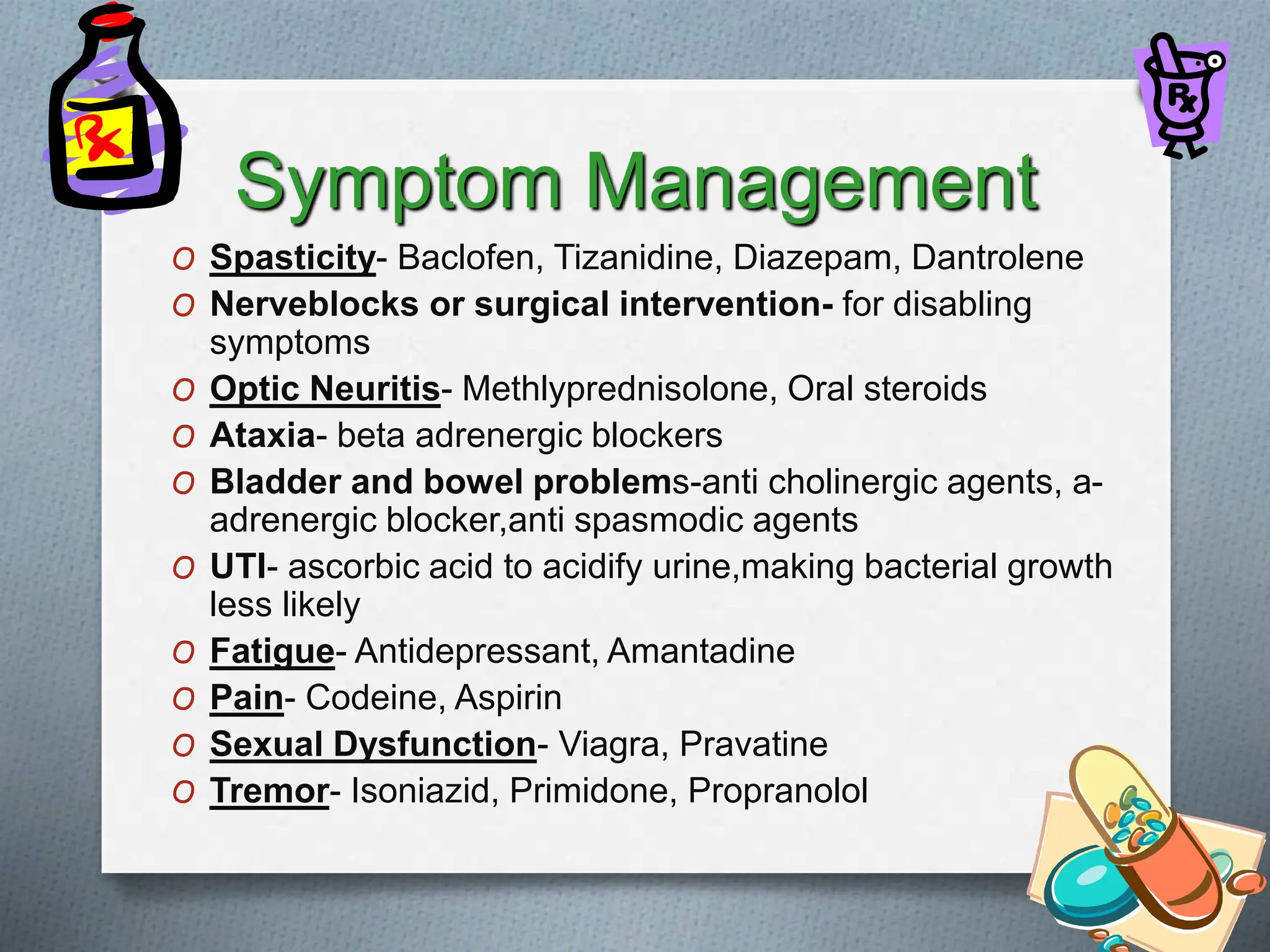
Multiple sclerosis (MS) is an autoimmune disease where the body's immune system attacks the protective myelin sheath that surrounds the nerves in the central nervous system. It is a lifelong disease with no known cure. Symptoms vary between individuals but can include motor problems, sensory issues, vision problems, and cognitive changes. The disease course is usually relapsing-remitting but can also be progressive. Diagnosis is based on symptoms, neurological exam findings, and MRI evidence of lesions in the brain and spinal cord. Treatment focuses on managing symptoms and reducing relapses and progression using medications like interferons and corticosteroids.