This document provides an overview of several neurologic disorders, including:
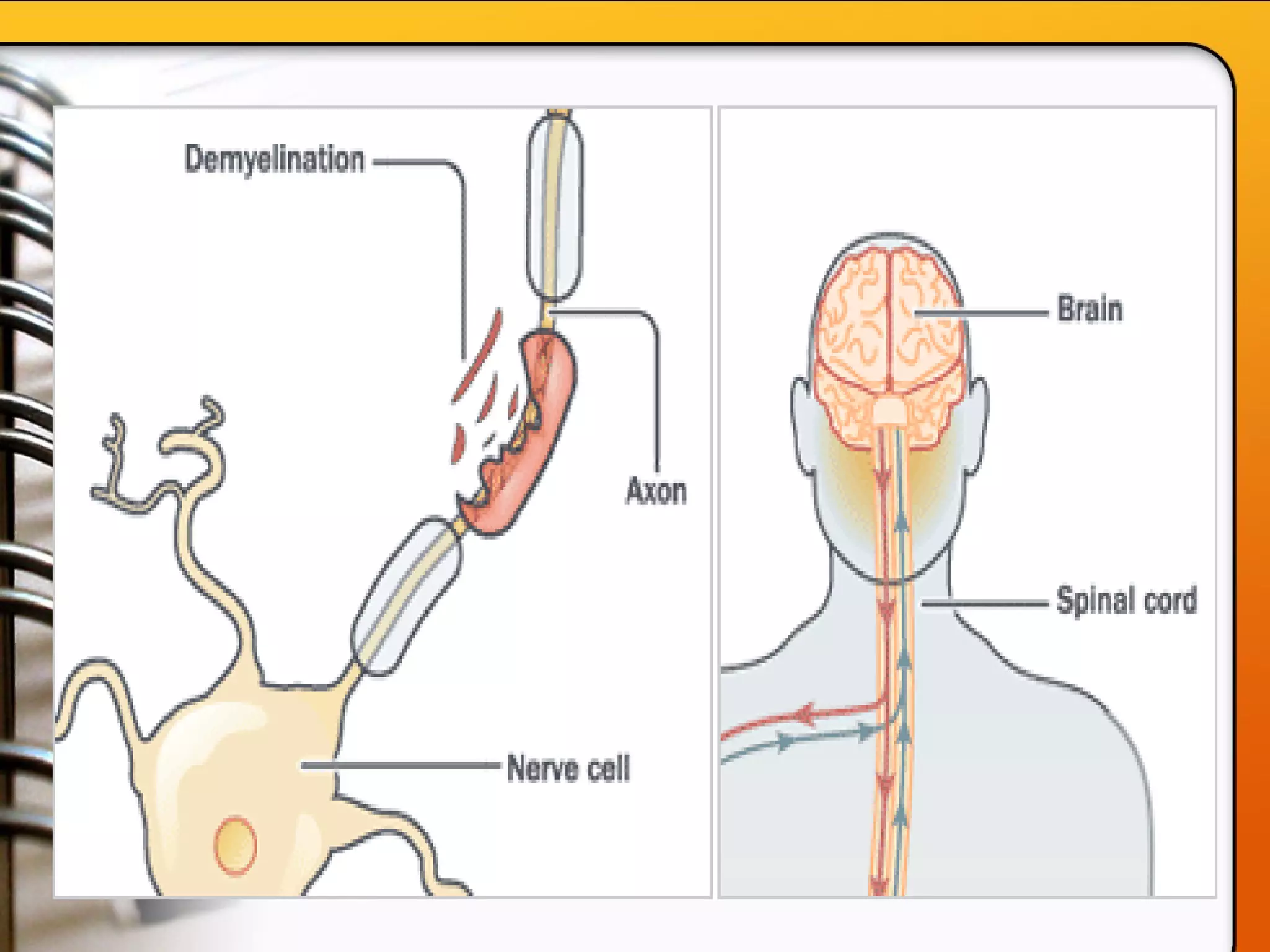
- Multiple sclerosis, which causes fatigue, vision issues, weakness and more. Treatment focuses on retaining function and limiting disability.
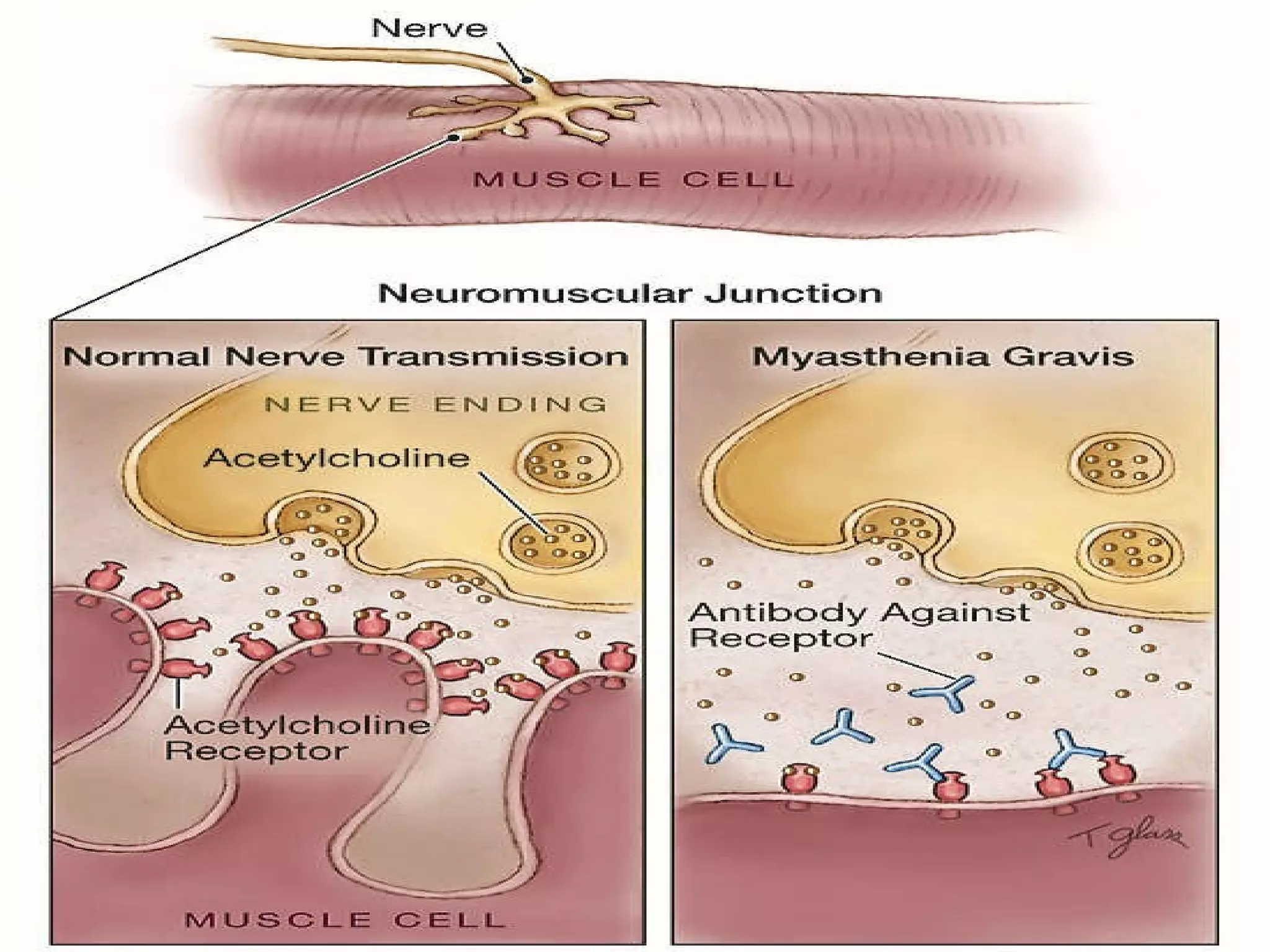
- Myasthenia gravis, an autoimmune disorder causing severe muscle weakness. Medications aim to improve symptoms.
- Guillain-Barré syndrome, an acute inflammatory disorder causing ascending paralysis. Supportive care and monitoring of respiratory function are priorities.
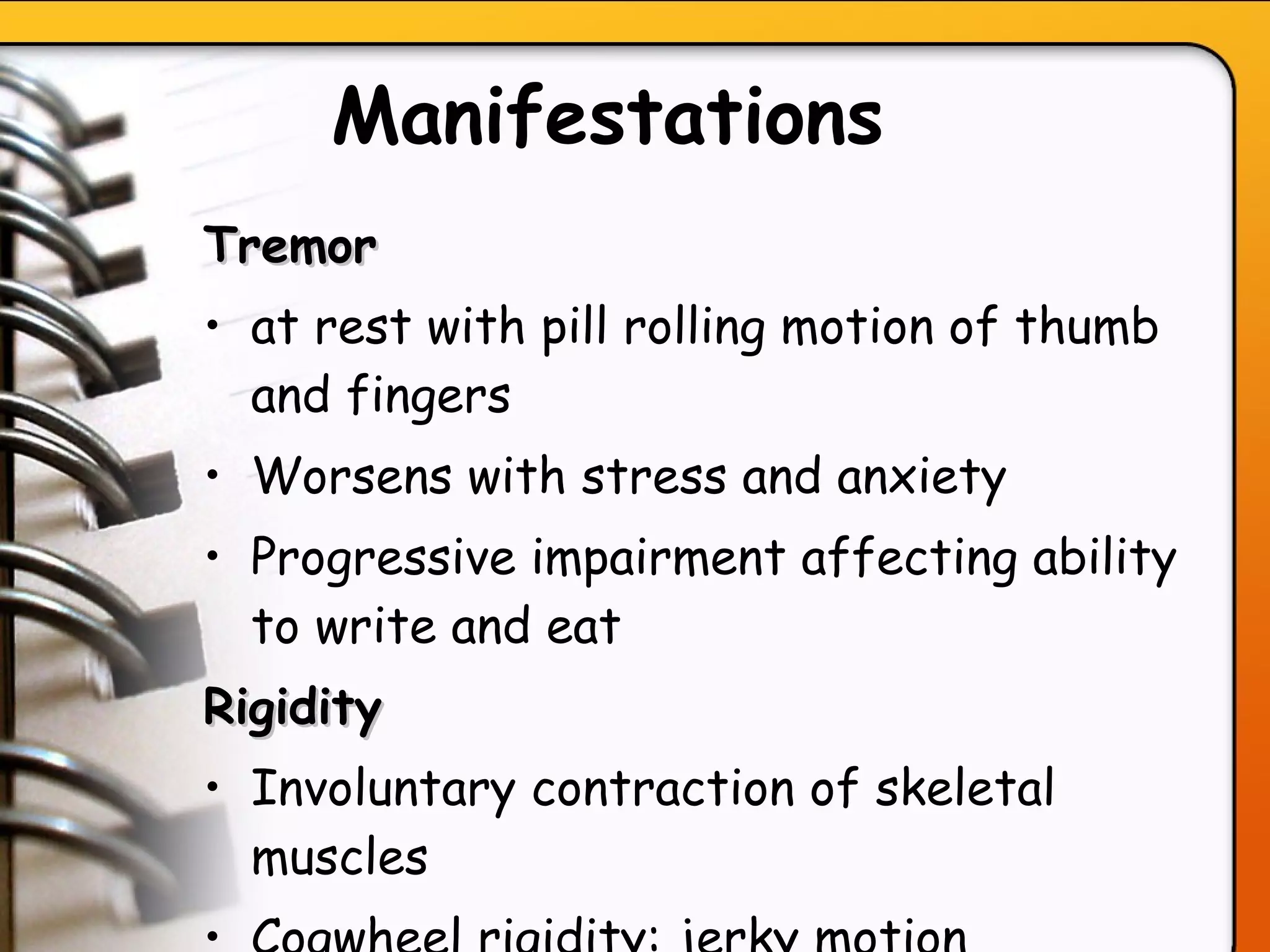
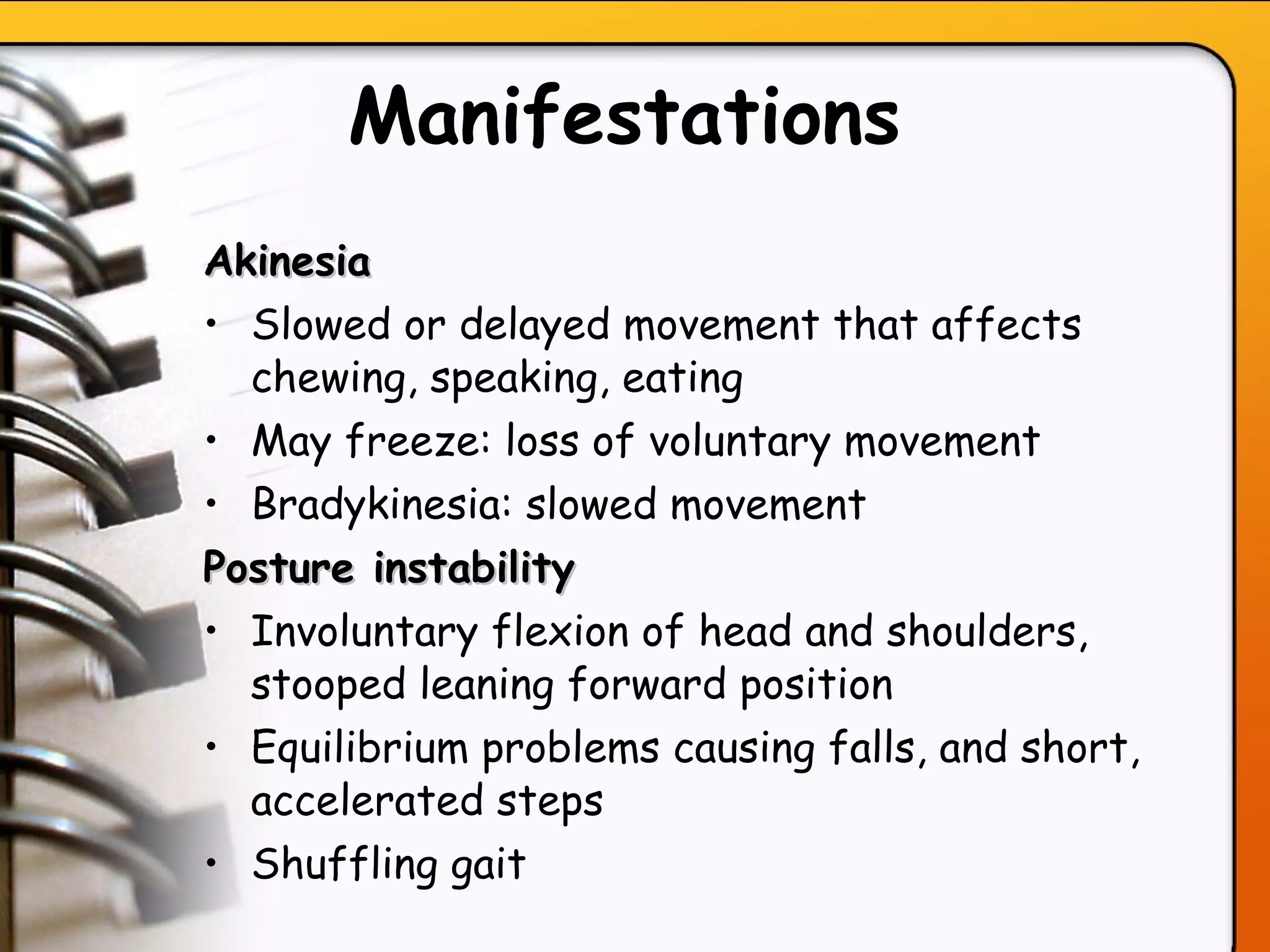
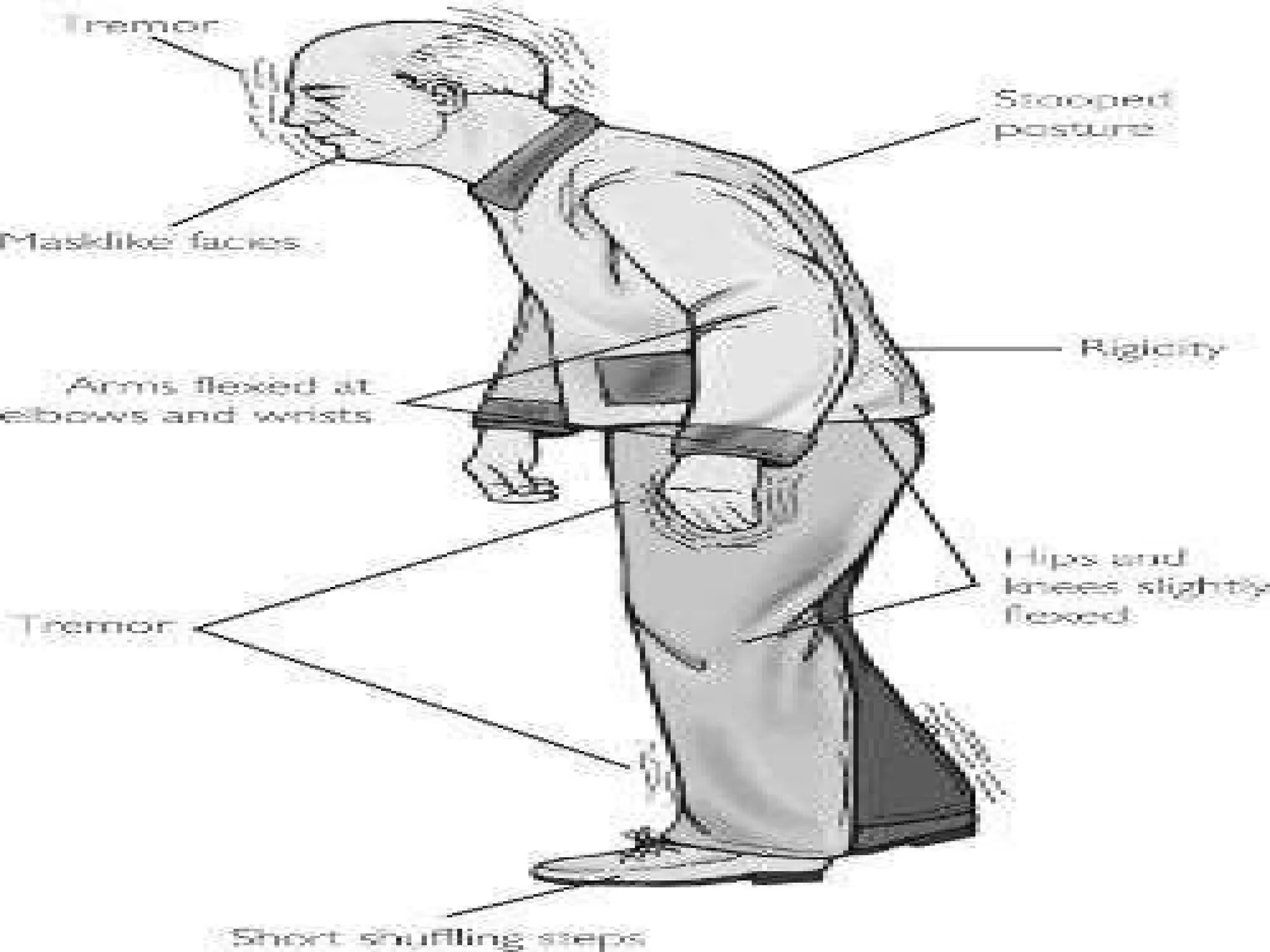
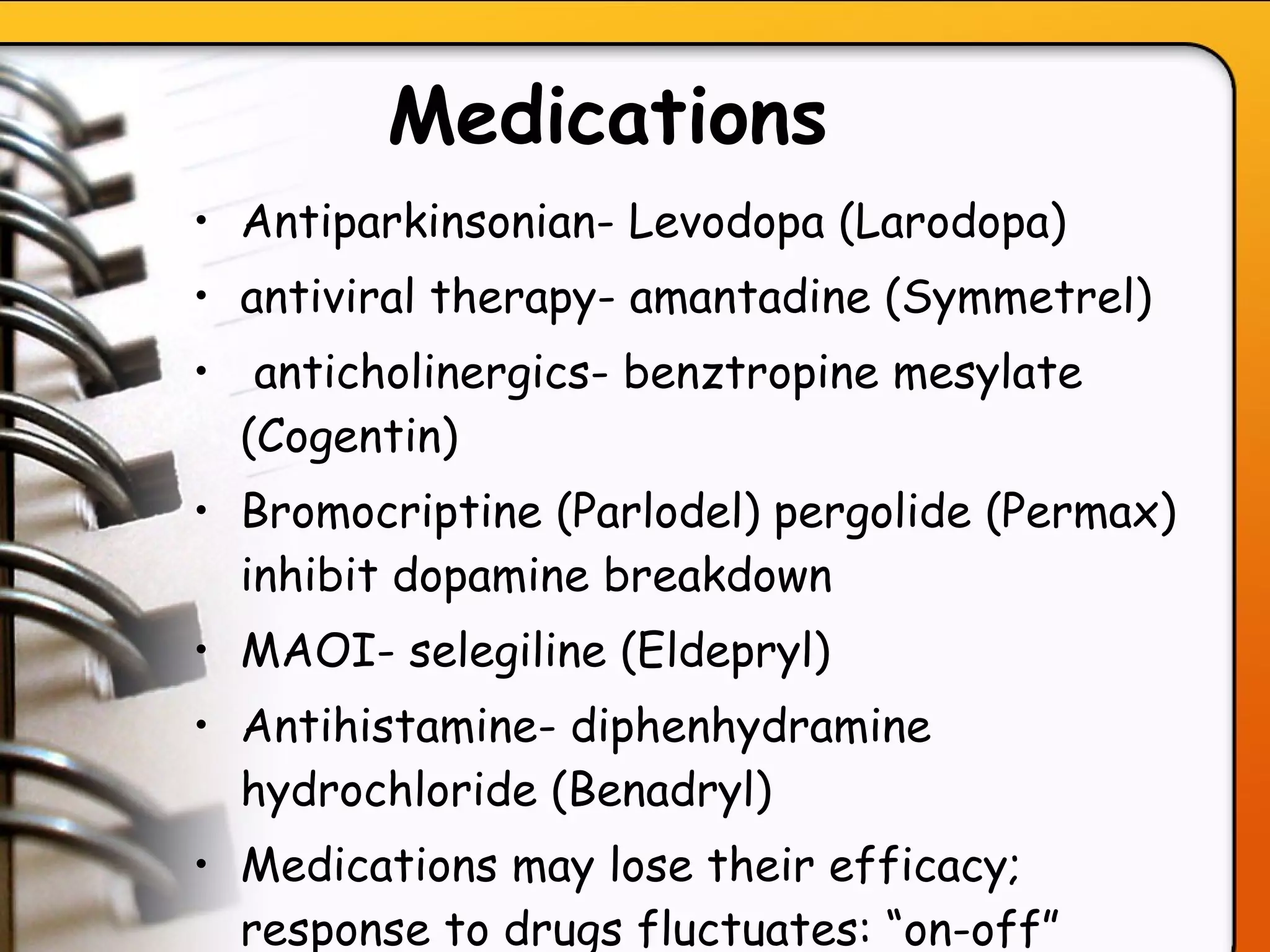
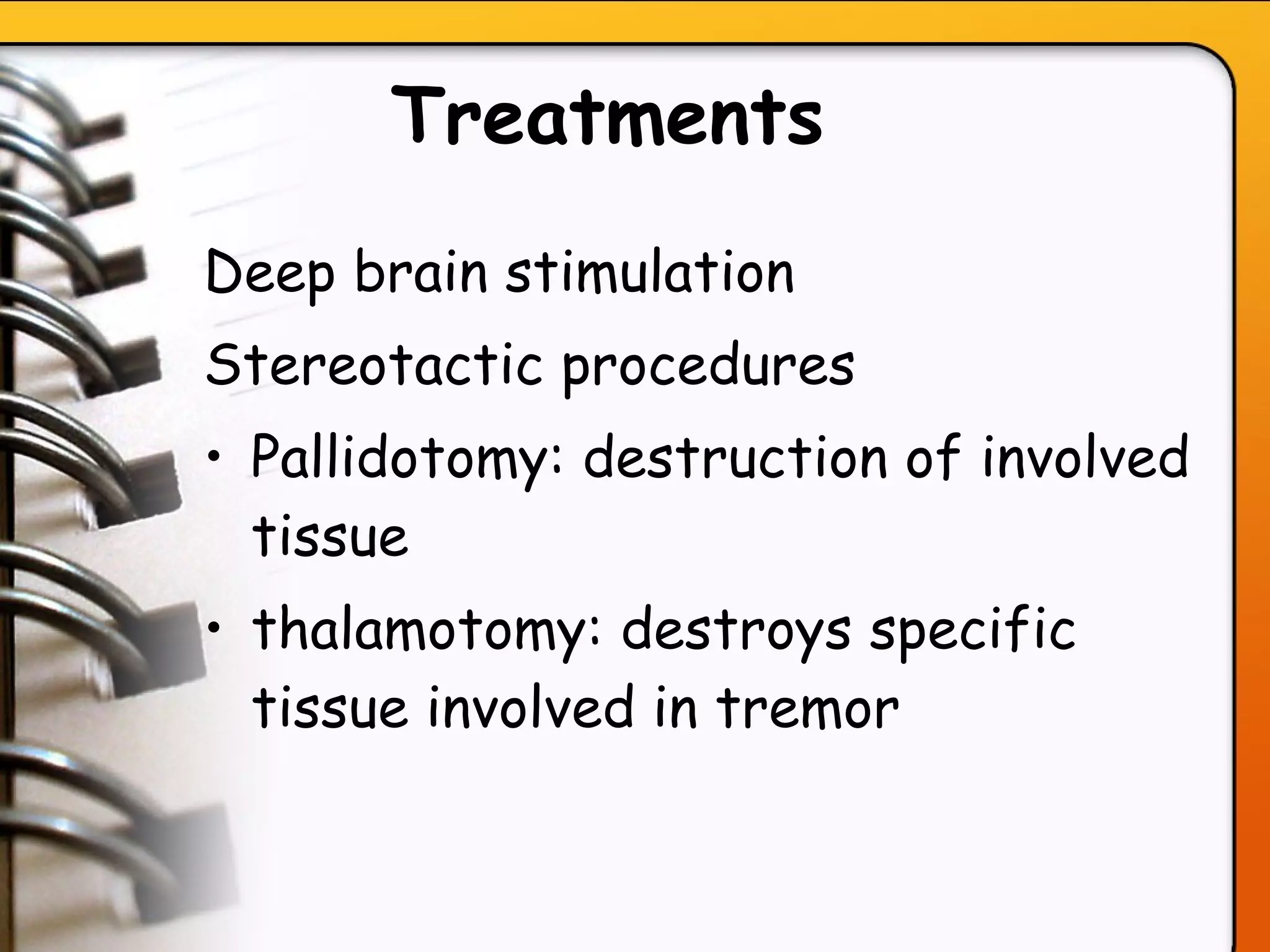
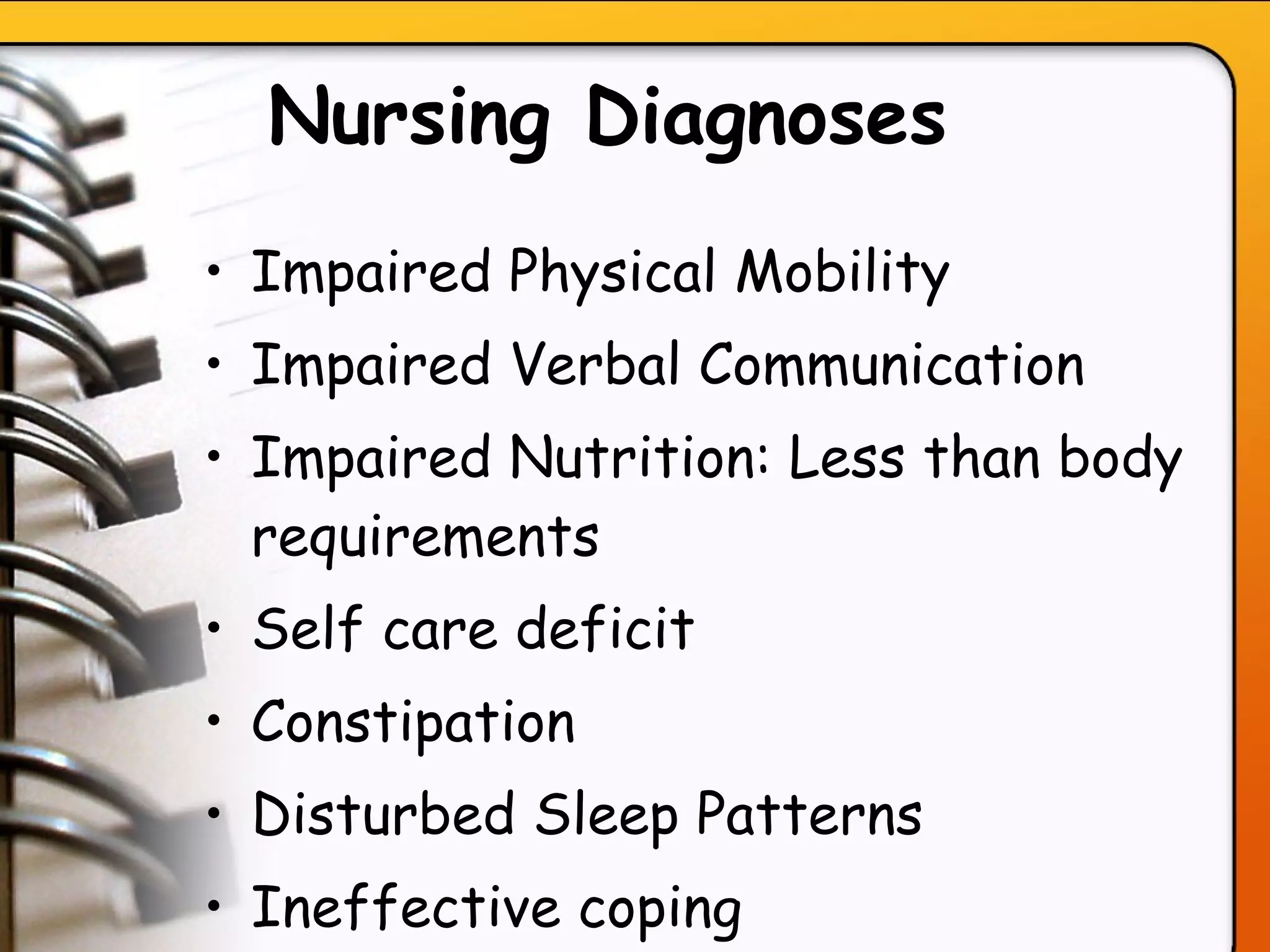
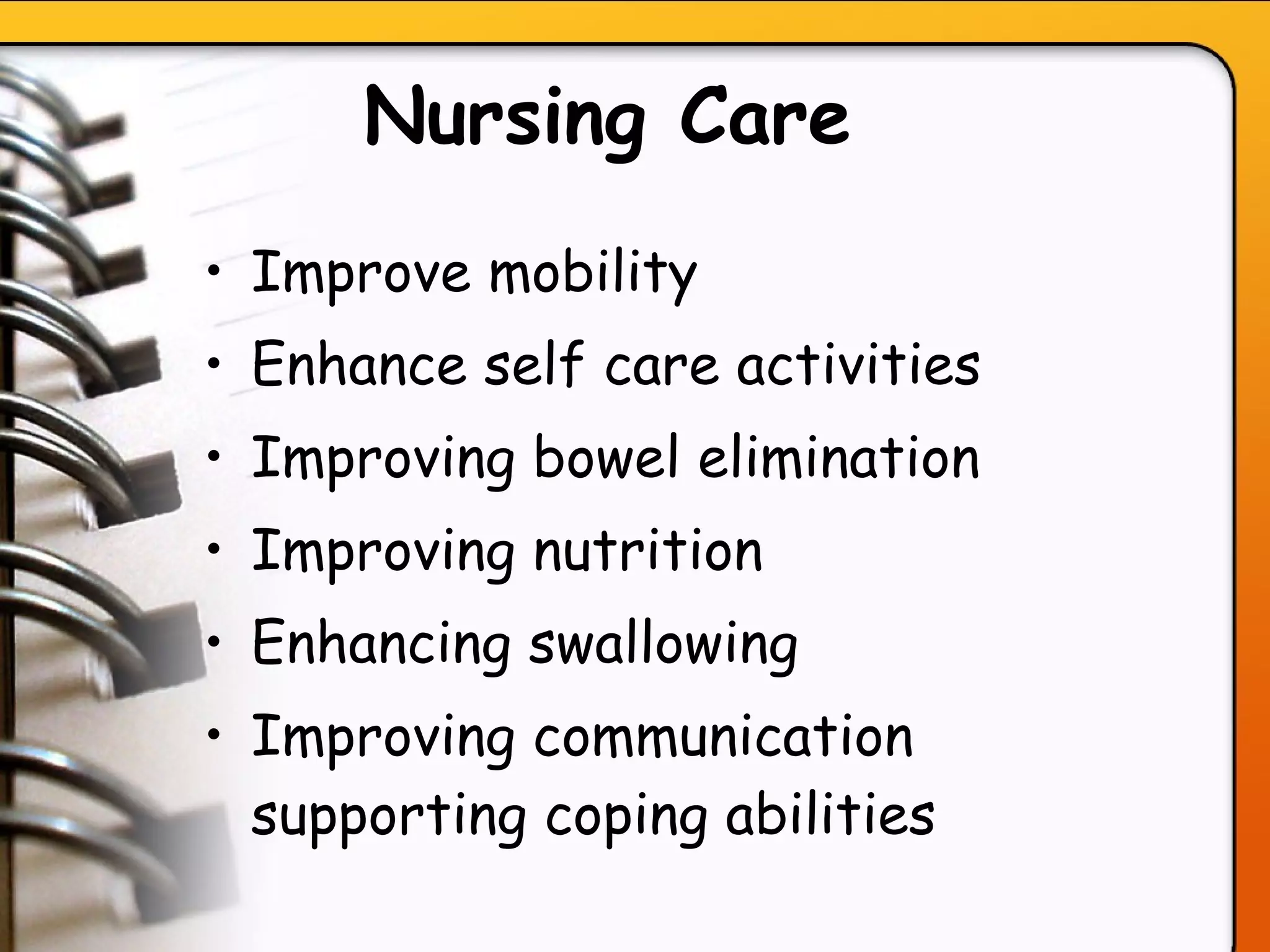
- Parkinson's disease, characterized by tremors and rigidity. Medications may provide relief but symptoms gradually worsen over time.
- Huntington's disease, an inherited disorder causing chorea and dementia. No cure exists, and