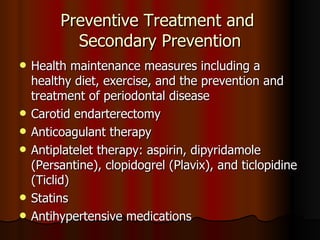
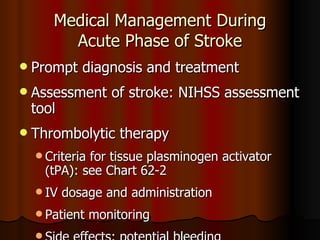
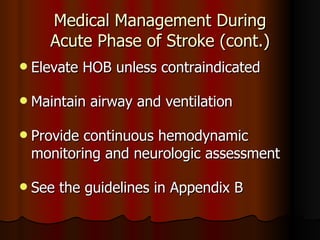
1) The document discusses the management of patients with cerebrovascular disorders such as stroke, which is a leading cause of death and long-term disability in the US.
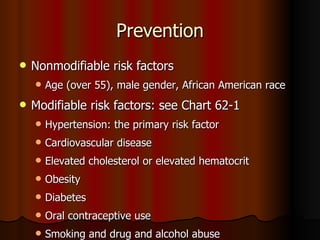
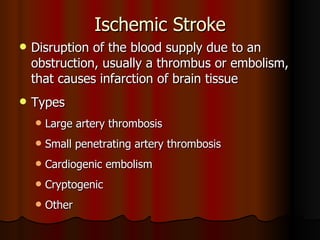
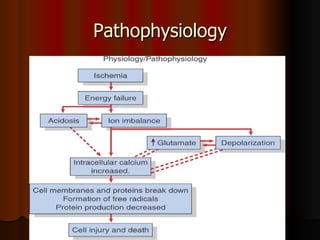
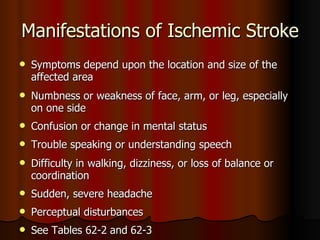
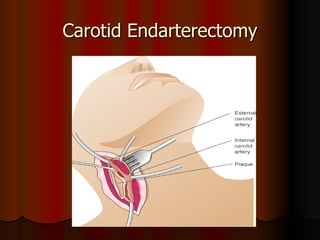
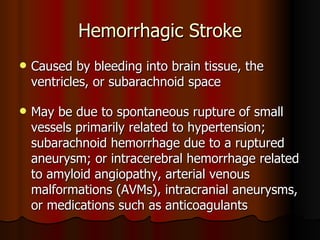
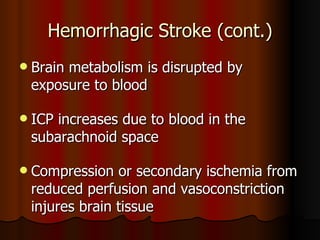
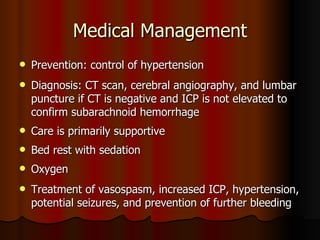
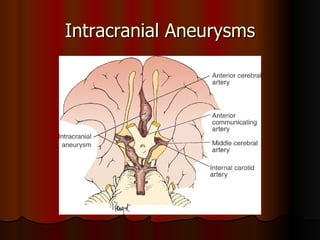
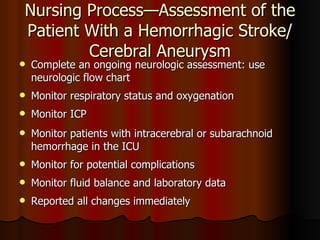
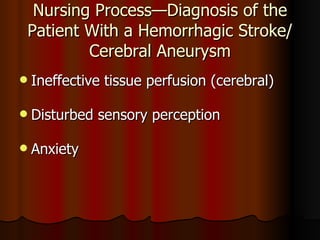
2) It covers the prevention, types, pathophysiology, manifestations, and medical management of ischemic and hemorrhagic strokes.
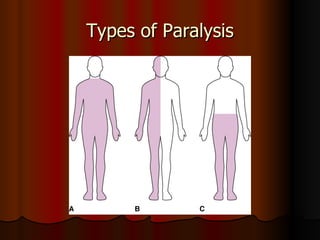
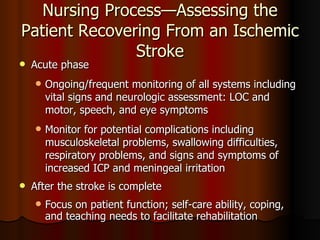
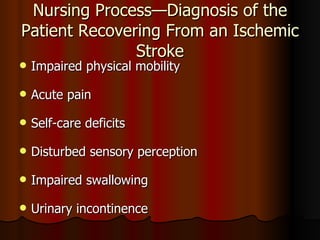
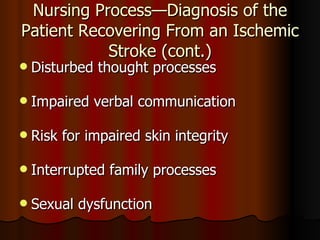
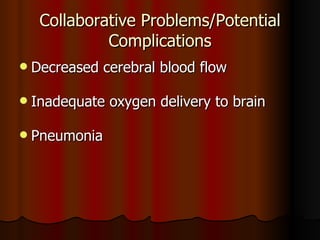
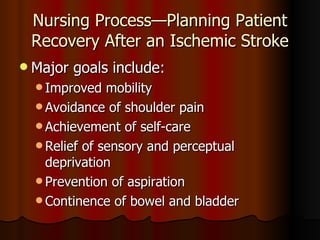
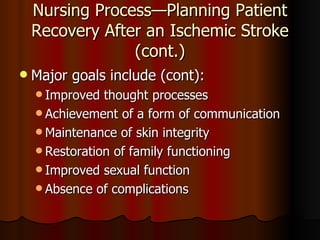
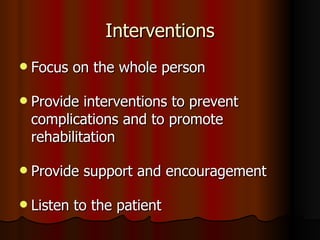
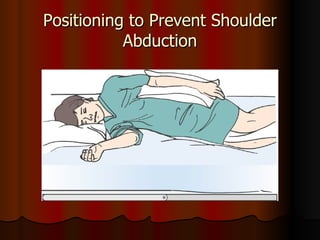
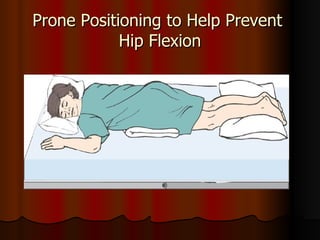
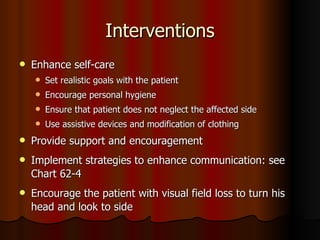
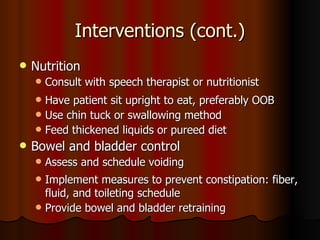
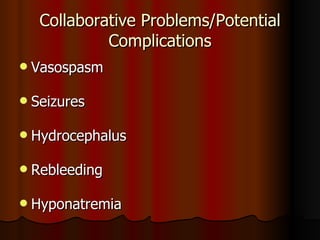
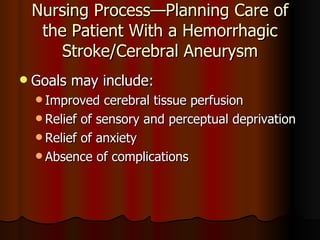
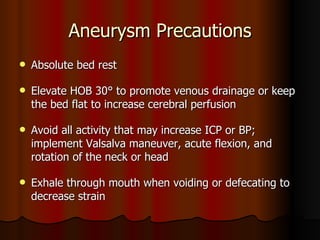
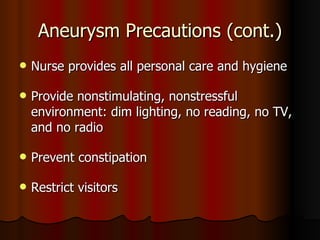
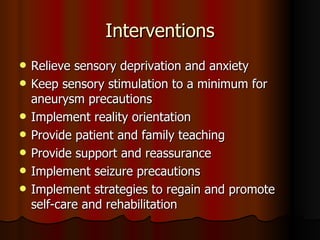
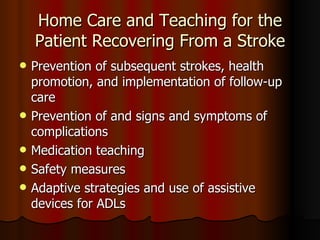
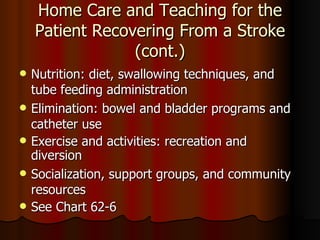
3) Nursing interventions are aimed at improving mobility, self-care, communication and preventing complications during recovery from stroke.