1) Encephalitis is an acute inflammation of the brain that is usually caused by a viral infection. Children, the elderly, and those with weak immune systems are most at risk.
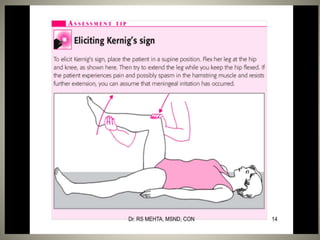
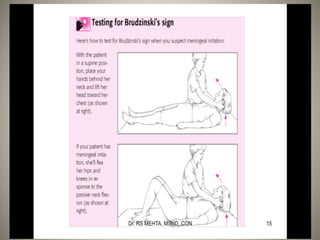
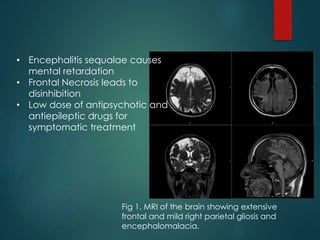
2) Diagnosis involves imaging tests like MRI and CT scans to view brain inflammation, as well as tests of cerebrospinal fluid and blood to identify potential viral causes.
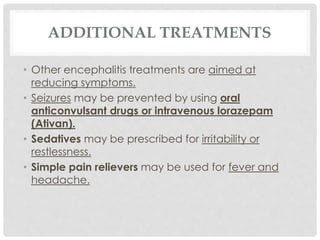
3) Treatment depends on the severity and cause of the inflammation. Supportive care aims to help the body fight infection, while antiviral drugs may be given if a viral cause is identified.

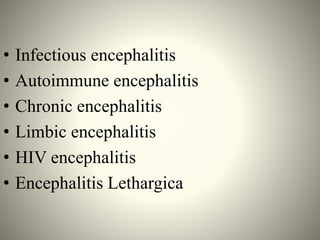

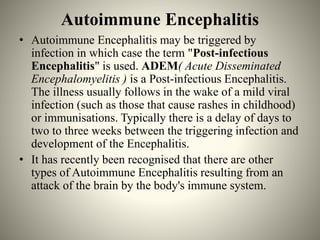
![• Some of the known types of Autoimmune
Encephalitis are:
o Acute Disseminated Encephalomyelitis (ADEM)
o NMDA Receptor associated Encephalitis [N-methyl
D-aspartate (NMDA) ]
o Hashimoto’s Encephalopathy
o Rasmussen Encephalitis](https://image.slidesharecdn.com/encephalitiscia3-151011085926-lva1-app6892/85/Encephalitis-12-320.jpg)