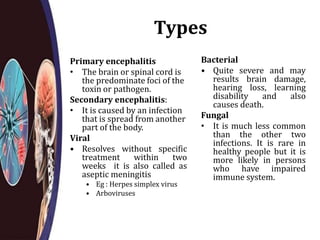
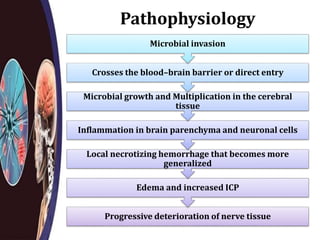
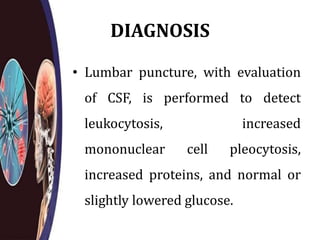
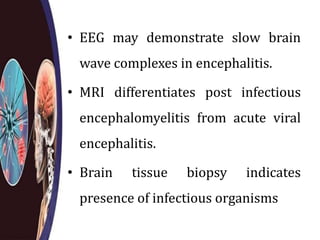
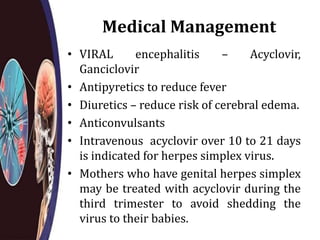
Encephalitis is an inflammation of the brain that is commonly caused by viral infections. It can cause symptoms like fever, headache, confusion, seizures, and neurological deficits as the brain tissue deteriorates. Diagnosis involves lumbar puncture to analyze CSF for signs of inflammation and PCR or antibody tests to identify the specific virus. Treatment focuses on managing symptoms, reducing fever and swelling, and using antiviral medications for viral causes. Nursing care involves frequent monitoring, preventing complications, managing aberrant behaviors, and providing supportive care and patient education.