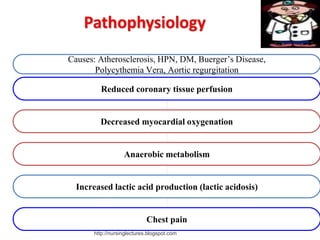
1. Angina pectoris is a clinical syndrome characterized by episodes of chest pain or pressure resulting from inadequate blood supply to the heart muscle.
2. Risk factors for angina include age over 55 for men or 65 for women, smoking, diabetes, high cholesterol, high blood pressure, obesity, physical inactivity, and family history of early heart disease.
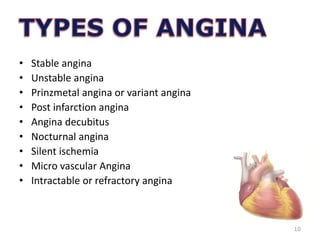
3. There are several types of angina including stable angina brought on by exertion, unstable angina occurring at rest or with minimal exertion, and Prinzmetal or variant angina occurring during rest especially between midnight and dawn.

![• Quality [crushing, squeezing, pressing, burning,
strangling, tight, stabbing]
• Onset [gradual or sudden,usually during activity]
• Duration [3-5 minutes, with a range of 2-15mts
• Location [substernal or retrosternal]
17](https://image.slidesharecdn.com/anginapectoris-221105150258-0375821d/85/Angina-Pectoris-PPT-17-320.jpg)
![Radiation :
[left chest and
arm,neck,jaw,teeth,back,both shoulders,
elbows and wrists]
Associated symptoms:
[nausea,vomiting,dyspnea,& diaphoresis]
Provocation:
[exertion,activity,emotional stress,
extreme temperature, heavy meals]
18](https://image.slidesharecdn.com/anginapectoris-221105150258-0375821d/85/Angina-Pectoris-PPT-18-320.jpg)