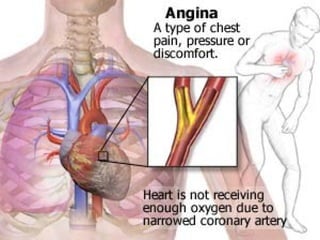
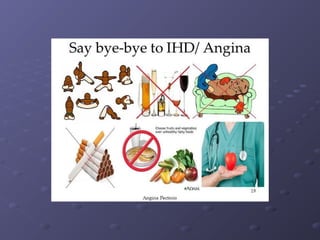
Angina pectoris is a clinical syndrome characterized by episodes of chest pain or pressure due to coronary artery disease. It occurs when myocardial oxygen demand exceeds supply. The document discusses the pathophysiology, risk factors, types, diagnosis and management of angina pectoris. Nursing interventions focus on treating episodes, reducing anxiety, and educating patients on prevention through lifestyle modifications and medication adherence. The goals are prompt relief of pain, decreased anxiety, avoidance of complications, and adherence to a self-care program.