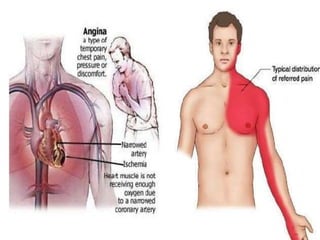
Angina pectoris is a clinical syndrome characterized by chest pain or pressure due to insufficient blood flow to the heart. It occurs when oxygen demand of the heart exceeds the oxygen supply. The main causes are atherosclerosis and coronary artery spasm. Diagnosis is made based on symptoms, ECG, stress test, and coronary angiography. Treatment involves lifestyle changes, medications to reduce oxygen demand or increase supply like nitroglycerin, beta blockers, and calcium channel blockers. The goal is to manage symptoms and prevent further heart issues.