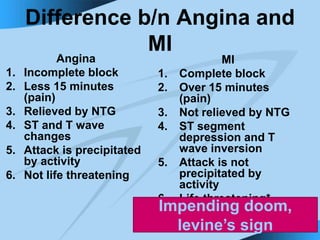
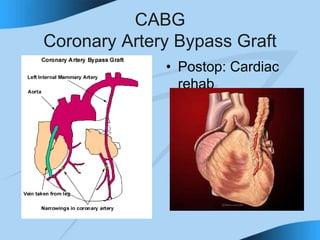
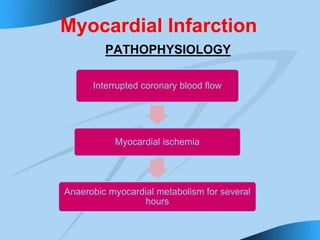
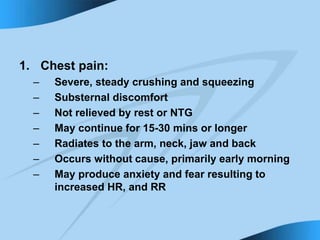
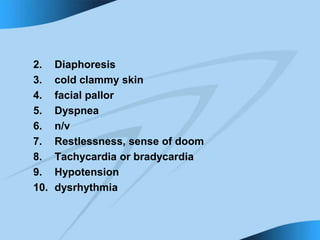
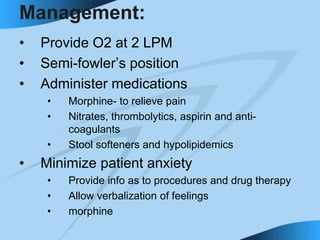
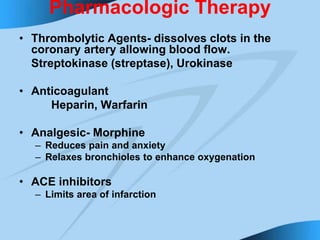
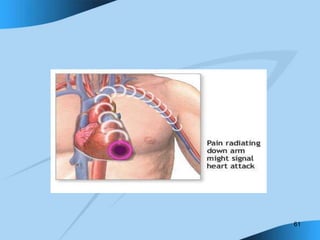
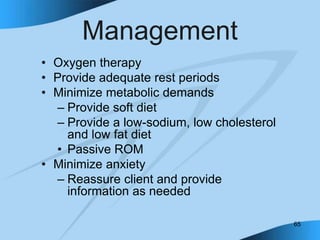
This document discusses angina pectoris and myocardial infarction (MI). It defines angina as chest pain due to inadequate blood supply to the heart muscle. The document describes the pathophysiology, types, symptoms, diagnostic tests, and management of angina and MI. It notes key differences between the two conditions including pain duration and relief with nitroglycerin. Treatment approaches discussed include medications, percutaneous coronary interventions like angioplasty, and coronary artery bypass surgery.