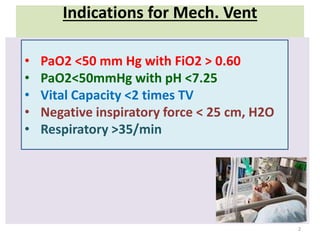
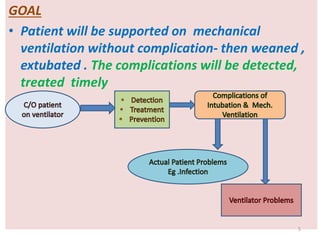
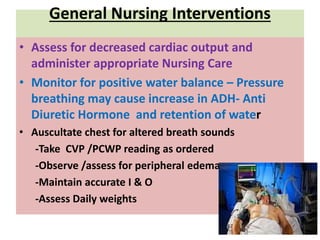
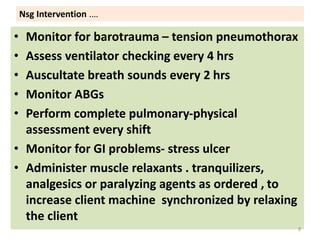
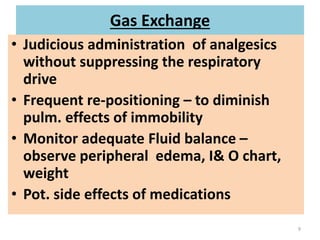
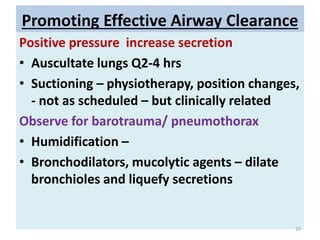
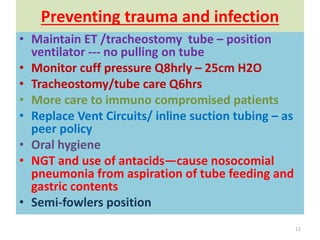
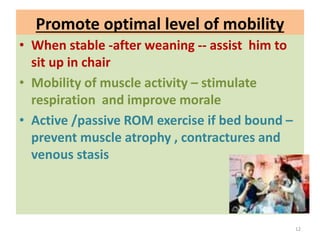
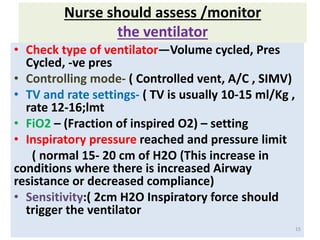
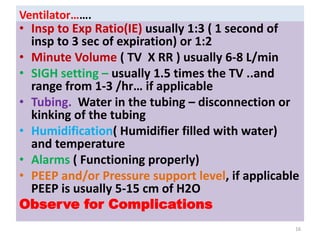
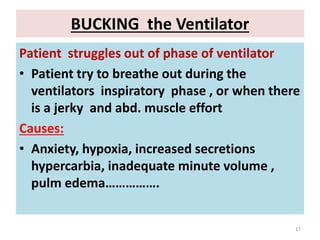
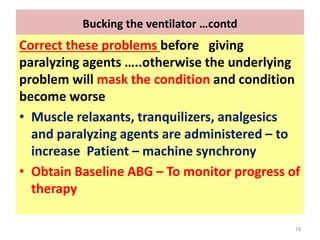
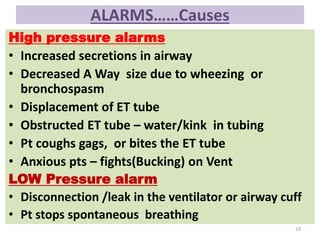
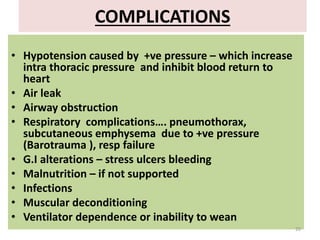
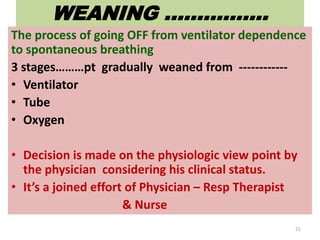
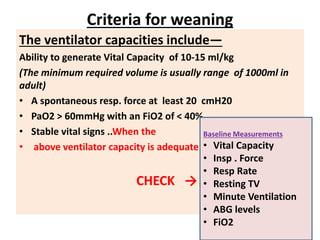
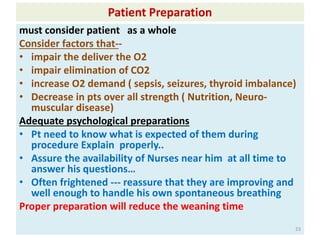
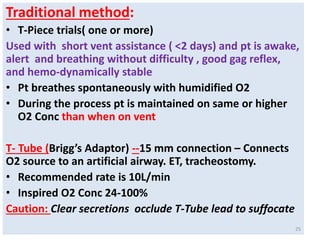
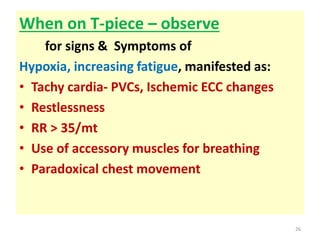
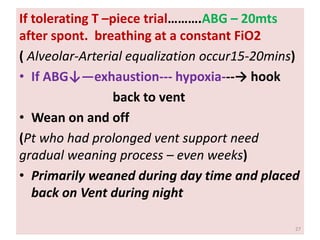
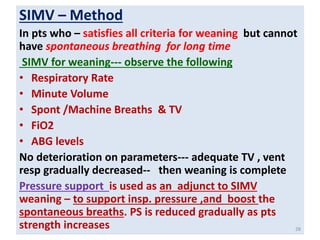
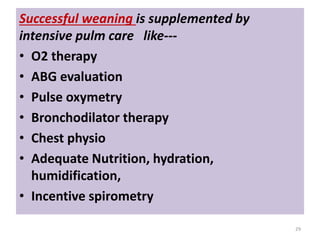
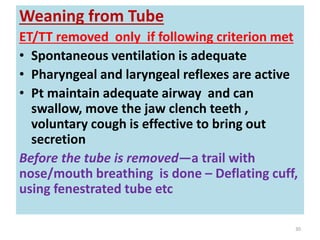
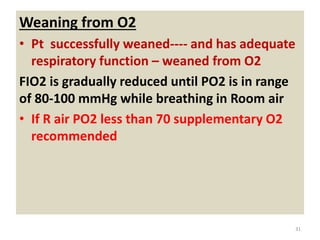
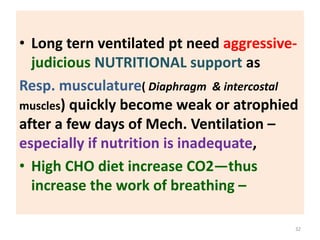
The document outlines the indications for mechanical ventilation, nursing interventions, and goals for patients on mechanical ventilation. It highlights the importance of continuous assessment of the patient and ventilator settings, monitoring complications, and preparing for the weaning process. Additionally, it discusses methods of weaning from the ventilator and the need for comprehensive patient care and support to ensure successful outcomes.