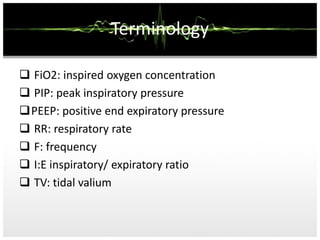
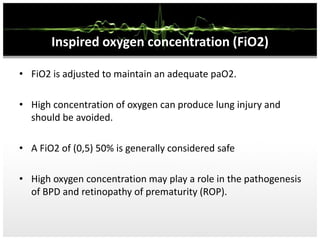
This document discusses mechanical ventilation. It begins by defining ventilation and the parts of a ventilator. It then covers the history of mechanical ventilation and describes various ventilator modes and settings such as PEEP, tidal volume, and inspiratory/expiratory ratio. The document outlines indications for ventilation and discusses monitoring ventilated patients. Key steps in ventilation like initiation, sedation, and weaning are summarized.