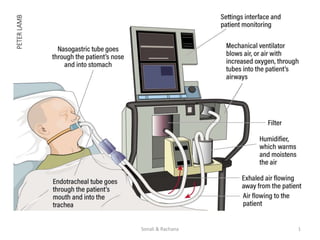
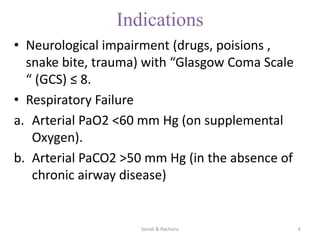
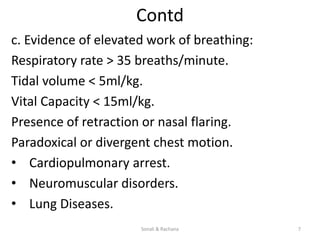
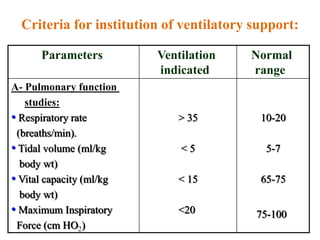
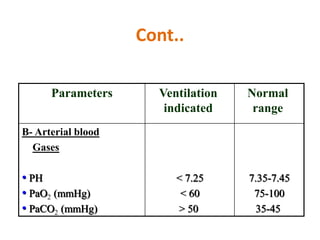
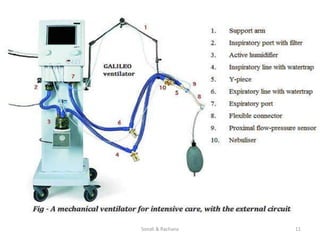
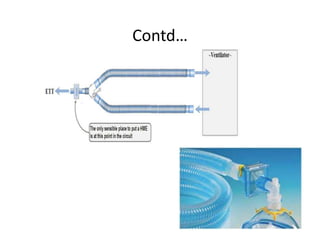
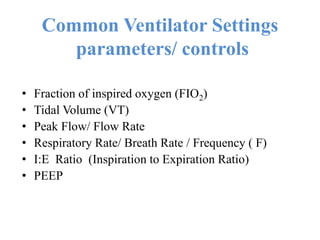
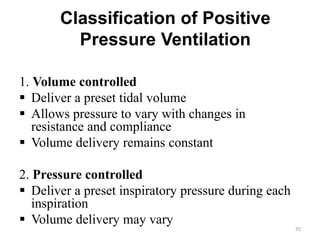
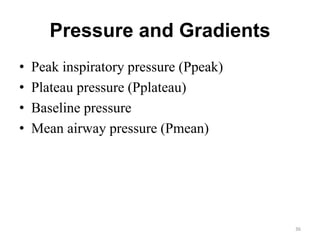
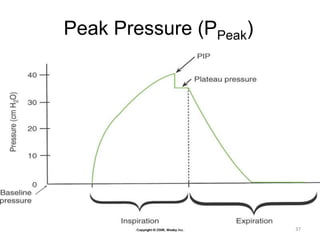
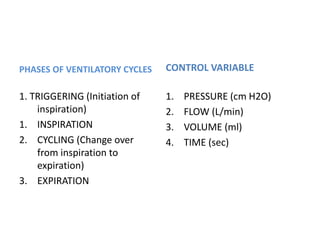
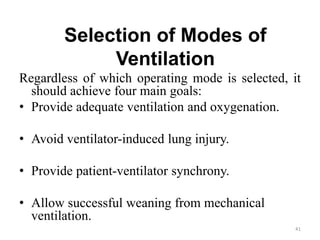
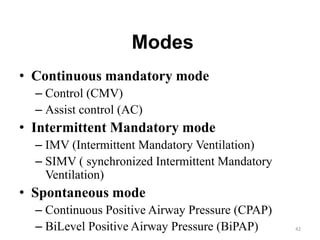
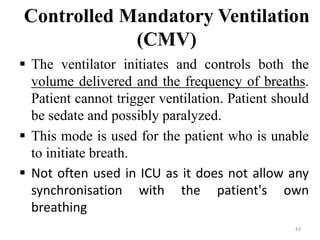
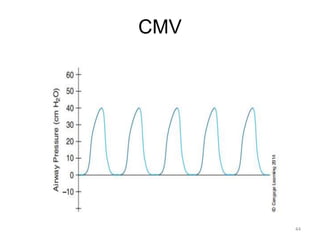
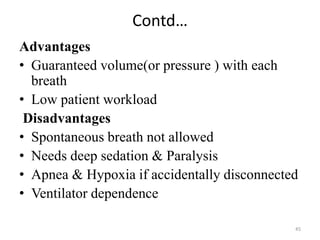
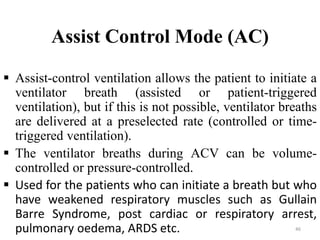
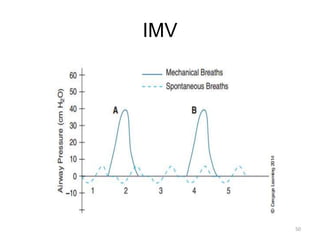
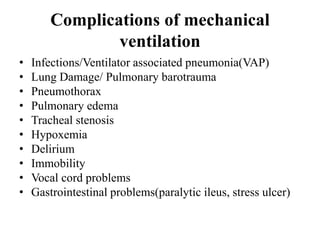
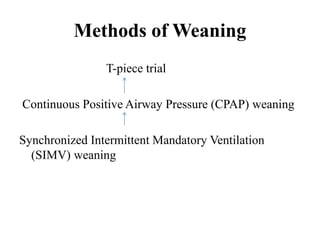
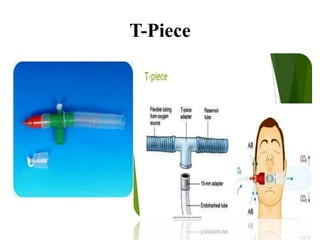
The document provides a comprehensive overview of mechanical ventilation, its goals, indications, and types of ventilators and settings. It explains the classification of ventilation modes, nursing management for patients on mechanical ventilation, and methods for weaning off the ventilator. Additionally, it discusses the role of the nurse in monitoring, patient care, and ensuring safe and effective use of mechanical ventilation.